Systemic Juvenile Idiopathic Arthritis
Systemic Juvenile Idiopathic Arthritis: What is It?
Systemic Juvenile Idiopathic Arthritis (sJIA) is a rare but severe form of juvenile arthritis that affects children. Unlike other types, it involves joint inflammation and systemic symptoms such as high fevers, rash, and inflammation of internal organs.
Flare-ups of arthritis, fever, and rash in children characterize systemic juvenile idiopathic arthritis (systemic JIA), which could also include issues with the heart, lungs, and blood, as well as enlarged glands.
Treatments can alleviate symptoms, allowing kids to lead active, fulfilling lives. The symptoms can go away for a while (called remission). Some children have a lasting cure for the disease.
Systemic Juvenile Idiopathic Arthritis: What Causes It?
It’s unclear exactly What causes SJIA. It is often believed that a kid has a genetic predisposition and that an environmental factor causes the condition to manifest. “Idiopathic” describes an unidentified cause or trigger. Researchers are learning more about SJIA and how it is different from other forms of juvenile arthritis, but there are still unanswered questions.
Innate and adaptive immunity are the two forms of immunity the body possesses. The initial line of defense against infection is the innate immune system, which is active from birth. The adaptive immune system changes during an individual’s lifetime. Its function is to detect and destroy bacteria and viruses that evade the innate immune system.
The majority of JIA types arise when healthy cells and tissues are attacked by an overactive adaptive immune system. We refer to these conditions as autoimmune illnesses. According to research, SJIA is unique. The innate immune system may be triggered by this autoinflammatory state even in the absence of an infection. Researchers believe that SJIA is an autoinflammatory illness because of several variables.
For starters, unlike many children with other types of JIA, children with SJIA typically do not have autoantibodies in their blood. When the adaptive immune system is hyperactive, autoantibodies are produced. Additionally, two inflammatory proteins (cytokines) known as interleukin-1 (IL-1) and interleukin-6 (IL-6) are elevated in the blood of children with SJIA. These proteins are thought to promote inflammation in SJIA and are known to cause inflammation in other autoinflammatory disorders.
What are the signs and symptoms of systemic juvenile idiopathic arthritis?
Children who suffer from systemic JIA have:
- Arthritis that lasts longer than six weeks in one or more joints, commonly the ankles, knees, and wrists.
- Elevated temperature that often lasts longer than two weeks.
- A rash.
They could also have:
- Decreased red blood cell count, or anemia.
- An enlarged lymph node, spleen, or liver.
- Joint injury.
- Inflammation of either the lung or heart lining.
Fever
One of the initial symptoms of SJIA is a high, recurrent fever, frequently accompanied by a rash. A youngster with a fever often exhibits a pattern whereby their temperature rises to 103 degrees or higher, usually in the evening, and then falls off in a few hours. Studies have revealed that the pattern can vary, even though one of the criteria for identifying SJIA is a daily, climbing fever, usually in the evening. Sometimes the fever happens twice a day or in the morning, and sometimes it lasts all day. However, nearly all children with untreated SJIA eventually experience the usual pattern of a daily fever that eventually subsides.
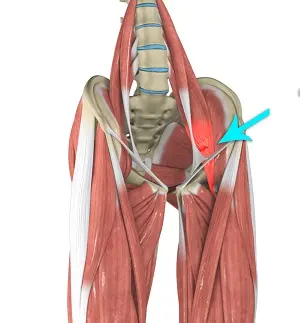
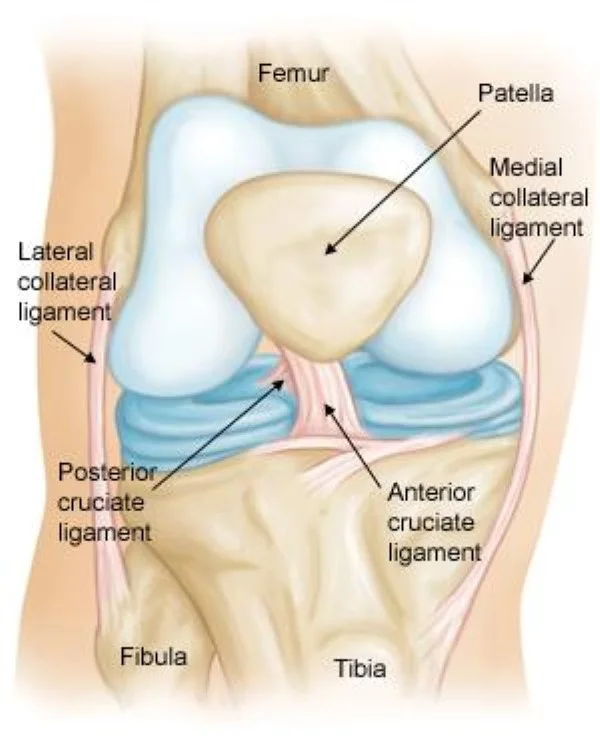
Joint Pain
The second most prevalent early symptom of SJIA is arthritis. In the morning and following a nap or extended periods of immobility, the symptoms of joint swelling, discomfort, stiffness, and warmth are more severe. Joint issues, in contrast to other types of pediatric arthritis, might appear weeks or even months after systemic symptoms.
Children, especially very young ones, frequently don’t complain of joint discomfort with SJIA, but parents usually detect the development of arthritis when a kid starts to limp, feels stiff in the morning, or suddenly becomes less active. The knees, wrists, and ankles are the most often affected joints, however occasionally just one is. Children with SJIA may also develop arthritis in the hip, jaw, and spine (around the neck).
Symptoms of SJIA might sometimes appear and go away. Flares are times when symptoms intensify and there is a lot of inflammation. Days or months may pass during a flare.
A rash.
Depending on the child’s skin tone, a flat, pale, or pink rash typically develops on the trunk, arms, or legs, however, it can spread to other areas of the body. The rash is often not irritating, though it can be. It is linked to temperature rises and usually lasts a few minutes to a few hours.
Diagnosis of Systemic Juvenile Idiopathic Arthritis:
High fever for at least two weeks and arthritis (pain and inflammation in one or more joints) in one or more joints for at least six weeks are prerequisites for a diagnosis of SJIA, according to the diagnostic criteria for the condition created by the International League of Associations for Rheumatology (ILAR). Thankfully, pediatric rheumatologists are adept at recognizing SJIA and managing the occasionally contradictory difficulties associated with the diagnosis.
Since there are no particular tests for SJIA, clinicians must use their knowledge and experience in addition to the child’s medical history and a thorough physical examination to diagnose the condition. In addition to ruling out illnesses that cause similar symptoms, laboratory and other investigations can assist confirm a diagnosis of SJIA.
SJIA testing
Medical Background:
To learn about prior diseases, current medications, and specifics of present symptoms, such as how long a kid has had them, doctors take a patient’s medical history. It is easier to rule out infections and other issues that might momentarily impact the joints when you know how long the symptoms of SJIA have been present.
Physical Examination:
Even if they don’t exhibit any overt joint complaints, children with chronic fever and rash should have a comprehensive musculoskeletal examination. During the physical examination, physicians search for signs of pain, warmth, edema, and decreased range of motion, particularly in the jaw and neck as well as the knees, wrists, ankles, and hips, which are the joints most frequently impacted by SJIA.
Doctors measure limb length and overall growth because joint inflammation can cause the growth centers in bones to become shorter than usual and perhaps unequal from side to side in some youngsters. Additionally, doctors could check for enlarged lymph nodes in the neck, behind the ears, or in the groin.
Blood examinations:
The following are a few of the most popular blood tests for suspected cases:
ESR, or erythrocyte sedimentation rate. The pace at which your red blood cells sink to the bottom of a blood tube is known as the sedimentation rate. Inflammation may be indicated by an increased rate. The main purpose of measuring the ESR is to assess the level of inflammation.
C-reactive protein. Although it uses a different scale than the ESR, this blood test also gauges the body’s overall degree of inflammation.
Antinuclear antibody. The immune systems of patients with several autoimmune disorders, such as arthritis, frequently create proteins called antinuclear antibodies. They indicate a higher risk of inflammation of the eyes.
Rheumatoid factor. This antibody may indicate a greater risk of arthritis-related damage and is infrequently detected in the blood of children with juvenile idiopathic arthritis.
CCP, or cyclic citrullinated peptide. Similar to the rheumatoid factor, children with juvenile idiopathic arthritis may have the CCP antibody in their blood, which may be a sign of increased damage risk.
These blood tests will not reveal any notable abnormalities in a large number of children with juvenile idiopathic arthritis.
Imaging scans:
To rule out further problems such as fractures, tumors, infections, or congenital anomalies, X-rays or magnetic resonance imaging may be performed.
Following the diagnosis, imaging may also be done sometimes to track bone growth and identify joint deterioration.
What is the treatment for juvenile systemic idiopathic arthritis?
SJIA has no known cure. Treatment aims to address the underlying inflammation and lessen the symptoms.
Children with juvenile idiopathic arthritis are treated with drugs that reduce pain, enhance function, and reduce the risk of joint deterioration.
Typical drugs consist of:
NSAIDs, or nonsteroidal anti-inflammatory medications. These drugs, which include naproxen sodium (Aleve) and ibuprofen (Advil, Motrin, and others), lessen pain and swelling. An unsettled stomach and, less frequently, liver and kidney issues are side effects.
DMARDs, or disease-modifying antirheumatic medications. When NSAIDs alone are unable to reduce joint pain and swelling symptoms or when there is a significant chance of further harm, doctors turn to these drugs.
DMARDs are used to halt the progression of juvenile idiopathic arthritis and can be given in conjunction with NSAIDs. Methotrexate is the most often prescribed DMARD for kids (Trexall, Xatmep, etc.). Methotrexate side effects can include liver issues, low blood counts, nausea, and a slightly elevated risk of infection.
Biological substances. TNF blockers, such as etanercept (Enbrel, Erelzi, Eticovo), adalimumab (Humira), golimumab (Simponi), and infliximab (Remicade, Inflectra, and others), are part of this more recent family of medications, also referred to as biologic response modifiers. These drugs can help avoid joint injury and lower systemic inflammation. They can be taken alongside other drugs, including DMARDs.
Other biologics, such as abatacept (Orencia), rituximab (Rituxan, Truxima, Ruxience), anakinra (Kineret), and tocilizumab (Actemra), suppress the immune system in slightly different ways. Every biologic has the potential to raise infection risk.
Corticosteroids. Until another drug takes effect, symptoms may be managed with medications like prednisone. When inflammation occurs outside of the joints, like in the sac surrounding the heart, they are also utilized to treat it. Generally speaking, these medications should be taken for as little time as possible because they can disrupt normal growth and make a person more vulnerable to infection.
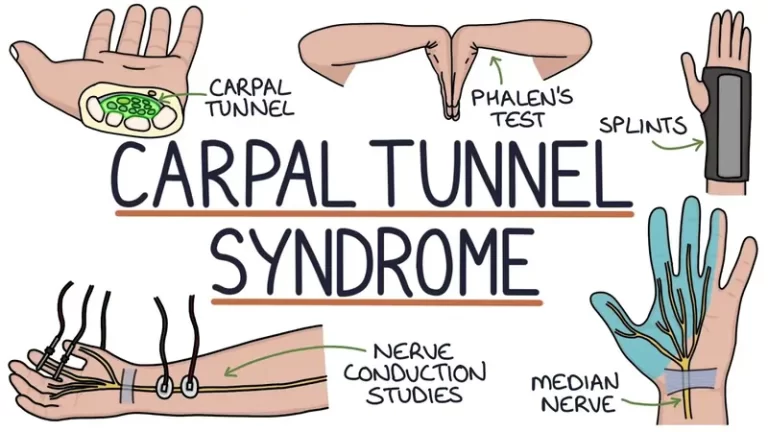
Therapies
To maintain range of motion, muscular tone, and joint flexibility, your doctor might advise your child to see a physical therapist.
Additional suggestions about the ideal exercises and safety gear for your child may come from an occupational therapist or physical therapist.
To help protect joints and maintain a good functional position, a physical or occupational therapist could also advise your kid to utilize splints or joint supports.
Surgery
Surgery may be required to enhance joint function in extremely severe cases.
What Other Issues Might Occur?
Rarely, children with JIA may develop macrophage activation syndrome, a potentially fatal condition. It occurs when the body’s organs are harmed by an overactive immune system. Seizures, hearing loss, severe diarrhea, and confusion might result from it.
Treatment for macrophage activation syndrome must begin immediately:
If your child appears extremely tired or has severe diarrhea bleeding, confusion, or seizures, you should take them to the emergency hospital.
How Can Parents Assist?
Although systemic JIA is typically a lifelong condition, some treatments can reduce discomfort, encourage physical activity in children, and stop long-term joint degeneration.
To assist your child:
- Make sure your child takes all of their medications as prescribed.
- Work with the physical therapist to develop a regular exercise routine. This will keep your child’s muscles strong and flexible.
- With your child, learn as much as you can about systemic JIA.
FAQs
What causes juvenile systemic idiopathic arthritis?
The innate immune system, which is the portion of the immune system that is present from birth, is hyperactive in children with sJIA. This causes inflammation throughout the body, including in the joints. Although the exact etiology of this overactivity is unknown, a mix of environmental and hereditary factors is most likely to blame.
What is the severity of idiopathic arthritis in children?
Inflammation that restricts movement can impact a child’s physical and mental development, and because JIA mostly affects the joints, it can impede bone formation. The entire body may be impacted by autoimmune disease, and in rare instances, JIA may result in issues with other organs.
What criteria are used to diagnose juvenile systemic idiopathic arthritis?
A child must be under 16 years old, have “arthritis in one or more joints with or preceded by the fever of at least 2 weeks’ duration that is documented to be daily (“quotidian”) for at least 3 days, and be accompanied by one or more of the following symptoms to meet the criteria for systemic juvenile idiopathic arthritis (sJIA).”
What symptoms appear initially in children with arthritis?
The initial symptoms of juvenile arthritis (JIA) are warmth, stiffness, edema, and joint discomfort. Usually, these symptoms are worse in the morning, after a lengthy period of sitting, or after a nap.
Is it possible to cure juvenile arthritis?
While certain forms of juvenile arthritis may go away in youth, others may continue into maturity. Sometimes a child’s joint symptoms go away and they enter remission, but years later, the disease flares up again.
In what ways might JIA be avoided?
Exercise, including physical and occupational therapy, can help maintain muscle tone, lessen pain, increase mobility (the capacity to move), and avoid long-term issues. Splints or braces may occasionally be used by a provider to help safeguard your child’s developing joints.
References
- Systemic juvenile idiopathic arthritis (for parents). (n.d.). https://kidshealth.org/en/parents/systemic-jia.html
- Systemic Juvenile Idiopathic arthritis | Arthritis Foundation. (n.d.). https://www.arthritis.org/diseases/systemic-juvenile-idiopathic-arthritis
- Systemic Juvenile idiopathic arthritis | HSS Pediatrics. (n.d.). Hospital for Special Surgery. https://www.hss.edu/conditions_systemic-juvenile-idiopathic-arthritis.asp
- Juvenile idiopathic arthritis – Diagnosis and treatment – Mayo Clinic. (n.d.). https://www.mayoclinic.org/diseases-conditions/juvenile-idiopathic-arthritis/diagnosis-treatment/drc-20374088