Tietze Syndrome
Tietze Syndrome: what is it?
Tietze syndrome is a rare, benign condition characterized by inflammation of the costal cartilage, typically where the upper ribs meet the sternum (breastbone). It causes localized chest pain, tenderness, and swelling, often mimicking heart-related pain.
Where your sternum (breastbone) joins your upper vertebrae (the first 10) is where the cartilage points (costal cartilage) are located. Cartilage is also present at the costochondral joints, which are the connections where these points join.
Although Tietze syndrome is more specific. Additionally, it is known for causing significant edema. The cause of Tietze syndrome is also known as costochondral junction syndrome. It doesn’t appear to be serious. With rest and painkillers, you can treat it at home.
Relevant anatomy
The main anatomical feature of Tietze syndrome is the inflammation of the cartilage at the costosternal junction, which results in severe chest pain and swelling. Tietze syndrome is characterized by localized pain, tenderness, and occasionally visible swelling at the costochondral joints, specifically the cartilage where the upper ribs (usually the second and third) connect to the sternum (breastbone).
- Affected area: While additional upper ribs may be impacted, the costochondral junction of the second and third ribs is the most frequently affected area.
- Inflammation: Inflammation of the costal cartilage at its attachment to the sternum is the main pathophysiology.
- Unilateral presentation: Only one side of the chest is often impacted by Tietze syndrome.
- Pain characteristics: Tietze syndrome pain can spread to the arms, shoulders, and neck and is frequently described as acute, hurting, or clutching.
Epidemiology
It is unknown how common Tietze syndrome is and how often it occurs. Geographical location, occupation, race, or biological sex don’t reveal anything about incidence rates. Males and females seem to be affected by this syndrome in roughly equal amounts. The syndrome affects people under 40 more often than it does people over 40. Although there have been documented examples, cases involving people 40 and older are rare.
Pathophysiology
The hallmark of Tietze syndrome is a small, painful, swollen lump that typically lacks erythema or a pustulation rub. About 70% of patients have the disease limited to one side, with the most common relationship being with the cartilage of either rib 2 or rib 3. However, the xiphisterna and sternoclavicular joints have also been found to be affected by this Tietze syndrome.
The idea that this syndrome process is inflammatory and could be a component of a more extensive seronegative pathology is still being discussed. Recurrences of Tietze syndrome are conceivable, but the symptoms usually go away on their own.
Sign and Symptoms
- The most noticeable symptom of Tietze syndrome is chest pain, which may develop gradually or suddenly.
- Some claim that when you’re motionless, it seems dull, but as you move or twist your upper body, it becomes acute and gripping. Exercise, sneezing, and coughing might exacerbate it. Usually on one side, you will feel it in the front and upper part of your chest. Additionally, it could radiate to your neck, shoulder, and arm.
- The other main sign of costochondral junction syndrome is localized edema. Somewhere in your upper sternum, usually at your second or third rib, you can see a little, swollen lump. In addition, it could appear red or discolored and feel warm. All of these are signs of inflammation. One characteristic of Tietze’s disease is swelling, which frequently goes away last.
Causes
Tietze syndrome is characterized by inflammation and irritation of the cartilage at that uncomfortable location in your rib cage. However, medical professionals are unsure of the reason for this and why it occurs in the specific manner that it does. Tietze syndrome differs from ordinary costochondritis in these ways.
- Traumatic injury. Tietze’s syndrome may be caused by an automobile accident, a fall, or an athletic injury that affects your upper rib cage. Perhaps this region’s soft tissues just respond to trauma differently.
- Microtrauma. Over time, minor but recurrent stress on your rib cage may cause a particular inflammatory response, such as intense coughing or repeated chest hits.
Risk Factor
If you have a persistent condition that weakens or irritates the cartilage in your rib cage, or if you are recuperating from another syndrome, you may be at a higher risk of developing Tietze’s disease. Among the examples are:
- Autoimmune diseases.
- Hereditary connective tissue diseases.
- Degenerative or inflammatory arthritis.
- Chronic chest infections.
- Chronic coughing or vomiting.
- Recent surgery in the area.
Diagnosis
When you present your chest pain to your doctor, they will first make sure it isn’t a heart attack. They will carefully go over your symptoms and check your chest after ruling that out. Imaging studies will be performed later to check for signs of injury and inflammation inside your chest. Once other potential causes of your symptoms have been checked out, medical professionals diagnose Tietze’s disease.
In addition to heart attacks, Tietze syndrome can resemble other heart and lung disorders. To rule out any further problems that might be more serious or require different treatment, you must see your doctor.
Tietze syndrome cannot be diagnosed with a single test. Your doctor will ask you to describe your symptoms and perform a physical examination to determine what’s causing them. To look for areas of pain and edema, they will most likely feel or apply pressure on your chest and ribs.
Investigation
Tests might include:
- Chest X-ray
- CT scan
- MRI
- Ultrasound
- Electrocardiogram (EKG)
- Biopsy
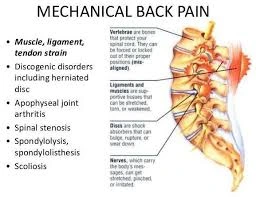
Differential Diagnosis
When acute chest pain first appears, it is important to think about a wide differential diagnosis because Tietze syndrome is identified by ruling out other possible causes. Because anterior chest wall pain that palpates at the osteochondral connections is a common symptom of both disorders, clinicians sometimes misdiagnose this condition as costochondritis. Multiple ribs, usually ribs two through five, are linked to costochondritis. Furthermore, there is no correlation between costochondritis and localized swelling over the affected joints.
Costochondritis will not show any notable results on ultrasound. Ultrasonography, on the other hand, actively visualizes edema and inflammation to diagnose Tietze syndrome. Performing a physical examination to check for obvious edema might also help make this diagnosis.
Exclude further conditions including acute coronary syndrome, hypertensive crisis, pleural infections or inflammatory processes, cancers, fractures related to chest trauma, rheumatoid or pyogenic arthritis, gastroesophageal reflux syndrome, or psychogenic disorders. Rib fractures, lupus, and fibromyalgia are among the other syndromes on the differential diagnostic list.
- Seronegative spondyloarthropathy
- Spondyloarthropathy(SA)
- Rheumatoid Arthritis(RA)
- Slipping Rib Syndrome
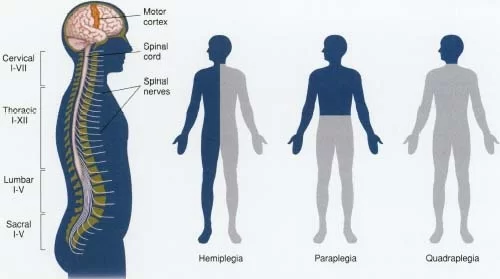
- Myelomalacia
- Early forms of soft tissue and bone cancers
- Chondrosarcoma of chondrocostal joints
- Costochondritis
- Chest or pulmonary tumors
- Metastases of breast, kidney, and prostate neoplasms
- Rib Fracture
Treatment
Your soft tissues require relaxation and time to heal from inflammation. Typically, medical professionals recommend just that. Pain and swelling can be reduced using over-the-counter pain medications. You shouldn’t have to miss work or school, but while you’re recovering, take it easy and stay away from strenuous activity. As you begin to feel better, you can progressively increase your level of activity.
After ten days, if you still feel that you need to take NSAIDs, speak with your doctor. Long-term use of these may result in adverse effects. At the site of irritation, they may administer a cortisone injection or advise you to switch to acetaminophen. Before their chests heal, some people may require treatment to halt coughing, sneezing, or vomiting. Discuss your recuperation with your provider.
Medical treatment
Conservative therapy is the cornerstone of treating Tietze syndrome, and patients are reassured that the syndrome will typically go away in a matter of weeks with no lasting effects. Months or even a year may pass while this condition persists. Rest and topical or oral anti-inflammatory and analgesic medications are the first-line treatments.
Given that inflammation is the primary cause, nonsteroidal drugs are usually more effective than acetaminophen or opioids. Clinically advise taking an anti-inflammatory dose of scheduled nonsteroidal medication for up to 10 days, if there are no contraindications. If there are no contraindications, a brief course of oral steroids like prednisone or methylprednisolone may also be taken into consideration.
If rest and nonsteroidal drugs are unable to significantly reduce swelling, medical professionals may inject a local anesthetic, steroid, or a combination of the two at the region of greatest swelling and use ultrasonography to monitor the area. Warming pads applied to the affected area have been beneficial to some patients. Clinicians have suggested resecting cartilage as a therapy option in certain severe, ongoing instances. In general, clinicians advise against using this treatment and advise just evaluating it in specific cases.
- Nonsteroidal anti-inflammatory medications(NSAIDs). This covers medications like naproxen, ibuprofen, and aspirin. Before taking any over-the-counter drug, consult your physician or pharmacist. They will inform you if certain medications can worsen pre-existing diseases or interfere with other medications you are taking.
- Steroids. Your doctor may prescribe corticosteroid pills or provide an injection directly into the affected area if your pain is severe and doesn’t go away with previous treatments. When alternative therapies fail, this can rapidly lessen joint pain and swelling.
- Injection of lidocaine. To relieve pain, your doctor may administer an anesthetic or numbing shot. This is something you might receive when over-the-counter painkillers don’t work, much like the steroid shot.
Physical Therapy treatment
Tietze’s condition is not yet perfectly treated. Whether the sickness is dealt with definitively or not is unknown. Therefore, Tietze syndrome is primarily treated symptomatically. There are currently insufficient reliable clinical trials on the treatment of Tietze’s condition.
Range-of-motion exercises
- Advise on how to perform exercises and demonstrate proper body alignment. Patients must strike a healthy balance between rest and exercise. The physiotherapist must provide accurate information regarding the patient’s posture when sitting and performing regular tasks. Additionally, the patient must refrain from repetitive motions or activities.
- As soon as feasible, range-of-motion exercises should be introduced. While performing the activities, the patient might not experience any pain. You should cease and stay away from vigorous exercises if they make your symptoms worse.
- Exercises for range of motion to increase flexibility, and gradually increase chest mobility.
- Strength training: After the pain goes away, specific shoulder and chest strengthening activities can be added.
Stretching of pectoralis major
- Stretching can be helpful.
- Standing in a corner for 10 seconds with both hands against the wall (like in a push-up) is a good way to stretch the pectoralis major.
- You must repeat it for one or two minutes several times a day.
- Stretching exercises to release tension in the chest region, concentrate on the pectoralis major muscle.
Mobilization of soft tissues
- A light massage to increase blood flow and relieve tense muscles.
- To prevent thoracic rigidity and to lessen symptoms, mobilize the spine and ribs.
- Instruct the patient on breathing techniques.
modalities to reduce pain
- To apply TENS. Shoulder and back exercises can be provocative, thus they should only be used once the problems have subsided. They can apply electroacupuncture and transcutaneous electrical stimulation to the painful spot. The solid filiform needle, another name for the acupuncture needle, is inserted into the affected spinal region. After that, the implanted needle is subjected to low-frequency electrical currents.
- Dry Needling: Assessing and treating musculoskeletal chest wall pain has historically been challenging. It has previously been reported that costochondral-related chest wall pain can be treated with injection therapy using local anesthetics or corticosteroids. According to the findings of an earlier study, dry needling may be just as successful for several syndrome as injection therapy.
Breathing exercises, electrotherapy (such as ultrasound), and cryotherapy (ice) are examples of physiotherapy for Tietze’s condition. You might also receive a soft tissue massage and additional stretching and strengthening exercises. Hydrotherapy is another crucial physiotherapy treatment. To help the patient manage their pain, introduce them to cognitive behavioral therapy and pain neuroscience education.
Home care advise
- Get some rest. Exercise and other forms of physical activity should be taken occasionally to avoid straining your chest and ribs.
- Ice or heat. For a specific period, your doctor could advise you to use hot or cold compresses intermittently. Using cold or heat packs to reduce pain and inflammation in the affected area
- Postural correction: Teaching the patient how to stand correctly to reduce rib strain.
- Heat and cold therapy. To assist prevent muscle overload and reduce pain, use massage and heat/cold pads. Both cold and heat pads work just as well. For the patient to select his favorite. The patient may also apply Vanpooling spray to the affected regions in place of cold pads. This spray can help with chest pain.
- Breathing techniques: Deep breathing exercises to ease pain and increase chest mobility
Complications
Complications Injections, drugs, or surgery may provide a danger, however, complications directly linked to Tietze syndrome are generally uncommon.
- Severe drug reactions
- Infection
- Pneumothorax
Prognosis
You should anticipate fully recovering from costochondral junction syndrome, which is a transient ailment. While some bodies take longer to heal, most people do so in a few weeks. After the pain subsides, the swelling may occasionally persist for several months. Sometimes Tietze’s syndrome appears to disappear and then returns. In certain circumstances, Tietze syndrome may be more persistent than in others due to varying causes and risk factors.
Tietze syndrome often has a good prognosis and resolves on its own. Because the cause or causes of Tietze syndrome are not fully understood, there is uncertainty about how to prevent this disorder. With conservative treatment, the majority of patients report complete symptom relief in 1–2 weeks; however, some patients report that the typical pain and swelling persist for up to a year. Moreover, recurrences are probable. The majority of individuals recover completely from Tietze syndrome.
Having Tietze Syndrome
Tietze syndrome usually resolves on its own without medical intervention. However, there are things you may do to improve your mood while you’re recovering.
You could:
- Use painkillers that are available over the counter.
- If your pain is severe, ask your doctor for a stronger medication.
- Where it hurts, apply ice or heat.
- Discuss with your physician what activities you should refrain from during your recuperation.
- Find out when you can resume chest exercises without risk.
- If your symptoms don’t improve in a few weeks or if you get any new chest pain or swelling, consult your physician.
Which information about Tietze syndrome is the most important to understand?
Tietze syndrome is an uncommon ailment that often affects the second or third rib and is characterized by chest pain and swelling of a single costal cartilage. It is distinguished from costochondritis by the swelling. Young people under 40 are usually the ones who exhibit it. The results of the clinical history and physical examination, along with the elimination of potentially fatal causes of chest pain, are used to make the diagnosis of Tietze syndrome. Painkillers and reducing physical activity until the inflammation subsides are the mainstays of treatment.
What should I avoid if I have Tietze’s condition?
You shouldn’t disregard your symptoms if you think you might have Tietze’s syndrome. Try to utilize a supported cough if you can, and stay away from any activity that can make your symptoms worse. This and other pain-reduction techniques will be taught to you by your physiotherapist.
Is Tietze syndrome dangerous?
However, you should still discuss it with your physician. They will want to rule out other medical disorders like lupus, broken ribs, acid reflux, and dangerous conditions like heart attacks or tumors of the chest wall that may exhibit the same symptoms but need different therapies.
Conclusion
Chest pain and edema are symptoms of the uncommon inflammatory disease Tietze syndrome. It is rarely severe and typically resolves on its own in a few weeks. However, if you believe you have it or if your symptoms persist, consult your physician. You can recover more quickly with rest, medicine, or other therapies.
FAQs
What is the duration of Tietze?
Tietze syndrome is thought to be a self-limiting syndrome that often goes away with rest in a few months. Analgesics and nonsteroidal anti-inflammatory medications (NSAIDs), such as ibuprofen, aspirin, acetaminophen (paracetamol), and naproxen, are typically used to treat Tietze syndrome.
Which medications address Tietze syndrome?
Your soft tissues require relaxation and time to heal from inflammation. Typically, medical professionals recommend just that. Pain and swelling can be reduced using over-the-counter pain medications. Nonsteroidal anti-inflammatory medicines, or NSAIDs, are frequently suggested by providers.
What distinguishes costochondritis from Tietze syndrome?
There is typically no accompanying redness or swelling in costochondritis. 70% of cases involve the second or third ribs, and Tietze syndrome is typically unilateral, affecting only one joint. A history of recent syndrome with coughing or recent intense exertion is frequently present in cases of Tietze syndrome.
What is the Tietze syndrome injection?
Tietze syndrome is typically treated with basic analgesics, such as nonsteroid anti-inflammatory medications, or rest. A local corticosteroid injection is known to be helpful in situations where the patient may remain immobilized for several months.
How much pain does Tietze syndrome cause?
The localized pain may be minor or even severe. Only the upper ribs, specifically T1 through T4, are usually affected by the syndrome; the most frequently impacted levels are the second and third ribs. When it comes to Tietze syndrome, cardiac, pulmonary, and neurological examinations are usually benign.
What might be confused for the syndrome of Tietze?
Though rarer and more significant, Tietze syndrome is sometimes mistaken for costochondritis and is characterized by acute chest pain and localized swelling at the breastbone-rib junction.
What adverse effects might Tietze syndrome cause?
Chest swelling and pain are the most typical signs of Tietze syndrome. It may be bland or acute, or it may be minor or severe. Redness or a warm sensation where it hurts are further symptoms of Tietze syndrome.
Is there a cure for Tietze syndrome?
Physical therapy and stretching or strengthening exercises may be helpful for an early recovery once movement is pain-free. The majority of Tietze syndrome cases go away on their own in a few weeks, however, they can sometimes recur or continue longer.
Is it possible to cure Tietze’s disease?
If I have Tietze syndrome, what can I anticipate? You should anticipate fully recovering from costochondral junction syndrome, which is a transient ailment. While some bodies take longer to heal, most people do so in a few weeks. After the pain subsides, the swelling may occasionally persist for several months.
What is the duration of Tietze syndrome?
Symptoms usually disappear in a few weeks or months. However, some people have swelling for months or more. If you find it difficult to control your symptoms on your own, let your doctor know. To reduce your pain and inflammation, you might need to take further measures.
Reference
- Tietze Syndrome. (2025, January 24). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/23565-tietze-syndrome
- Wiginton, K. (2024, February 11). Tietze Syndrome. WebMD. https://www.webmd.com/pain-management/tietze-syndrome
- Wikipedia contributors. (2024, August 17). Tietze syndrome. Wikipedia. https://en.wikipedia.org/wiki/Tietze_syndrome
- RIB pain | Aurora Health Care. (n.d.). https://www.aurorahealthcare.org/services/heart-vascular/conditions/rib-pain
- Pt, S. R. B. (2024, September 23). Can dehydration make costochondritis worse? CARESPACE Health+Wellness. https://carespace.health/post/can-dehydration-make-costochondritis-worse/