Peripheral Nerve Injury
What is a Peripheral Nerve Injury?
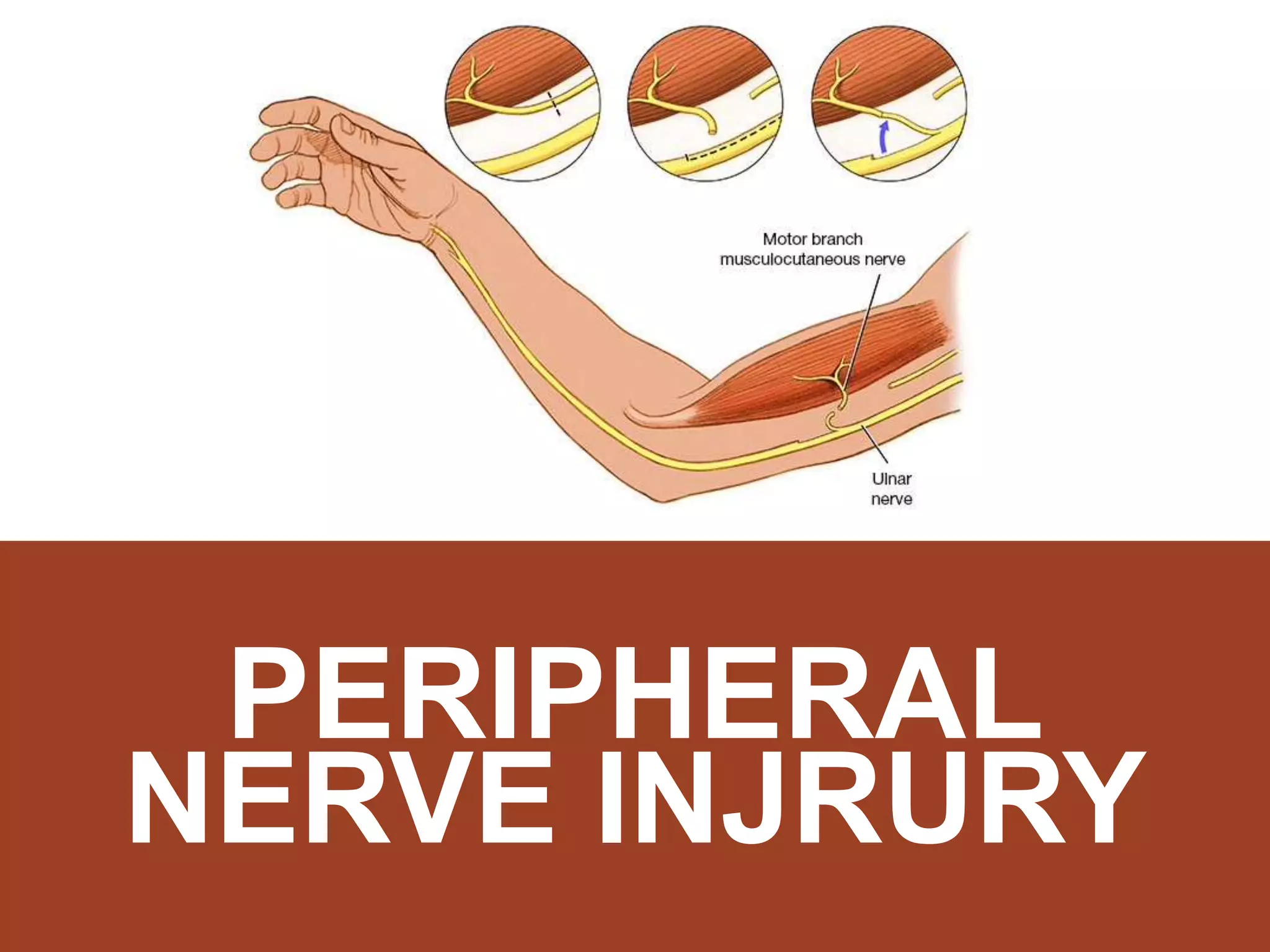
Peripheral nerve injury causes damage or disruption to the nerves that extend from the spinal cord and brain to the rest of the body, which affects sensation, movement, and motor coordination.
The peripheral nervous system is a group of motor and sensory nerves that connect the central nervous system (the brain and spinal cord) with the rest of the body. These nerves transmit sensation, movement, and motor coordination. A nerve damage may impair the brain’s capacity to connect with muscles and organs. They’re fragile and get easily damaged.
Peripheral nerve problems occur when one or more peripheral nerves get injured. Nerve injury might result in signal loss or complete breakdown. Depending on which nerves are affected, you may have pain, tingling, numbness, difficulty walking, or a variety of other symptoms. Nerve regeneration may or may not be achievable, depending on the kind and severity of injury.
Peripheral nerve injury treatment depends on the type of injury, symptoms, and the amount of nerve injury sustained. depending on which nerves are involved. When one of these nerves is severely damaged or stressed, surgical intervention may be required.
Classification of Peripheral Nerve Injury
There are two popular categories for peripheral nerve injury: the Seddon Classification and the Sunderland Classification. Seddon identifies peripheral nerve damage as neuropraxia, axonotmesis, and neurotmesis. Sunderland improved on this notion by categorizing them into various degrees or levels of injuries.
Neurapraxia( First degree)
This form of nerve damage is frequently the result of compression pathology. This is the mildest type of peripheral nerve injury, with little structural damage. This allows for a full and fairly rapid healing period. A neuropraxic injury occurs when a localized section of the nerve is demyelinated at the affected site, but the axon or its surrounds are not injured or disrupted. This is mainly due to chronic ischemia caused by high pressure or nerve stretching without Wallerian degeneration. symptoms of pain, muscle weakness, numbness, and proprioception issues with no muscle wasting
Axonotmesis ( Second and Third degree )
An axonotmesis injury causes damage to both the axon and the myelin sheath. However, the endoneurium, perineurium, and epineurium are intact. Although the internal structure is intact, injury to the axons causes Wallerian degeneration. This sort of nerve damage also leads to complete healing but at a slower rate than a neuropraxic injury. Symptoms of pain, muscle wasting, and complete motor, sensory, and sympathetic function loss
Neurotmesis ( Third Fourth and Fifth degree)
Neurotmesis damage can occur at several levels, thus we employ Sunderland’s additional breakdown of peripheral nerves. 3rd-degree neurotmesis damage is caused by axon and endoneurial disruption. When this happens, the perineurium and epineurium stay intact. Axon and perineurium disruption is classified as fourth-degree damage. Total disruption of the nerve trunk is categorized as a 5th-degree injury. symptoms of no pain (anesthesia), muscle wasting, and complete motor, sensory and sympathetic function loss
(Sixth Degree) (MacKinnon & Dellon) Mixed levels of injury along the nerve

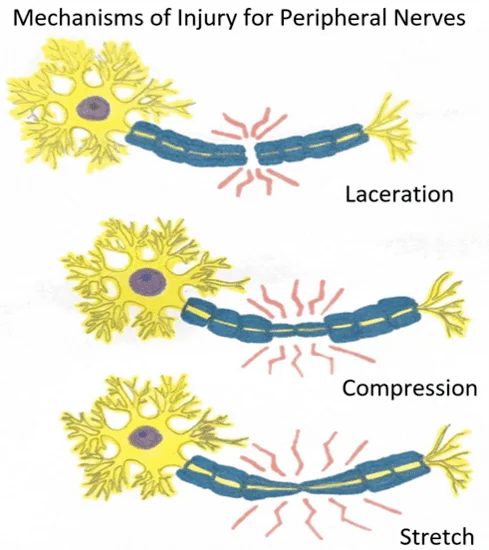
Causes of peripheral nerve injury
Injury to the peripheral nerve network can occur by the following:
- Diabetic people with diabetes will develop diabetic nerve problems.
- Physical trauma like falls or overstretching of a limb
- Injury caused by an accident, a fall, or sports can stretch, compress, crush, or cut off the nerve.
- Infections
- Laceration(cuts or tears in nerve tissue)
- severe bruise (contusion)
- gunshot wounds
- Pulling strech (Traction)
- Injuries due to drug injection
- Electrical injury
- Birth injury to brachial plexus
- Health conditions including diabetes
- Autoimmune disease Rheumatoid arthritis and lupus
- Certain cancers
- blood vessel problems
- severe fracture
- Dislocation of joint or bone
- excessive intake of alcohol and smoking
- Exposure to toxins
- Any surgery
Types of Peripheral Nerve Injury
Peripheral nerve injuries include
- Spinal accessory nerve injury
- Brachial plexus injury (Birth injury) which includes:
- Erb’s palsy (upper trunk palsy)
- klumpek’s palsy (lower trunk palsy)
- Radial nerve damage (wrist drop)
- Peroneal nerve damage (footdrop)
- carpal tunnel syndrome
- Tarsal tunnel syndrome
- Thoracic outlet syndrome
Spinal accessory nerve injury
The spinal accessory nerve is the eleventh of twelve cranial nerves originating in the brain. It helps two types of neck muscles to work: the sternomastoid muscles, which allow the head to tilt and rotate, and the trapezius muscles, which allow for some moves such as shrugging the shoulder or rotating the shoulder blades.
The spinal accessory nerve can be damaged after trauma or even during surgery when physicians operate on lymph nodes or the jugular vein in the neck.
The symptoms include shoulder pain, stiffness, outward “winging” of the shoulder blades, and weakening or shortening of the trapezius muscle.
Quick treatment and diagnosis give you the best chance of recovering from this injury. Doctors are likely to give physical therapy for minor spinal accessory nerve damage. Deeper injuries might require surgery, such as nerve grafting, regeneration, or tendon or muscle transfer.
Brachial plexus injury
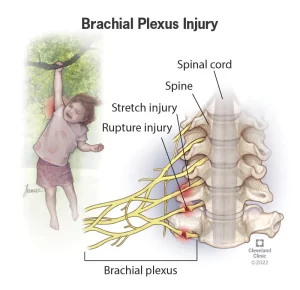
The brachial plexus is a neural network that connects the spinal cord with the shoulders, arms, and hands. The brachial plexus innervates the whole upper arm, with two exceptions: the trapezius muscle (CN XI) and a region of skin around the axilla (intercostobrachial nerve). A brachial plexus injury occurs when these nerves are stretched, broken, or, in the most severe cases, torn from the spinal cord.
When the arm is pulled or stretched with violence, this network of nerves can be damaged and cause paralysis of the supplied muscles.
There are multiple types of brachial plexus injuries.
Erb’s palsy (upper trunk palsy)
Erb’s point is located on the upper trunk of the brachial plexus. Six nerves connect here. Erb’s paralysis occurs due to an injury to the upper trunk.
Causes
Unnecessary separation of the head from the shoulder, which usually occurs in,
- Birth injury (extreme pull of the neck)
- physical trauma
- motor accidents
- Fall on shoulder
- During anaesthesia
Nerve root involvement :
- it involves nerve roots mainly C5 and partly C6
Muscle paralyzed are :
- the biceps, deltoid, brachialis, and brachioradialis muscles
- Partly Rotator cuff muscles supraspinatus, infraspinatus, and supinators
It causes the inability to do :
- Abduction, lateral rotation of the arm
- flexion and supination of the forearm and
- Biceps and supinator jerks are lost
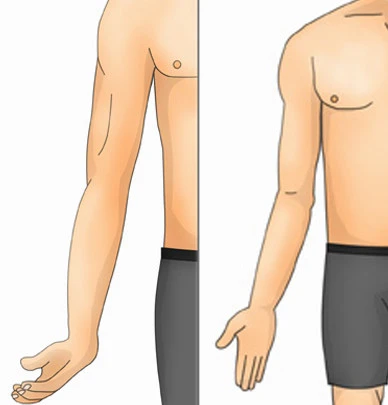
It leads to deformity in the upper extremity :
- in which the Arm: Hangs by the side, adducted and medially rotated
- Forearm: Extended and pronated
- Also called “Porter’s tip hand” or “policeman’s deformity.”
Klumpek’s palsy (lower trunk palsy)
Injury to the Lower trunk of the brachial plexus is called Klumpek’s paralysis
Causes of injury :
- Excessive arm abduction, for example, picking up a branch from a tree after a fall
- Birth injury ( excessive pull of arm)
- fall from the height of an outstretched hand
Nerve root involvement :
- it involves nerve roots mainly T1 and partly C8
Muscle paralyzed are :
- Intrinsic muscles of the hand (T1)
- wrist and fingers Ulnar flexors (C8)
Deformity :
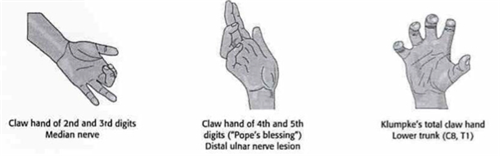
- Claw hand (hand position) is caused by the unopposed action of the long flexors and extensors of the fingers. Claw hands have hyperextension at the metacarpophalangeal joints and flexion at the interphalangeal joints.
Disability:
- Claw hand
- Cutaneous anesthesia and discomfort relief in a limited zone along the ulnar border of the forearm and hand.
Radial nerve damage (wrist drop)
Radial neuropathies result from radial nerve damage caused by compression, ischemia, arm fractures, or cutting wounds. Wrist drop is the most common presentation. The type of neuropathy is defined by the level of damage. Radial nerve palsy is sometimes called crutch palsy, Saturday night palsy, or honeymooner’s palsy.
Cause:
A condition that can arise after extending one’s arm over a chair (or crutches) for a long period, resulting in pressure damage to the radial nerve.
Nerve root involvement :
- Radial nerve lesions involve the nerve root (c7,c8)
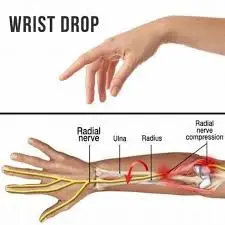
Disability:
- Weakness in finger flexion, wrist extension, and brachioradialis
- Finger extensor weakness and radial deviator weakness during wrist movement
Deformity :
- Wrist drop
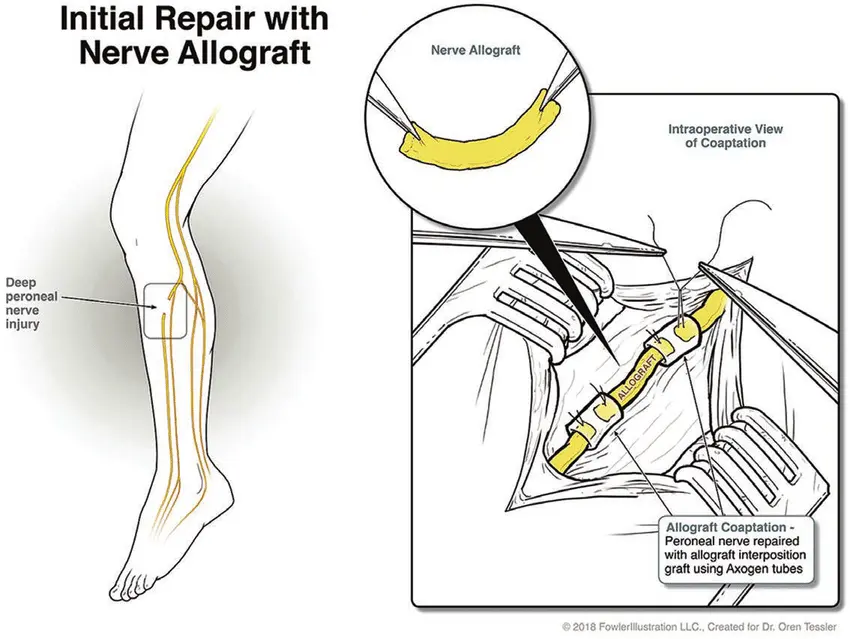
Peroneal nerve damage (foot drop)
Foot drop is most commonly caused by injury to the peroneal nerve. This nerve, commonly known as the fibular nerve, is a branch of the sciatica. It causes movement and feeling in the lower leg, foot, and toes.
Causes :
Foot drops can be caused by conditions affecting the body’s nerves and muscles. They include the following:
- Peripheral neuropathy— Diabetes is the most prevalent cause of peripheral neuropathy. Tooth disease is a prevalent hereditary peripheral neuropathy.
- Foot drop is caused by some muscle illnesses, such as muscular dystrophy.
- Poliovirus causes muscular weakness and paralysis.
- Crossing your legs at the knees might potentially harm the peroneal nerve.
- Muscle weakness and paralysis can result from brain and spinal cord illnesses, such as:
- Stroke
- ALS
- MS
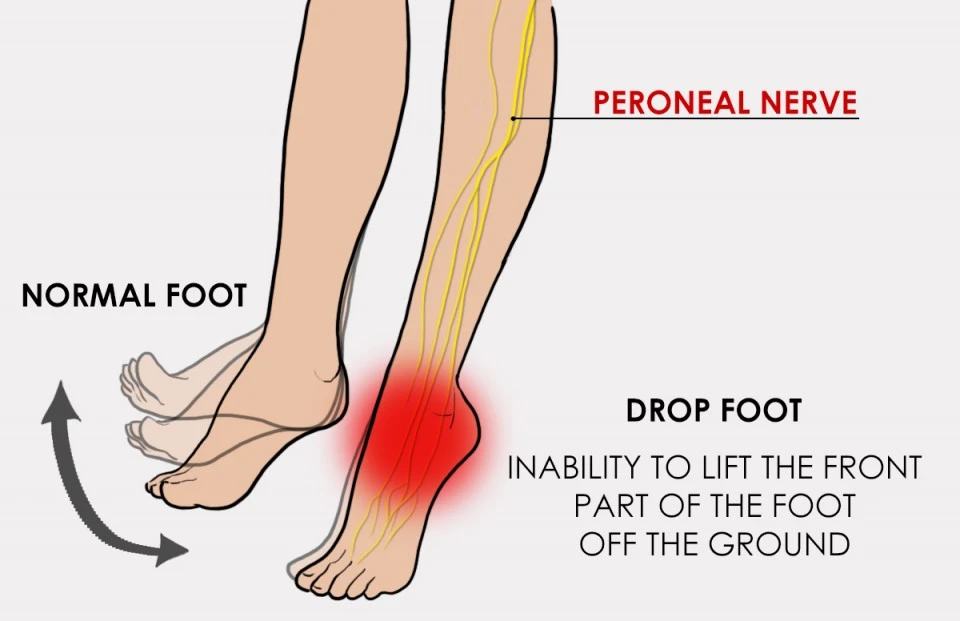
Disability:
paralysis or weakness of the anterior tibialis muscle. Although the anterior tibialis plays a major role in dorsiflexion which is supplied by the peroneal nerve
Deformity :
- Damage to this peroneal nerve leads to the dropping of foot
- the person will be unable to dorsiflex the foot or raise the foot toward them
Carpal tunnel syndrome
Carpal tunnel syndrome occurs when the tunnel becomes narrow or when the tissue around the flexor tendons (known as synovium) increases, compressing the median nerve and reducing its blood supply. pressure on the median nerve, as it travels through the carpal tunnel, is known as Carpal tunnel syndrome.
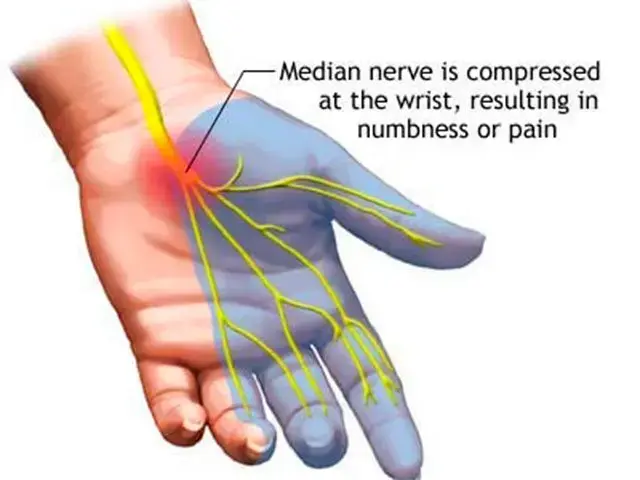
Cause :
- Heredity
- Repetitive hand use
- Hand and wrist position
- Health conditions like
- diabetes
- Rheumatoid arthritis
Symptoms :
Carpal tunnel syndrome symptoms may include the following:
- Numbness, tingling, burning, pain, and being uncomfortable typically affect the thumb, index, middle, and ring fingers. This frequently wakes individuals awake at night.
- Sometimes, shock-like sensations travel to the thumb, index, middle, and ring fingers.
- Pain or tingling may spread up from the forearm to the shoulder.
- Weakness and clumsiness in the hand may make it difficult to accomplish specific actions, such as buttoning your garments.
- Dropping objects—due to weakness, numbness, or a lack of proprioception
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome (TTS) is a compression neuropathy affecting the posterior tibial nerve.[1] The tunnel is located under the flexor retinaculum and posterior to the ankle’s medial malleolus. Symptoms include discomfort spreading into the foot, which is typically increased by walking (or weight-bearing activities). An examination may suggest Tinel’s sign over the tibial nerve at the ankle, weakness, and atrophy of the tiny foot muscles, or a lack of feeling in the foot
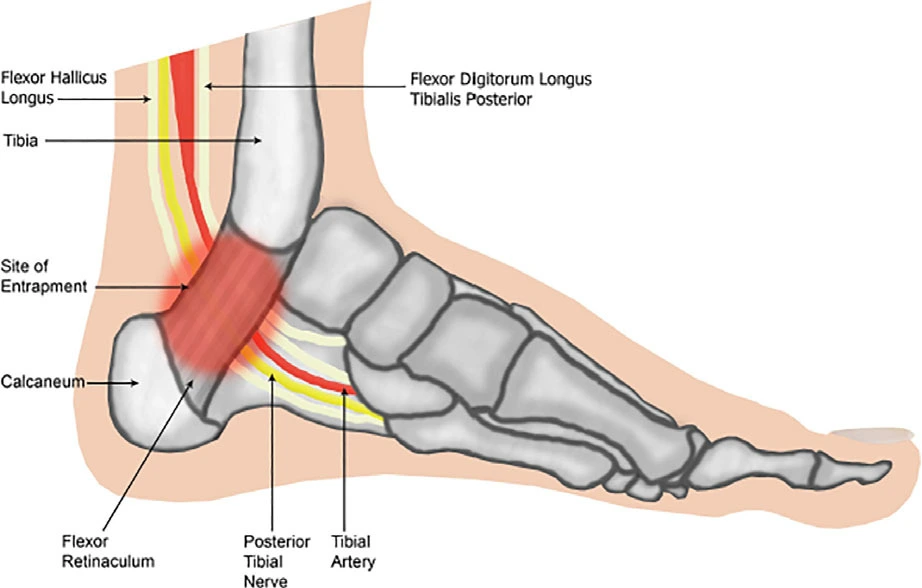
Causes :
- Heredity
- improper shoes
- flat foot or exaggerated arch of the foot
- uneven weight bearing
- Repetitive use of ankle or foot
- excessive exercise
Symptoms :
- Patients with tarsal tunnel syndrome have one or more of the following symptoms:
- Tingling, Numbness, burning, or a sensation like an electrical shock
- pain, particularly shooting pain
- Symptoms are frequently felt on the inside of the ankle or the bottom of the foot. In particular individuals, a symptom may be localized and develop in only one location. In others, it can spread to the heel, arch, toes, and even the calf.
- Symptoms of the condition may appear suddenly. They can often be started or worsened by overuse of the foot, such as prolonged standing, walking, exercising, or starting a new fitness program.
Thoracic outlet syndrome
Thoracic outlet syndrome (TOS) is a group of conditions that put stress on blood vessels or nerves between the neck and shoulder. This area is referred to as the thoracic outlet. Compression of blood vessels and nerves can result in shoulder and neck discomfort. It might also cause numbness in your fingertips.
Causes :
- Thoracic outlet syndrome is frequently caused by car accidents, repetitive strains from sports or the workplace, and pregnancy.
- Differences in anatomy, such as having another or uneven rib, can potentially lead to TOS.
- Sometimes the reason for thoracic outlet syndrome is unknown.
- Physical therapy and pain management are frequently used as treatment options. Most patients improve after receiving these therapies. For some, surgery may be necessary.
Types :
Three kinds of thoracic outlet syndrome are recognized:
- Neurogenic thoracic outlet syndrome. This is the most typical kind of thoracic outlet syndrome This sort of injury compresses a network of nerves known as the brachial plexus. The nerves of the brachial plexus begin in the spinal cord Nerves control muscular movement and sensation in the shoulder, arm, and hand.
- Venous thoracic outlet syndrome. This kind of thoracic outlet syndrome develops when one or more veins under the collarbone get squeezed and injured. This can lead to blood clots.
- Arterial thoracic outlet syndrome. This is the least typical form of TOS. It develops when one of the arteries behind the collarbone becomes squeezed. The compression may injure the artery, which leads to a bulge, known as an aneurysm, or blood clot formation.
Symptoms :
Symptoms of thoracic outlet syndrome vary according to form.
Symptoms of Neurogenic thoracic outlet syndrome may include :
- It can cause sensations of numbness or tingling in the arm or fingers due to nerve compression.
- Pain in the neck, shoulder, arm, or hand.
- Arm tiredness occurs with exercise.
- A falling grasping. (weak grip)
Symptoms of venous thoracic outlet syndrome may include :
- changes in the color of the hand or fingers.
- Hand or arm discomfort and swelling.
The following are possible signs of arterial thoracic outlet syndrome:
- A vibrating weight on the collarbone.
- Cold fingers, hands, or arms.
- Hand and arm ache.
- A change in color in one or more fingers, or the entire hand.
- A weak or absent pulse in the afflicted arm
Peripheral Nerve Injury Symptoms
There are many symptoms of peripheral nerve damage. The condition can affect a single nerve, a system of connected nerves, or many nerves over your body. The symptoms also depend on the type of nerve signal damaged; many signal types may be involved.
The symptom types (with more information below) are:
- Motor.
- Sensory and pain.
- Autonomic.
Motor symptoms
our peripheral nervous system transmits motor impulses, which are orders from your brain to your muscles. These signals allow you to move around. To stay healthy and working, your muscles need nerve connections to the brain.
Motor symptoms include:
- Muscle weakness and paralysis. Peripheral neuropathy causes nerve degeneration, which weakens the surrounding muscles. This can result in paralysis, making it difficult to move the toes, as well as foot drop and hand weakness. Weakness can affect muscles in the thighs, arms, and other areas.
- Muscular atrophy. Loss of nerve connectivity can cause muscles to shrink and weaken. This especially occurs in the feet, lower legs, and hands of patients with peripheral neuropathy. Muscle loss may cause anomalies in the feet and hands.
- Uncontrolled muscular actions. Nerves that lose contact with the brain because of peripheral neuropathy can become hyperactive on their own, resulting in cramping.
Sensory symptoms
our peripheral nerves transform information from the outer environment into nerve impulses. These impulses then travel to your brain, where they are converted into how you think of the world. Peripheral neuropathy may affect your senses’ capacity to see the outside environment and interact with your brain.
The sensory signs of peripheral neuropathy are:
- Tingling. This occurs when there is an issue with the nerves that send messages to your brain.
- Numbness. This occurs when nerves fail to send or transfer sensory impulses, resulting in the loss of some types of feelings. For example, picking up a cold pop can but not feeling its smoothness or coolness, or not feeling the texture of the carpet or the temperature of the floor through your fee
- Imbalance and clumsiness. Nerves also carry sensations, which your brain takes for monitoring the position of your hands and feet. You are not aware of these feelings, yet they are necessary to maintain balance and coordination. Without these sensations, you can lose balance, particularly in the dark, and become clumsy with your hands.
- Pain. Nerve damage from peripheral neuropathy can create problems in how and when nerves give pain signals, making them more powerful (hyperalgesia) or occurring too frequently. It may cause nerves to produce their pain impulses. The most obvious and unpleasant symptom of peripheral neuropathy is this pain, which is referred to as “neuropathic” pain.
Autonomic symptoms
Our body has multiple autonomic processes. Problems in autonomic signals mean that your body’s automatic systems cannot function properly. These are your body’s autonomic actions that occur without any conscious thinking or awareness. They include sweating, digestion, blood pressure control, and other functions. Autonomic nerve fibers transmit autonomic impulses. Some may run occasionally, while others may never function.
Autonomic signs of peripheral neuropathy may include
- Blood pressure changes. Your body usually regulates blood pressure, but peripheral nerve injury may interfere with this process. This can result in rapid decreases in blood pressure or increases in heart rate, particularly while standing up.
- Sweating too much or not enough. Your body automatically regulates the inside temperature by sweating to release heat. Peripheral nerve injury might cause you to sweat excessively or not enough. This might cause dry skin and scaling on your feet, as well as a lot of sweat after eating.
- Bowel and bladder problems. You are not aware of the autonomic impulses that regulate your bowels and bladder. Nerve fiber damage can alter bowel motions (constipation or diarrhea) and, on certain occasions, bladder control.
- Sexual dysfunction. Your autonomic nerve system regulates the feeling of sexual desire. This is why autonomic disorders can cause sexual dysfunction.
Other symptoms. Autonomic changes caused by peripheral neuropathy can also result in skin color changes, edema, pupil changes, and blurred vision.
Complications of peripheral nerve injury
- Adhesions
- Poor tendon gliding
- Neuroma formation
- Pain & Hypersensitivity
- Intense pain can result from peripheral nerve damage, particularly nerve root avulsions, which cause neuropathic pain.
- Extreme pain can also mainly lead to complicated regional pain syndrome, all of which can affect repair.
- Altered Sensation
- Peripheral nerve damage is frequently associated with severe alterations in feeling, including numbness, tingling, burning sensation, or complete
- Loss of feeling in the area of the body affected by the injured nerve increases the risk of complications such as pressure ulcers, burns, and lacerations.
- Pressure Ulcers
- Pressure sore due to foot drop
- There are extrinsic and intrinsic variables that contribute to tissue damage.
- Extrinsic variables include pressure, shear, friction, immobility, and wetness
- Intrinsic factors associated with the patient’s status include local infection, impaired autonomic control, sepsis, changed level of awareness, increasing age, vascular occlusive disease, anemia, malnutrition, sensory loss, and contracture.
- Burns & Lacerations:
- Burns and skin lacerations caused by contact with hot surfaces or water, sharp surfaces, or the failure to wear protective clothes, for example:
- Shoes are often associated with altered or diminished feelings following peripheral nerve damage.
- Delayed Healing:
- Peripheral nerve damage can impact and slow down the healing processes of soft tissues. Muscle weakness can worsen this by interfering with blood circulation in the distal limbs, resulting in edema and poor recovery.
- Smoking is another risk that may cause the healing process to take longer since it drastically reduces the blood supply to the injured nerve and soft tissue.
- Diabetes and nutrition might cause recovery to be delayed if enough protein and nutritional intake are not maintained.
- Swelling: Because peripheral nerve damage causes motor dysfunction in the extremities, it impairs the muscle pump from the distal aspect of the limbs, especially in a sciatic nerve injury, When the distal limbs are in a gravity-dependent posture, blood pooling may occur. This may result in greater neuropraxia due to increasing nerve compression and discomfort.
- Contracture & Deformity: Contractures are caused by a lack of extensibility in the soft tissue structures that connect joints–skin, ligaments, muscles, and joint capsules–resulting in restricted joint motion, joint stiffness, and, eventually, deformity. Contractures impair joint mobility and limit everyday activities. They are also linked to discomfort, stiffness, sleep difficulties, and skin deterioration. Contractures most commonly affect the joints necessary for everyday living: hips, knees, ankles, wrists, and shoulders, creating difficulties with dressing, eating, transferring, sleeping comfortably, using a wheelchair, or doing any chores that need complete joint motion. Problems in any of these areas can limit a person’s mobility. If affected muscles’ joints are not manipulated passively regularly, they shorten and stiffen, resulting in contracture and abnormalities. Positions or postures in which the patient spends most of the day in bed or a wheelchair raise the chance of contracture, as well as discomfort, This increases the time soft tissues spend in shorter postures. Stretching, range-of-motion and strengthening exercises, splinting, serial casting, and positioning should all be utilized to avoid and treat contractures
- A neuroma is a typical result of peripheral nerve damage or amputation, and it can produce massive discomfort that is often resistant to most pain relievers. Neuromas are not malignant thickenings of nerve fibers made up of non-conducting tissue that prevents signals from being transferred along the nerve. Potentially restricting complications of nerve regeneration, neuromas can cause pain or hypersensitivity. Because the neuroma stimulates the nerve it contains, pressure or movement of nearby tissues can typically produce discomfort in the affected area.
- Muscle Weakness:
- Muscle care is particularly essential to preventing muscle injury, including heat or cold stress, overstretching due to gravity or inappropriate lifting/transfer procedures, and muscular contractures. When performing muscular strengthening exercises, it is essential not to injure the recovering neural tissue: if pins and needles, numbness, or increased discomfort occur, the exercise is too severe and advanced too soon, it may hamper recovery.
- Psychological Stress:
- Peripheral nerve injuries can cause muscle weakness, contractures, deformity, and discomfort, leading to psychological stress.
- Chronic neuropathic pain is severe, producing emotional stress, a worse quality of life, and an increased risk of posttraumatic stress disorder, depression, or anxiety. The aim is not just to relieve pain, but also to enhance quality of life, which can only be accomplished by addressing depression, anxiety, and sleep disturbances.
Diagnosis
To properly determine the level of nerve injury, the doctor may perform an electrical conduction test, which measures the passage of electrical currents in the nerves. These tests include nerve conduction velocity (NCV) and electromyography (EMG). These tests are occasionally performed during real surgery while the patient is asleep.
The doctor can also request any of the following imaging techniques:
- CT scan
- MRI
- MRI neurography
Treatment
- Depending on the degree of peripheral nerve damage, treatment options include surgical repair as well as conservative approaches such as physiotherapy.
- Non-surgical therapies for minor nerve damage may include the following options
- Medication
- Physical therapy and rehabilitation
- Acupuncture
- Orthotics
- Massage therapy
- Occupational therapy
- Electrical stimulation therapy
Medication for peripheral nerve injury
Treatment for peripheral neuropathy may involve treating any underlying causes or symptoms.
- For certain underlying issues, treatment may be more effective. For example, keeping diabetes under control can help to improve or prevent neuropathy from worsening.
- There are several causes of peripheral neuropathy, and some of them can be treated in various ways.
- Lifestyle adjustments, such as quitting smoking, dropping alcohol use, keeping a healthy weight, and exercising frequently, can help manage diabetes.
- Vitamin B12 deficiency can be addressed with pills or injections.
- Certain kinds of peripheral neuropathy can be treated with medications, including steroids, which are strong anti-inflammatory agents.
- Immunosuppressants are medications that limit immune system activity, whereas immunoglobulin injections are a combination of antibodies produced by the immune system.
- However, the root problem may not always be curable.
Relieving nerve pain
- You may also need medication to relieve any nerve pain (neuropathic pain) you are experiencing.
- Unlike most other forms of pain, neuropathic pain does not generally improve with basic pain relievers like paracetamol and ibuprofen, hence additional medications are frequently utilized.
- Typically, they should be begun at the lowest possible dose and progressively raised until an effect is shown.
- Higher dosages may provide better pain relief, but they are also more likely to induce negative effects.
- Tiredness, dizziness, and a sense of being “drunk” are the most typical adverse effects. If you experience any of these, your dose may need to be reduced.
- The negative effects will disappear within a week or two as your body adjusts to the medication.
- However, if your adverse effects continue, talk to your doctor since it may be possible to switch to a different medication that works better for you.
- Even if the initial medication does not work, other options may.
- Many of these medications can also be used to treat other medical disorders like depression, epilepsy, anxiety, and headaches.
- Even if you are not depressed, using an antidepressant may help with your discomfort. This does not imply that the doctor thinks you’re depressed.
- The major drug indicated for neuropathic pain is amitriptyline, which is also used to treat headaches and depression.
- Duloxetine is used to treat bladder issues and depression.
- Pregabalin and gabapentin are used to treat epilepsy, migraines, and anxiety.
- There are also some more medications that you can take to reduce pain in a specific location of your body or to reduce extremely acute pain for a short time.
Capsaicin cream
- If your pain is limited to one area of your body, you may benefit from applying capsaicin cream.
- Capsaicin, the ingredient that makes chili peppers bright, is considered to help with neuropathic pain by preventing neurons from delivering pain signals to the brain.
- Apply a pea-sized dose of capsaicin cream to the sore region of the skin three to four times each day.
- At the beginning of therapy, capsaicin cream may cause skin irritation and a burning sensation in the treated region.
- Do not use capsaicin cream on injured or inflammatory skin, and always wash your hands after using it.
Tramadol
- Tramadol, a strong analgesic similar to morphine, can be used to treat neuropathic pain that does not respond to other therapies prescribed by a doctor.
- Like all drugs, tramadol has the potential to become addictive over time. It’s normally only given for a short period.
- Tramadol might be helpful to use when your pain is severe.
- Common side effects of tramadol include:
- feeling sick or vomiting
- dizziness
- constipation
Treating other symptoms
- In addition to pain relief, you may need medication to address additional symptoms.
- For example, if you have muscle weakness, you may require physiotherapy to learn exercises to increase muscle strength.
- You may also need to wear splints to assist your weak ankles or use walking aids to move about.
other issues connected with peripheral neuropathy may be treated with medication
For example:
- erectile dysfunction
- constipation
- Gastroparesis is the poor movement of food through the stomach.
In some situations, you could require additional therapy, such as:
- botulinum toxin injections for excessive sweating (hyperhidrosis)
- If you struggle to empty your bladder, you may require additional therapy, such as a urinary catheter.
Physiotherapy treatment for peripheral nerve injury:
Aims
- counseling
- decreases the pain
- decrease the tingling numbness
- decrease muscle spasms and cramps
- prevent contracture and deformity
- improve muscle strength
- improve balance and coordination
- improve the sensation
- improve quality of life
Pain relief
- Acupuncture, TENS, Laser, massage, and Relaxation techniques can all help to reduce the pain associated with these conditions.
- Neuropathic pain reduces quality of life and is a typical result of nerve injury.
- It is critical to manage pain properly.
- Complete reduction is unusual, and 40-60% discover ways to get partial relief.
- Anticonvulsants and tricyclic antidepressants are the most popular drugs used to treat neuropathic pain.
- A Physical therapist may employ additional pain-relieving techniques. Massage, such as aromatherapy, may help neuropathic pain.
- Transcutaneous Electrical Nerve Stimulation (TENS). TENS lower discomfort in neuropathic pain. It was shown to be effective when used at 100 Hz in continuous mode.
- Low-level laser therapy (LLLT). Studies have shown that this can help with pain reduction and healing in the treatment of neuropathic pain and neurological impairments as an additional form of therapy.
- Relaxation techniques
- Acupuncture
muscle Weakness
- Denervation causes muscular atrophy and functional impairments. The neurological regulation of muscles requires a healthy neuromuscular junction (NMJ). Numerous studies have shown that TENS improves NMJ health and prevents muscular atrophy.
- Muscle care plays an essential role in reducing muscle injury, including heat or cold pressure, overstretching due to gravity or inappropriate lifting and transfer procedures, and muscular contractures.
- Muscle weakness can be strengthened with appropriate and graded muscle-strengthening exercises based on the severity, time, and type of the injury.
- This may use
- electrical stimulation
- actively assisted
- isometrics
- supported straps that assist in the strengthening process.
Sensory education
- Functional and sensory impairments Learning functional tasks involves using the brain to improve visual-tactile and auditory-tactile relations. The upper arms are mostly used for collecting fine motor skills.
- Sensory reeducation helps to the rehabilitation of awareness. grasping and touching, as well as brushing and icing, are common methods of sensory stimulation
- Balance and coordination are essential in the lower limbs.
- Techniques are employed to activate several sensory systems.
- Massage
- US
- hydrotherapy
- splints
- passive range of motion stretches
- accurate transfer skill instruction are some techniques physical therapists utilize to achieve the desired aims.
- When muscular strengthening activities may begin, it is critical not to harm the recovering nerve tissue. If you get pins and needles, numbness, or extreme pain, the workout is too difficult and can affect healing
Muscle-strengthening
- exercises are added as needed,
- such as isometric
- Hold and Relax Exercise
- graded weight progression
- Weight cuff, Theraband, and Dumbles can be used in weight-bearing exercise
- open-close chain, and
- Moderate-intensity exercise promotes strength and physical function.
- Nerve gliding activities are movements demonstrated by a Physical therapist to assist you to move and glide your nerves.
Proprioception impairments
- Proprioception exercises use exercise and other methods to improve joint position and balance in the limbs.
- It can be corrected by employing balancing pads for weight-bearing exercises, exercise balls, and bouncing balls for upper limbs and gym bosu ball
- Reach out
- equilibirium and non equilibirium method
- yoga
Balance and coordination activities –
- Your physical therapist develops ways of improving your balance and coordination. Improving balance and coordination reduces your chance of falling and the injuries that result from it. Balance exercises are an important aspect of the rehabilitation from peripheral neuropathy. Balance exercise is essential for overcoming feelings of stiffness and unsteadiness, especially in aged people.
- Education – Your physiotherapist will advise you on how to safely treat peripheral neuropathy. It mostly focuses on increasing your safety, avoiding extra problems, and identifying alternate ways to do particular jobs.
- Kinetic treatment in peripheral nerve injuries shouldn’t start until the last stage of nerve regeneration, when gradual strength recovery may be noticed. After a nerve injury, physiotherapeutic procedures can be used to treat paresis, restore normal muscular function, and increase circulation.
Electrostimulation
- Electrostimulation plays a significant part in the treatment of different neuromuscular disorders.
- Magnetotherapy is a treatment in which a pulsed low-frequency magnetic field is delivered. It has well-known effects on enhancing enzyme activity, oxy-reductive processes, and healthy blood circulation, resulting in improved oxidation and conduction. characteristics of regenerating peripheral nerves.
- Galvanic and faradic current helps to strengthen the muscle.
Joint Stiffness:
- If the soft tissues in the area and surrounding areas supplied by the injured nerve remain in shortened postures, they are at risk of contractures. Daily passive range of motion exercises are beneficial in preventing these issues, and protective removable static splints can also help avoid contractures.
- Ultrasound and laser therapy have been proven to be beneficial in treating tight joints.
Emotional Stress:
- Chronic neuropathic pain is severe, producing emotional stress and a worse quality of life. According to a patient with neuropathic pain is essential for good treatment. The final goal is to improve one’s quality of life rather than only decrease discomfort. This can only be done if depression, anxiety, and sleep issues are all treated.
- Relaxation Techniques may help to reduce stress.
Ergonomic cast and splints:
- If you have neuropathy that affects your muscles, ergonomic casts and splints can assist. Splints can assist with muscular weakness.
- These casts provide support to the area of your body that is painful. This can help ease the pain. A splint or cast, for example, can ease one’s suffering from carpal tunnel syndrome by holding their wrists in the right place while they sleep.
- Splinting and bracing – The use of a splint or brace to support the joint and prevent overstretching or contractures the use of support slings to help mobility and bear the weight of the limb.
- Additionally, splinting techniques—such as postoperative splinting and casting—as well as splints to halt deformities from growing or correct developed contractures and improve function are commonly employed in the care of peripheral nerve injuries and aid in the patient’s rehabilitation.
- Static and dynamic splints can assist paralyzed muscles rest in the best possible posture, preventing overstretching and contractures. They also assist unaffected muscles in operating from proper postures.
Self-care:
- Many have used electric footwear or heating pads, applied packs of ice to the affected areas twice daily for fifteen minutes each, tried acupuncture, underwent biofeedback, and used a variety of holistic therapy techniques such as reflexology, tai chi, or reiki in addition to these methods for managing their pain and finding relief from peripheral neuropathy. In order to enhance circulation, they have also found comfort in massaging the areas that are affected.
- Avoid pressure on the afflicted region, such as not crossing legs or bending on elbows. Looking for social support and participating in activities with others, explaining daily priorities and not doing more than you believe you are capable of, avoiding caffeine, and having a regular evening routine that promotes sleep.
- Moderate, consistent exercise could be beneficial for pain.
- Consider quitting or reducing your intake of alcohol and tobacco.
- Both alcohol and tobacco worsen nerve discomfort and can cause nerve damage if used for a prolonged period
Surgical management
During surgery, the injured nerve segment is removed, and the surgeon attempts to reconnect the healthy nerve ends. In certain situations, a nerve from another region of the body is transplanted (nerve graft). Physiotherapy is used to treat several types of peripheral nerve injury.
- Physiotherapy management is also recommended following surgical treatment for this issue
- Management begins with a complete history and examination of the injury.
- A neurosurgeon may do peripheral nerve surgery to treat more serious damage.
Procedures include:
- Carpal tunnel surgery
- Brachial plexus surgery
- DREZ procedure
- Free muscle transfer
- Nerve repair or nerve graft
- Nerve entrapment surgery
- Nerve sheath tumor surgery
- Nerve transfer surgery
- Nerve transplant surgery
- Open decompression surgery
- Sensory nerve surgery (for meralgia paresthetica)
- Thoracic outlet syndrome surgery
Indications of surgery
Nerve grafting
- Neurotmesis (3rd-5th degree)
- Early surgical examination includes accidental damage, penetrating trauma, blood vessel damage, and progressive disabilities. Gunshot wounds that affect the brachial plexus may cause neurotmesis one to three weeks after damage, allowing time to identify the zone of harm.
- Indications
- Cracks that restrict tension-free direct repair
- Nerve transfer
- Indications
- Proximal nerve injury
- The goal is to give fresh axons and stimuli before motor endplate damage and permanent muscle injury
- Restoring shoulder abduction and external rotation, as well as elbow flexion and finger function, is the first focus.
- Tendon transfer
- Indications
- The return of function through nerve regeneration is not occurring due to problems of tendon transfer, which may result in greater scarring and blood supply damage
Alternative and complementary therapies
Because peripheral neuropathy can be a painful and difficult condition that is only partially decreased by current treatments, you might want to explore different options.
This may include:
- Acupuncture,
- herbal medicine.
- Benfotiamine (a kind of vitamin B1) supplements
- Alpha-lipoic acid (antioxidant) supplements
- However, while some people may find them useful, the data supporting them is not always clear.
- Consult your doctor before starting these remedies, since they might interfere with your current therapy
Precautions
- If you have peripheral neuropathy, you might become more prone to accidents at home.
Do’s
- Use safety guards and other equipment while holding sharp devices such as scissors and knives.
- Use thermometers to determine the temperature of the bath & tap water.
- Handle hot goods with potholders and gloves.
- wear a hand or foot orthosis for maintaining a posture and stability
- Use a walker and a cane for extra stability.
- Use lights to avoid falling in the dark.
- When it is cold outside, carefully wrap your hands and feet.
- take a healthy diet to maintain or control your body’s sugar level
- always change the position to maintain mobility and prevent pressure sore
- use modified objects to ease your work
- use velcro tape or chain instead of buttons
- use splints to prevent contracture or deformity
Don‘t’s
- don’t smoke or drink it will delay your healing
- don’t use sharp objects
- don’t use a hot pack as if you’re unaware of the sensation
FAQ
Can a traumatic fall cause nerve damage?
Peripheral nerves can be injured in several ways: Injury from an accident or a fall from a height A fall on an outstretched hand or a fall on the shoulder can cause injury to the brachial plexus, which can stretch, compress, crush, or cut off nerves.
How can someone strengthen the nerves?
Follow a nutritious diet. A well-balanced diet promotes a healthy neurological system.
Control your alcohol intake and quit smoking (if you haven’t already).
Exercise regularly.
take precautions at home
and wear orthosis for better support and to prevent deformity or contracture
Keep your diabetes under control
Get your medications examined
Can exercise repair nerve damage?
Physical exercise-based rehabilitation has been shown to aid PNI recovery by stimulating nerve regeneration and decreasing pain.
What makes nerves repair faster?
Exercise is essential during rehabilitation since it helps your muscles restore function and increases blood flow throughout your body. This, in turn, speeds up nerve repair. Similarly, inactivity affects progress. You don’t want to overuse it, but moving your muscles is beneficial.
References
- Classification of peripheral nerve injury. (n.d.). Physiopedia. https://www.physio-pedia.com/Classification_of_Peripheral_Nerve_Injury
- Peripheral nerve injury. (2022b, May 4). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/peripheral-nerve-injury#:~:text=Peripheral%20Nerve%20Injury%20Symptoms,affected%20by%20the%20damaged%20nerve.
- Brachial plexus injury – Symptoms and causes – Mayo Clinic. (2022, June 3). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/brachial-plexus-injury/symptoms-causes/syc-20350235
- Brachial plexus injuries – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/brachial-plexus-injuries/
- Brachial plexus injury. (n.d.). Physiopedia. https://www.physio-pedia.com/Brachial_Plexus_Injury
- Radial nerve palsy: Causes, symptoms, and treatment. (2024, February 3). Centeno-Schultz Clinic. https://centenoschultz.com/condition/radial-nerve-palsy/
- Wikipedia contributors. (2024, February 15). Foot drop. Wikipedia. https://en.wikipedia.org/wiki/Foot_drop
- Carpal tunnel syndrome – symptoms and treatment – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/carpal-tunnel-syndrome/
- Tarsal Tunnel Syndrome. (n.d.). Physiopedia. https://www.physio-pedia.com/Tarsal_Tunnel_Syndrome
- Bates, T., MD. (n.d.). Peripheral Nerve Injury & Repair – hand – orthobullets. https://www.orthobullets.com/hand/6066/peripheral-nerve-injury-and-repair
- Professional, C. C. M. (n.d.-p). Peripheral neuropathy. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/14737-peripheral-neuropathy
- Thoracic outlet syndrome – Symptoms and causes – Mayo Clinic. (2023, September 26). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/thoracic-outlet-syndrome/symptoms-causes/syc-20353988
- Website, N. (2023b, December 15). Treatment. nhs. uk. https://www.nhs.uk/conditions/peripheral-neuropathy/treatment/
- Jersey, P. C. O. N., & Jersey, P. C. O. N. (2021, December 13). Do’s and Don’ts for Dealing with Peripheral Neuropathy. Podiatry Center of New Jersey. https://podiatrycenternj.com/2021/12/dos-and-donts-for-dealing-with-peripheral-neuropathy/
- Classification of peripheral nerve injury. (n.d.-b). Physiopedia. https://www.physio-pedia.com/Classification_of_Peripheral_Nerve_Injury



2 Comments