Lumbar Instability
Introduction:
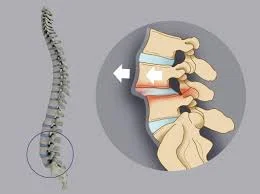
Lumbar instability is a spinal disorder characterized by abnormal movement or joint deformation between two or more contiguous vertebrae. When a patient has lumbar instability, there is excessive movement between the vertebrae, which leads to gradual deterioration of the intervertebral joints and can impair the nervous system components that run through them.
Lumbar instability is a major cause of low back pain and can lead to significant disability.
According to the World Health Organization’s worldwide disease burden report, back pain is the leading cause of disability-adjusted life years.
Spinal stability:
Spinal stability can be attributed to one, two, or three “sub-systems” that have a significant impact on the spine. They are:
- Spinal column and ligaments
- The nervous system regulates spinal mobility.
- Muscles move the spine.
In a healthy condition, the three systems collaborate to maintain stability. When one of these subsystems is injured, for as via age-related degeneration, fractures, or neuromuscular illness, the remaining two must compensate. When it comes down to it, you can’t tell one spinal subsystem from another. Clinical instability is essentially a multi-system disorder.
The ensuing imbalance can cause an unstable spine and discomfort, as well as significantly damage the patients’ quality of life by prohibiting them from performing their everyday duties.
There are two types of lumbar instability: functional (clinical) and structural (radiographic).
Functional instability, which can induce pain even in the absence of radiologic abnormalities, is characterized by neuromotor control over segmental movement during the midrange.
Structural or mechanical instability is the failure of passive stabilizers that control excessive segmental end range of motion (ROM).
It is also possible to have mixed instability.
Relevant anatomy:
Spinal instability is most commonly caused by injury or damage to the spinal column. The spinal column is a complicated structure with several potential faults in the subsystems.
Spinal Stabilisation System:
The passive subsystem includes the intervertebral disc, ligaments, facet joints and capsules, vertebrae, and passive muscle support.
Facet Joint Capsular ligaments (which cover and support the facet joints) can relax. When they do, they cause excessive movement—and hence instability—in the spine. Capsular ligament laxity can be caused by various conditions, including disc herniation, spondylosis, whiplash-related issues, and others.
Active subsystems include spinal muscles and tendons, thoracolumbar fascia, and Spinal muscles are the strong engines that propel the spine. They also offer rigidity and stability. Spinal instability can be caused by weakness or injury to the muscles that support the spine, such as multifidus and transverse abdominal. Ultrasound may reveal wasting (a symptom of weakening) in deep spinal muscles, although electromyography (EMG) is commonly utilized to identify muscle alteration.
The nervous system receives data regarding the location of the spinal bones and columns and generates movement impulses. These impulses are sent to the muscles, prompting them to contract. Muscle contraction drives spinal motions and maintains stability. If these muscles contract slowly or in an atypical way, there may be a problem with the brain control subsystem. An EMG test can identify both of these issues.
These disturbances can produce alterations in spinal movement patterns that can be seen with a trained eye (or a motion-detecting system). Nerve conduction studies can potentially uncover abnormalities in the neural control sub-system. An NCS is frequently conducted in conjunction with an EMG to detect related muscle stress or injury.
Causes of Lumbar Instability:
The main causes of lumbar instability are classified as follows:
Degenerative: The most common cause of spinal instability in adults is degeneration or premature wear of the intervertebral discs, the most significant portion of the spine, resulting in abnormal movement of these structures. This can happen to persons who have a higher genetic susceptibility to it, as well as those whose bodies are subjected to excessive exercise. Poor posture, poor physical condition, muscle insufficiency, sedentary lifestyle, excess body weight, injury, and other factors all contribute to these degenerative disorders.
Congenital:
The most common congenital condition is spondylolisthesis, caused by spondylolysis (a bone abnormality at the intersection of the facet joints).
Lumbosacral transition abnormalities (lumbarization of the first or fifth sacral vertebra).
Scoliosis is characterized by an abnormal alignment of the spinal bodies.
Acquired:
After surgery.
Infections and tumors are two examples of lumbar spine pathologies.
Symptoms for Lumbar Spinal Instability:
Symptoms vary according to the degree of the instability and individual circumstances. Common symptoms include:
- Low back discomfort is the most prevalent symptom, which can be characterized as dull, aching, or acute. It may radiate to the buttocks and legs.
- Back muscles can spasm in reaction to instability, producing discomfort and stiffness.
- Numbness and tingling in the legs and feet might be caused by pinched nerves as a result of instability.
- Weakness: The legs may feel weak or wobbly, which affects balance and coordination.
- Loss of flexibility: The spine can become rigid and difficult to move, making bending and twisting difficult.
- Difficulty walking: Walking might become unpleasant and unsteady, affecting regular tasks.
How is Spinal Instability Diagnosed?
Diagnosing spinal instability requires a mix of professional judgment and modern imaging tools. For example, here’s how it is usually done:
Comprehensive Medical Evaluation:
Patient’s History: A detailed medical history, including symptoms and previous injuries, aids in the diagnosis procedure.
A comprehensive physical exam evaluates mobility, reflexes, and any indications of nerve injury.
The physical examination may include numerous tests:
Low midline sill sign:
To identify the low midline sill sign, evaluate the patient’s lower back’s midline first. A sill resembling a capital “L” on the midline indicates a favorable test result if the lumbar lordosis increases. Next, the examiner palpates the interspinous space to determine the location of the upper spinous process concerning the lower spinous process. If the top spinous process is moved anterior to the lower spinous process, the test is affirmative.
Interspinous gap changes during lumbar flexion-extension motion:
This test is used to diagnose lumbar instability. First, the lower back is examined to see whether the interspinous gap has changed. The patient stands shoulder-width apart, flexes his back, and rests both hands on an examination table. After inspecting the lower back in flexion, the physiotherapist palpates and assesses the breadth of the individual interspinous space and the location of the upper spinous process concerning the lower one. Following that, the physiotherapist will instruct the patient to extend (or hollow) the lower back while assessing the interspinous gap change during this motion.
Sit – to – stand test:
The Sit-to-Stand test is positive (associated with instability) if a person has discomfort when sitting and partially relieves it by standing.
Passive Lumbar Extension Test (PLE test ):
The Passive Lumbar Extension Test (PLE) involves placing the patient in a prone posture. The therapist lifts both lower extremities passively to a height of approximately 30cm. The knees remain extended while softly pulling the legs. The examiner locates T12 ventrocaudally. This test can also be performed in a lateral posture with the patient’s legs bent. The test is positive if it produces comparable symptoms.
Instability catch sign (active flexion test):
The Instability Catch Sign (active flexion test) is a provocation test that involves the patient bending forward as far as possible and then returning to a neutral position. A positive result indicates that the patient is unable to return to the neutral position.
Advanced Imaging Techniques:
MRI Scans: Magnetic Resonance Imaging (MRI) delivers a thorough image of spinal structures, assisting in the diagnosis of herniated discs or concerns with vertebral alignment.
CT Scans: Computed Tomography (CT) offers detailed pictures of bone structures, which is critical for detecting anomalies in the spine that may cause instability.
Specialized Diagnostic Tests:
X-rays are frequently used to study vertebral movement, particularly while changing postures, to diagnose instability.
Dynamic imaging: flexion and extension. X-rays show how the spine moves, which might identify instability that static imaging may overlook.
Treatments for lumbar instability:
Non-Surgical Treatment Options: To address lumbar spinal instability, non-surgical therapies are frequently used first.
- Physical therapy: Increasing core muscular strength and flexibility can help to stabilize the spine and relieve discomfort.
- Pain management: Nonsteroidal anti-inflammatory medications (NSAIDs) and pain relievers can help with pain symptoms.
- Wearing a lumbar brace can give support while restricting excessive movement.
- Lifestyle changes, such as maintaining a healthy weight, avoiding activities that aggravate symptoms, and adopting excellent posture, can all assist in controlling instability.
- Epidural steroid injections can temporarily relieve pain by lowering inflammation surrounding the nerves.
Surgical Treatment Options:
Surgery may be a viable option for patients with significant instability or who do not respond to non-surgical treatments. The most common surgical options are:
Spinal fusion: This operation combines two or more vertebrae to form a stable piece. This helps to correct spinal instability and dramatically lowers pain from worn-out joints. When vertebrae are fused, the spinal column becomes more balanced, resulting in better function and comfort for the patient.
This operation is especially advantageous for patients whose quality of life is compromised by severe spinal disorders since it provides both structural support and relief from persistent pain.
Physical Therapy Management:
Patient education is essential in the management of patients with segmental instability. This teaching should not be limited to the instances in which the patient should not perform. However, it should encourage the patient to be active while also recognizing which motions should be avoided or undertaken with extreme caution. These are loaded flexion motions because they may cause a posterior displacement of the disc. In addition, any end-range lumbar spine postures should be avoided since they overburden the posterior passive stabilizing elements.
Diaphragmatic breathing with abdominal bracing:
Lay on your back, legs bent, and lay your hands on either side of your ribs.
Inhale through your nose and feel the breath go beneath your palms and toward the back of your rib cage. Imagine your ribcage as a balloon that expands in all directions when you breathe in. Exhale, and feel your hands sliding closer together as your ribcage narrows down towards the floor and into the center of your body. Maintain a relaxed neck, shoulders, and chest while feeling the rear of your rib cage connected to the floor.
Maintain a neutral pelvis (not tucked or unduly arched). Inhale again.
Then, exhale while picturing a broad belt around your lower back and lower abdomen. Gently tighten and elevate the belt as your deep core engages. Aim for a moderate contraction in these muscles, without grabbing or holding onto extra tension. You should be able to communicate with someone during contracting.
Bridging
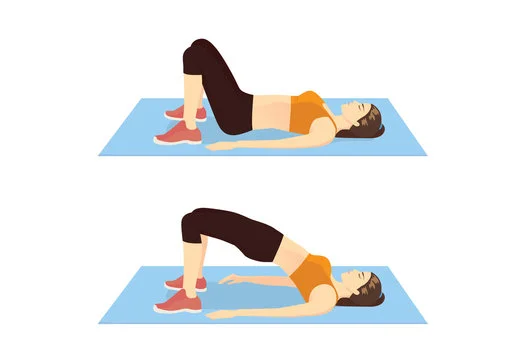
inhale while lying on your back, legs bent, feet parallel, and hip-width apart.
Exhale and brace your abdominals as described above. Lift your hips off the ground by engaging your glutes and pushing your feet onto the floor.
Inhale as you release the position back down. Aim to maintain your shoulders and neck relaxed throughout. Avoid overarching your back.
Complete 8-10 repetitions.
Side plank on knees.
Begin by sitting on your side, on one hip, with your legs bent and piled beside you. Bend your elbow and lower your forearm on the ground beside you.
Exhale and drive your forearm into the floor, then elevate your hips into the air.
Inhale and drop your hips halfway.
Exhale to raise your hips again.
Repeat 8-10 times, then inhale while lowering your hips with control.
Repeat on the opposite side.
Bird Dog

Begin on all fours, knees precisely beneath your hips and hands below your shoulders.
Aim for a neutral spine.
Exhale to bring the abdominals inside and upward. Without changing your weight or arching your back, raise one leg behind you and your opposing arm in front.
Breathe and maintain the posture for three slow counts.
Inhale carefully to return your leg and hand to the mat.
Complete 6-8 repetitions, then repeat on the opposite side.
Long-Term Advantages of Treatment:
Effective treatment of lumbar spinal instability can bring considerable long-term advantages.
Reduced pain: Treatment can aid in pain management and enhance overall quality of life.
Improved mobility: Greater flexibility and strength enable more efficient movement and involvement in daily activities.
FAQs
How do you manage lumbar instability?
Treatments
Physical therapy can help cure minor cases of spinal instability by strengthening the muscles in the spine.
Prescription pain relievers and anti-inflammatory medications.
A microdiscectomy is a surgical treatment that involves removing the intervertebral disc that is impinging on the spinal nerve.
What symptoms indicate lumbar spine instability?
Pain might be accompanied by weakness in the leg or foot. Abnormal movement might also result in excruciatingly painful muscular spasms. Signs of spinal macro-instability may include back discomfort, weakness, and/or numbness in the arms and legs.
How do you check for lumbar instability?
The patient is supine, and the examiner instructs him to elevate both lower extremities. The knees must be extended. The examiner next asks the patient to carefully return to the starting position. If the lower extremities slid down immediately due to low back discomfort, the test proved affirmative.
How do you sleep when your lumbar spine is unstable?
Sleeping on your side.
If you sleep on your side, pull your legs up slightly towards your chest and place a cushion between them. Flexing your knees and placing a pillow between your legs might assist in aligning your spine, pelvis, and hips. This posture relieves strain on your spine. If you’d like, use a full-length body pillow.
Can paralysis result from lumbar instability?
Patients may occasionally additionally have muscle spasms. Weakening of the muscles. Paralysis.
Can spinal instability be shown on an MRI?
Until true discontinuity was shown at that level, soft tissue hemorrhage in the interspinous gap was not linked to ligament rupture. We conclude that the majority of unstable spinal injuries may be quickly and reliably assessed by MRI immediately, negating the need for further imaging.
Is there a cure for the lumbar spine?
Additionally, you can experience numbness or discomfort in your legs. In more extreme situations, you can experience difficulties managing your urine and bowel movements. Although lumbar spinal stenosis cannot be cured, there are several therapeutic options available.
Is there a substantial risk of spinal instability?
It can result in several problems that can significantly affect a person’s quality of life and is frequently brought on by trauma or degenerative diseases. That effect may be considerably lessened by educating my patients and creating individualized treatment programs.
References
- Lumbar instability: causes, symptoms and treatments. (n.d.). https://www.institutoclavel.com/en/lumbar-instability
- Southwest Scoliosis Institute. (2021, January 15). THE TETHER VERTEBRAL BODY TETHERING SYSTEM. Southwest Scoliosis and Spine Institute. https://scoliosisinstitute.com/lumbar-spinal-instability/
- Menzies, R. (2022, October 26). What are lumbar stabilization exercises? Healthline. https://www.healthline.com/health/lumbar-stabilization-exercises#bottom-line