Lumbar Degenerative Disc Disease (Lower Back)
Introduction:
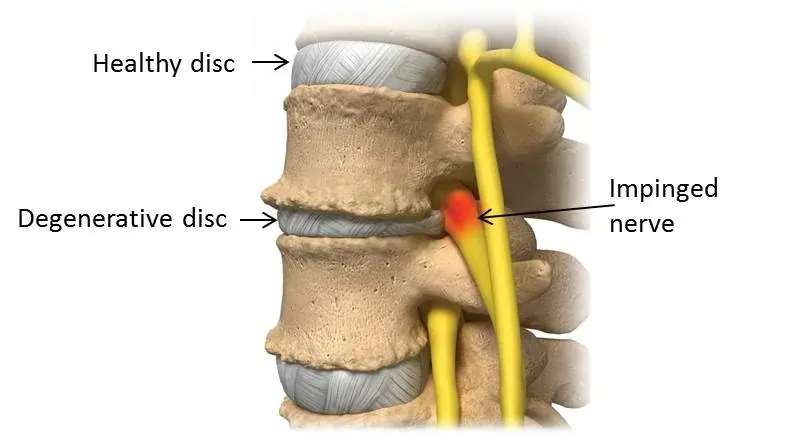
Lumbar Degenerative Disc Disease (DDD) is a condition where the intervertebral discs in the lower back gradually lose hydration and elasticity, leading to reduced cushioning between the vertebrae.
This can cause pain, stiffness, and reduced mobility. Although it’s a natural part of aging, factors like injury, obesity, and genetics can accelerate disc degeneration. Symptoms often include localized lower back pain that may worsen with movement or sitting for long periods.
Treatment typically involves physical therapy, pain management, and exercises to strengthen the back and core muscles.
Anatomy of Lumbar spine:
The lumbar spine, or lower back, is a complicated structure that serves a critical function in supporting the body and permitting mobility. Here’s a breakdown of its essential anatomical components:
The vertebrae:
L1–L5:
- The five big, strong vertebrae that make up the lumbar spine are designated L1 through L5.
- Because they sustain the weight of the upper body, these vertebrae are bigger than those in the cervical and thoracic areas.
- There are many processes, including a vertebral arch, and the vertebral body, which is the primary, block-like part of each vertebra.
Important Vertebral Elements:
Vertebral Body:
- Weight-bearing portion of the vertebra.
Vertebral Arch:
- The spinal cord is shielded by the vertebral arch.
- Made up of laminae and pedicles.
Processes:
- The backward-projecting spinous process serves as a point of attachment for ligaments and muscles.
- Transverse Processes: Act as attachment sites and project laterally.
- Movement between vertebrae is made possible by articular processes, often known as facet joints.
- Situated in the space between every spinal body.
- Serve as shock absorbers, supporting the spine when moving.
Consists of:
- The strong outer layer is called the Annulus Fibrosus.
- Nucleus Pulposus: The inner core that resembles gel.
Ligaments:
The spine is stabilized by strong connective tissues.
Important ligaments consist of:
- Running along the front of the vertebral bodies is the anterior longitudinal ligament.
- The ligament that runs along the rear of the vertebral bodies is called the posterior longitudinal ligament.
- Laminae are connected by the ligamentum flavum.
- The spinous processes are connected by the interspinous and supraspinous ligaments.
Muscles:
Support the lumbar spine and allow it to move.
Among the key muscle groups are:
- Paraspinal Muscles: The paraspinal muscles, which run down the spine, help with rotation and extension.
- Abdominal Muscles: Together with the back muscles, the abdominal muscles help to stabilize the spine.
- Quadratus Lumborum: The quadratus lumborum, which is involved in side bending, is situated on each side of the lumbar spine.
- Iliopsoas: Hip flexion depends on the iliopsoas, a collection of muscles that connect the lumbar vertebrae to the femur.
Nerves
- Cauda Equina and Spinal Cord: The cauda equina, a bundle of nerve roots, is where the spinal cord stops at the L1–L2 level.
- Intervertebral foramina are the entrances via which nerves leave the spinal canal.
- Spinal Nerves: The lower limbs and pelvis get sensation and motor function from the lumbar spinal nerves.
Curvature
Lordosis is a naturally occurring inward curvature of the lumbar spine.
Lumbar disc disease: What causes it?
Inflammation around the disc area and tension on the muscles supporting the spine are the usual causes of pain from degenerative disc disease.
Age-related wear and strain on a spinal disc causes degeneration, which can be Accelerate up by lifestyle, health, and accident variables as well as potentially by a hereditary susceptibility to musculoskeletal problems or joint pain. Rarely does a severe trauma, such an automobile collision, cause degenerative disc degeneration. The most likely cause is a low-energy disc damage.
What signs and Symptoms of lumbar disc disease are present?
The following are typical signs and symptoms of lumbar degenerative disc disease:
Symptoms might vary but common characteristics often include:
Constant, moderate low back ache. The most typical sign of a degenerative disc is painful pains at the location of the injured disc. The upper thighs, groin, and buttocks may all experience pain. This pain can be modest to severe and usually feels dull and achy.
Periodic flare-ups of pain. For a few days or weeks, back pain may get worse before subsiding to a more manageable level. As the spine eventually stabilizes and the disc continues to deteriorate, flare-ups occur. Severe and abrupt flare-ups of pain might impair movement for a short time.
Local tenderness. The lower back region around the deteriorated disc may be touch-sensitive. Muscle strain and inflammation around the degenerative disc are the causes of local pain.
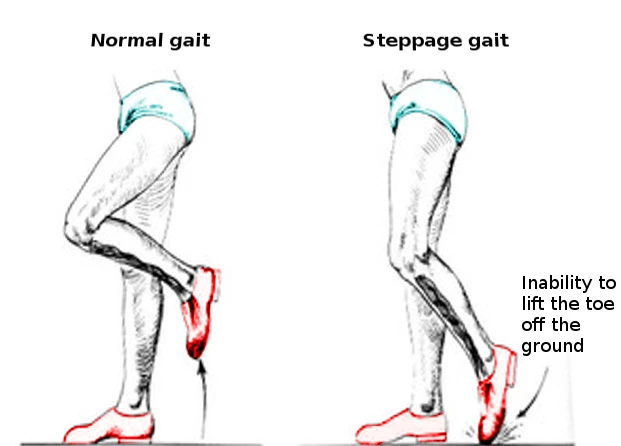
Leg pain. If the disc gap collapses sufficiently to squeeze a nerve root leaving the spine, neurological symptoms such as numbness, weakness, or acute, shooting sensations in the buttocks, hips, and/or back of the leg may be experienced. Lumbar degenerative disc degeneration often does not cause leg pain that extends below the knee.
Giving out symptoms. As the disc weakens, there may be a sudden sensation of weakness or instability, giving the impression that the lower back may “give out” with abrupt movements.
The Impact of Positions and Movements on Lumbar Degenerative Disc Pain:
Usually, particular postures, positions, and motions will make pain seem better or worse, including:
Pain when sitting. Long-term sitting frequently results in increased lower back pain and stiffness until you get up or move positions. It is often well tolerated to sit in a supported, reclining position.
Increased pain when twisting or bending. Intense, localized pain around the disc can result from twisting the spine and from bending forward, backward, and side to side.
Alleviation of pain with walking or posture changes. Pressure is transferred from the discs to the muscles and joints as the spine shifts positions. Regularly shifting postures, switching between sitting and standing, or going for little walks can all help reduce pain and ease stiffness.
How is lumbar disk disease diagnosed?
To guarantee an accurate diagnosis, our clinic integrates cutting-edge testing equipment with our knowledge. The diagnostic procedure consists of:
Medical history. Your symptoms, their intensity, and any previous therapies you have tried are all things the doctor asks you.
Physical assessment. You are closely inspected for pain, balance issues, and mobility limits. The doctor checks for neurological damage throughout the examination, such as loss of reflexes, muscular weakness, or loss of feeling.
Diagnostic tests.
X-ray. This test creates pictures of inside organs, bones, and tissues on film using invisible electromagnetic energy beams.
MRI. This process creates fine-grained pictures of the body’s organs and structures without the need for X-rays by combining radio frequencies, big magnets, and a computer.
Myelogramm. To make the structure readily apparent on X-rays, dye is injected into the spinal canal.
CT scan. This imaging technique creates fine-grained pictures of any area of the body, including the bones, muscles, fat, and organs, using X-rays and computer technology. CT scans provide greater information than ordinary X-rays.
EMG stands for electromyography. This test gauges how the muscles react electrically when they are stimulated by a nerve. This examination looks for any related nerve injury.
Discogram. In this process, a needle is guided by X-rays and inserted into the disc.
Lumbar Degenerative Disc Disease Treatment:
Reducing pain, stabilizing the spine, and preserving or increasing mobility are the major goals of treatment for painful degenerative disc disease.
Physical therapy, pain management strategies, and other methods are often used to treat degenerative disc degeneration.
The following are frequently used in conjunction as first pain treatment techniques for degenerative disc pain:
Over-the-counter (OTC) pain medications
Common painkillers like aspirin (Bayer), ibuprofen (Advil), or naproxen (Aleve) help reduce inflammation, which is a contributing factor to pain, stiffness, and irritation of the nerve roots. Acetaminophen, also known as Tylenol, is a painkiller that blocks the brain’s ability to perceive pain.
Prescription drugs for pain relief
Muscle relaxants or narcotic painkillers may be used to treat severe pain that is not alleviated by over-the-counter drugs. Intense, acute pain that is not anticipated to persist longer than a few days or weeks is frequently treated with these drugs. These drugs must be taken carefully and by the prescription doctor’s recommendations since they have the potential to become addictive and have major addictive effects.
Ice and heat
Heat therapy for the lower back increases circulation, which eases stress and muscular spasms while increasing the range of motion. Ice packs can dull minor pain and minimize inflammation. Applying heat before exercise can help relax the muscles, while applying cold after exercise can help reduce inflammation.
Manual manipulation
Manual manipulation is a common pain treatment technique for low back pain and is frequently linked to chiropractic care. In order to relieve tension in the muscles and joints, practitioners apply pressure and force to the hips, back, and other places using their hands. It has been shown that manual manipulation can effectively reduce pain in the short term and can even be just as effective as medicine in some situations.
Massage therapy
Massage treatment helps ease pain and strain on the spine by decreasing low back muscular tension and spasms. Furthermore, massage treatment helps increase circulation, giving stiff muscles oxygen and nutrients that promote recovery.
Epidural steroid injections (ESIs)
Both inflammation and pain signals can be decreased by administering a steroid injection in the area around the spine. In order to relieve pain during exercise and rehabilitation, a physical therapy program may be combined with a steroid injection. An epidural steroid injection can reduce pain for a few weeks to a year if it works.
Physical Therapy for Lumbar degenerative disc disease:
To support the maintenance of good spinal mobility, physical therapy is frequently recommended or prescribed. A comprehensive low-back workout regimen needs to have a mix of the following:
Physical therapy and exercise
Stretching techniques for strengthening, hips, pelvis, and lower back muscles. Low back pain is exacerbated by tightness in these muscles, which puts additional strain on the lumbar spine. Strengthening activities strengthen the muscles in the abdomen and lower back to help support the spine and maintain good posture. A personalized physical therapy program, dynamic lumbar stabilization, tai chi, stabilization other forms of exercise may be part of a strengthening regimen.
Low-impact aerobic exercise raises the heart rate and improves circulation while also delivering nutrients and oxygen required for tissue regeneration. Walking, swimming, water aerobics, stationary bike, and elliptical running are a few forms of cardiovascular exercise that are easy on the spine.
Exercises for Lumbar degenerative disc disease:
Knee to Chest
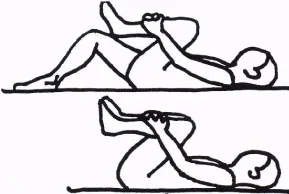
Pull your knees gently to your chest while lying on your back, hold for a second, and then release, repeating the action in a pulsating fashion for 20 seconds at a time, releasing, and repeating up to five times. You may practice the entire routine up to three times a day.
Hip flexor stretches

The front of your hip will be stretched out as a result. Perform the stretch five times for each leg while in a low lunge stance and holding it for 30 seconds. Do as much as five sets a day.
Piriformis stretches

It could be challenging if your pain is severe, but this is a powerful stretch for your hips and glutes. Lower your buttocks softly to the floor while forming a figure-four with one leg on top of the other thigh. Hold for 20 seconds. Be cautious not to push through any pain while performing each leg five times, up to five times a day.
Hamstring stretches

Place a stretch band around your foot and lie on your back with one leg bent and one in the air. Hold for 30 seconds, then do this five times with each leg, up to three times a day.
Bridging

While lying on your back with both legs bent and your feet flat on the ground, gently lift your buttocks 4 to 6 inches off the ground, hold them there for 5 seconds, and then lower yourself down to the beginning position 5 to 10 times.
Back Extensions

Extend and gently press up your lower back while lying on your stomach. Repeat the movement ten times for three sets, up to three times a day, without holding it. You may modify this stretch by resting on your forearms or just not stretching it all the way if it seems too intense.
Pelvic tilts
Place your feet on the floor and both knees bent while lying on your back.
Lower your back gently to the floor, hold it there for 5 to 10 seconds, and then release it.
Repeat five to ten times.
Foam rolling
One of the best exercises for lower back pain is foam rolling. Maintaining your posterior on the floor, place the foam roller beneath your mid-back and slowly stretch your spine rearward. Repeat as required throughout the day, holding for 30 seconds at a time.
Cat/Cow

Begin by bending and flattening your mid-back 20 times on your hands and knees. Do this as much as three times per day. This is a fantastic way to begin your day.
Child’s Pose

A patient stretch that can be a great option if your pain is severe is to start with your knees apart and your toes touching, After that, sit your butt back towards your heels and reach out in front of yourself. Hold this position for 30 seconds, repeat 5 times for one set, and do up to 3 sets per day.
Surgical Intervention for Lumbar degenerative disc disease:
Additional diagnostic testing can be required if nonoperative therapy for lumbar DDD is ineffective. A CT scan, MRI, myelogram, and potential discography are among the possible tests. Surgery can be required if your surgeon finds that one or more intervertebral discs are injured and producing pain or other symptoms (such as muscular weakness). A discectomy, or removal of the injured disc, and interbody fusion, or joining the vertebrae above and below the disc space, are likely to be part of the surgical operation.
Minimally invasive methods are used for several treatments, which can hasten your recuperation. Naturally, your surgeon will thoroughly explain the suggested course of action, along with the advantages and risks, if surgery is required.
Risk Factors for Degenerative Disc Disease:
The spinal discs may be impacted by lifestyle choices that affect general health. Degenerative disc disease risk factors include:
- A family history of musculoskeletal problems or back pain.
- Excessive low back strain caused by labor-intensive employment, sports, or regular heavy lifting.
- Lumbar spinal disc strain is caused by extended sitting and/or bad posture.
- Weak core muscles result in a lack of support for the discs.
- Being overweight.
- Smoking or consuming nicotine in any way.
What are the potential consequences of lumbar disc disease?
Back and leg pain that interferes with everyday activities might be a symptom of lumbar disc disease. It may result in numbness or paralysis in the legs as well as issues controlling the bowels and bladder.
How can lumbar disc disease be avoided?
Lumbar disc disease can be prevented by maintaining a healthy weight, exercising often, and adopting proper posture. Smoking should be avoided as it raises the risk of disc herniation.
How to Live with Lumbar Disc Disease?
Patience is necessary for conservative treatment. However, according to your treatment plan might lessen the likelihood of disc degeneration or chronic back pain. Both surgery and conservative methods may not show results right away.
Conclusion
Even though lumbar degenerative disc degeneration is a normal aspect of aging, low back pain is not something you have to put up with. We can assist you in getting back to living an active, pain-free, and healthy life. For the majority of patients, nonsurgical methods are used to achieve this. Even if surgery is required, you can be confident that we will provide you with the finest care possible and go over the advantages and disadvantages of the treatment.
Our medical staff is deeply committed to patient education in addition to therapy. We can assist you in removing risk factors and establishing lifelong spine-healthy behaviors by assisting you in understanding the origin of your illness. Our medical team will provide you with good information to help you stay healthy, reduce risk factors, and Get better while you are in our care.
FAQs
Is it possible to cure degenerative disc disease?
No. Although the structural alterations associated with DDD will not go away, therapy may eventually alleviate the symptoms, such as back pain.
How is lumbar degenerative disc disease treated?
From bothersome to incapacitating, this pain might vary. Daily activities, sports, accidents, and the disc’s gradual drying up can all contribute to the disease. In addition to nonsurgical therapies including acupuncture, back graces, and pain management, treatment options include disc replacement and various surgical procedures.
Does a degenerative disc benefit from walking?
DDD symptoms can also be controlled by keeping a healthy weight and avoiding activities that overstress your back. Frequent exercise can also be beneficial, particularly low-impact exercises like swimming or walking.
Is degeneration of the lumbar disc serious?
In extreme circumstances, this illness can prevent some individuals from leading regular, healthy lives and can cause excruciating agony. Remember that a certain degree of spine deterioration is natural with aging.
Is degenerative disc disease a condition I can live with?
Age-related disc wear and tear is the cause of degenerative disc disease. Many people are unaware that the pain associated with degenerative disc degeneration may usually be controlled with self-care and some nonsurgical therapies. Pain from degenerative disc degeneration does not usually get worse with age.
Which stage of degenerative disc disease is the last one?
The collapse stage is the last stage of degenerative disc disease. The vertebrae fall at this advanced stage due to severe degradation of the intervertebral discs. The spine loses height as a result, and significant chronic pain and impairment may follow.
References
- Khan, H., MD. (n.d.). Causes and risk factors of lumbar degenerative disc disease. Spine-health. https://www.spine-health.com/conditions/degenerative-disc-disease/causes-and-risk-factors-lumbar-degenerative-disc-disease
- Lumbar disk disease (Herniated disk). (2024, March 21). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/lumbar-disc-disease-herniated-disc
- Explaining spinal disorders: Lumbar degenerative disc disease. (n.d.). https://www.coloradospineinstitute.com/conditions/lumbar-degenerative-disc-disease/