Steppage Gait
Introduction
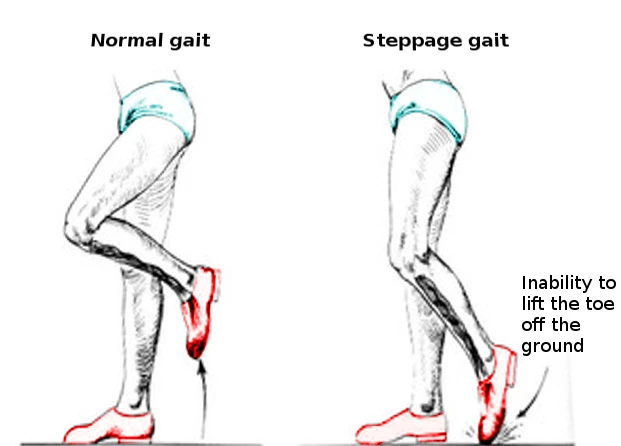
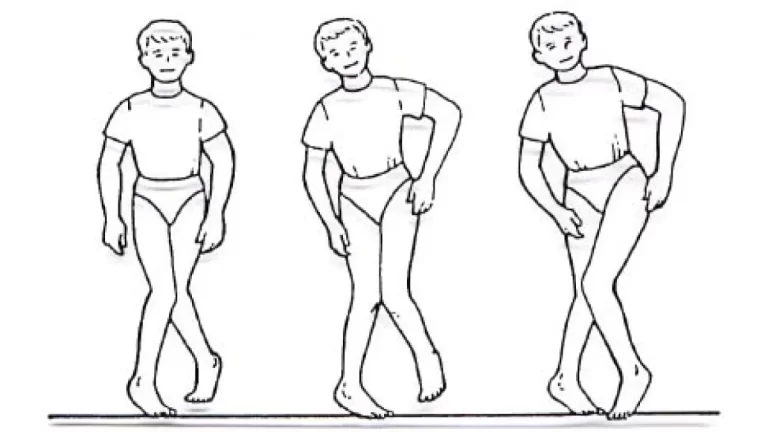
Steppage gait, which is additionally known as high stepping or neuropathic gait, is an improper gait type that results in foot drop or ankle equinus because of its absence of dorsiflexion. When walking, someone must elevate their leg higher than usual because the foot hangs with the toes facing downward, scraping the ground.
Foot drops could be caused by disruption to the deep fibular nerve. This pattern of walking is frequently observed in people with peripheral neuropathy, spinal cord injuries, muscular dystrophy, multiple sclerosis, neurological disorders, or other conditions that cause nerve loss or muscle weakness in the lower limbs. Steppage gait is often treated by addressing the underlying source of the difficulty, which may entail surgery, physical therapy, or bracing.
What is Steppage Gait?
- A sign of an irregular gait or walking pattern is steppage gait, which is defined by excessive toe and foot raising during the walking swing phase. Various other names for it include foot drop gait or drop foot gait.
- The foot is raised and the toes are pointed upward during the swing phase of normal walking to clear the ground. In contrast, in patients with steppage gait, the muscles that lift the foot and toes are either weak or paralyzed, giving in a high-stepping gait in which the foot is raised higher than necessary to clear the ground.
- One reason that leads to the Steppage gait is the trouble in elevating the foot when walking due to decreased muscle strength regulating the ankle joint’s dorsiflexion. Comparable to foot drop, however, foot drop is uncommon. When the muscles that lengthen the foot when walking suddenly weaken, this is the typical appearance of the patient.
- The medical record usually comprises a fracture-causing incident, prolonged inactivity, unusual behaviors, surgical procedures, or a lower limb in a severely tight cast. A previous diagnosis of collagen vascular disorders resulting in nerve ischemia is one of the additional factors. Foot drop is an additional indicator that upper motor neurons have been damaged.
- The most common cause of peripheral neuropathies, which can result in either unilateral or bilateral foot drops, is diabetes. The same justification applies to hemiplegia and aphasia.
Statistics
- Men are typically more likely than women to be suffering from peroneal neuropathy; their probability is 2.8 to 1. Ninety percent of peroneal lesions are unilateral, meaning they don’t favor one side over the other.
- The incidence after total knee arthroplasty (TKA) varies between 0.3 and 4%.
- Three to thirteen percent of patients may experience foot drop following proximal tibial osteotomy.
What causes the Steppage Gait?
- People with lower limb nerve injury or muscle weakness, such as those suffering from peripheral neuropathy, spinal cord injuries, muscular dystrophy, or multiple sclerosis, frequently exhibit this kind of stride.
- Additionally, several neurological illnesses that influence the neurons controlling the ankle and foot muscles may be contributing factors.
- Foot drop occurs when the anterior tibialis muscle, which is situated in front of your shin bone, weakens or paralyzes.
- Among the most prevalent causes are injuries caused by trauma, pelvic bone fractures, tibia or fibular head fractures, tightened plaster casts, long-term lithotomy positioning during surgical procedures, compression from a space-occupying lesion, vascular impairments like those linked to lupus, or Waldenstrom macroglobulinemia, which can result in vasculitis and nerve ischemia.
- Primary demyelinating neuropathies can also be inherited or hereditary. They may be largely demyelinating, mostly axonal, or a combination of the two.
- Primary demyelinating neuropathies, whether acquired or congenital, are also common.
- Toxin exposure to radiation, infections from bacteria or viruses, and chemotherapy medications like vincristine or vinblastin are the primary contributors to axonal neuropathies.
- Combined peripheral polyneuropathies can result from several illnesses, including diabetes, alcoholism, and renal failure.
- Amyotrophic lateral sclerosis and cerebrovascular accidents (CVAs) are the two primary sources of foot drop.
- Cerebrovascular accident (CCA) symptoms include dysphagia, dysarthria, and hemiplegia or hemiparesis.
- The “cock-walk gait,” which is the screening of the upper motor neuron type, has a high steppage stance and a drop in the foot.
What are the signs of Steppage Gait?
- People who walk with a steppage stride may show.
- A foot that is raised excessively even with walking.
- The dragging of toes.
- A gait that is awkward or erratic.
- Heightened the chance of falls and trips.
- Foot drop (incapacity to elevate the forefoot).
What is the diagnosis of the Steppage Gait?
- In the event of trauma, the diagnostic evaluation should include routine X-rays of the pelvis and tibia or fibula to identify any fractures or dislocations.
- \When plexopathies are suspected, the results of an MRI may be suggestive.
- Rheumatoid factor, an antinuclear antibody (ANA), and other relevant laboratories should be investigated in patients with collagen vascular disease.
- To rule out sepsis, the total blood count, differential count, and SMA 18 should be taken into account.
- Electromyography (EMG) and nerve conduction velocity (NCV) investigations will discover denervation potentials and motor units. Peroneal neuropathy has nothing to do with tibialis posterior weakness; instead, it is triggered by lumbar plexopathy, a lumbosacral trunk lesion, and L5 radiculopathy.
- It is easier to differentiate the lateral trunk of the sciatic nerve involvement in peroneal neuropathy from the short head of the biceps because that portion is weaker over time. For an evaluation of both of these muscles, EMG is beneficial.
What are the treatments for the Steppage Gait?
Conservative Treatment
Medication:
Medications may be recommended to treat any underlying medical conditions that may be the cause of the steppage gait.
For ailments such as peripheral neuropathy or multiple sclerosis.
Physical Therapy:
Physical therapy recommendations for pain management, ankle range of motion (ROM) exercises to prevent stiffness, and strengthening exercises for weak muscles are all crucial in moderately intense circumstances.
Surgical Interventions:
When there are serious nerve damage or structural problems surgery may be necessary.
- Nerve Decompression: If nerve compression is the root of the steppage gait, the pressure can be released surgically.
- Tendon Transfer: A healthy tendon is transferred to improve the anterior tibialis muscle’s function.
- Ankle Fusion: In certain situations, the steppage gait can be corrected by fusing the ankle joint.
Physical therapy for the Steppage Gait
Physical treatment is essential to regulating steppage gait.
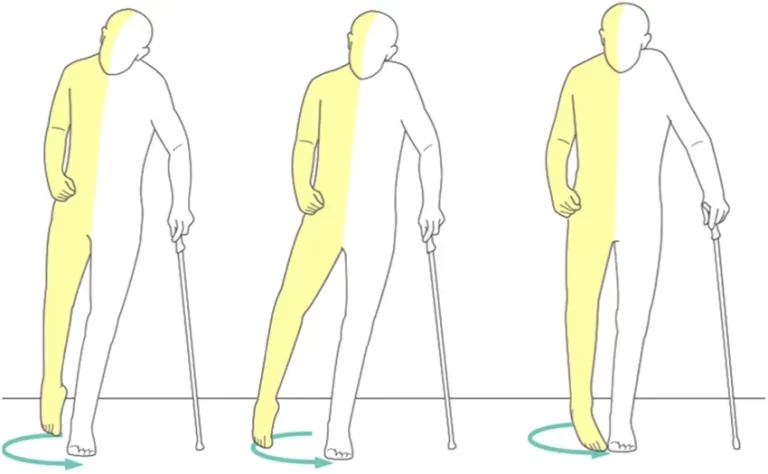
- Gait training teaches appropriate walking strategies to correct foot drop.
- Balance and coordination training helps to improve overall stability and reduces the danger of falling.
- Stretching helps to maintain lower-limb flexibility.
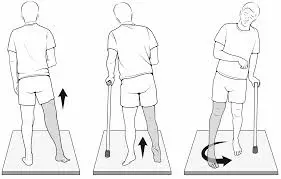
- Assistive devices, such as canes or walkers, may be advised for increased mobility and safety.
Exercises for the Steppage Gait
Dorsiflexion
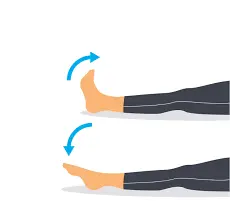
- Flexing your ankle forward toward the surface of your shin is known as ankle dorsiflexion, and it’s a basic ankle-strengthening exercise. This step will bring back your ability to walk properly.
- Start by adjusting your knee.
- Simply point your foot down near your nose while moving your ankle. Continue until you feel pain or can walk correctly with the assistance of this action.
- Hold this position for fifteen seconds.
- Return to your normal posture now.
Plantar flexion
- Your ankle goes downward and outward when your plantar flexes. Increasing your range of motion (ROM) might be feasible.
- To start Adjust your knee.
- All you have to do is stretch your ankle by directing your foot moving forward. Keep doing this until you feel uncomfortable or you’ve reached your limit.
- Hold this position for fifteen seconds.
- Restore your position to normal.
Inversion
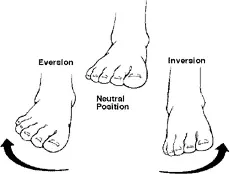
- When you point your ankle inside near your body, you execute an inversion. To turn your foot internally, move your ankle upward while preserving your toe pointed.
- The bottom of your foot should be facing the opposing leg. Until you start to experience pain or can no longer bend your foot inward, continue going.
- Hold this position for 15 seconds.
- Return to your typical position.
- Inversion and eversion
Eversion
- It is the motion of the ankle, which encompasses the leg’s outward movement. This exercise will aid in increasing your ankle’s range of motion.
- Continue your toe pointing and slowly rotate your ankle to turn your foot away from your other leg.
- Continue this exercise until you either lose the ability to turn your foot outward or start to feel pain.
- Hold this position for 15 seconds.
- Return to your normal posture now.
Calf-raising while seated

- By using partial weight-bearing in these exercises, you can put extra strain on the damaged ankle.
- They also aid in strengthening the ankles. Ten repetitions of this should be made in a single set of exercises.
- You must be in a comfortable seat with your injured foot resting on the ground.
- Try to lift your heel as high as you can while preserving your steady posture.
- Return your heel to the floor.
Weight shifting while standing.

- Initially, you may need to lessen the weight you put on the wounded leg. This ensures that your ankle is safe while it repairs.
- After that, you can progressively raise the weight on your wounded ankle. Because weight changes strengthen the ankles, they are perfect for this kind of workout.
- You can stand up straighter if you hold onto something sturdy.
- Your affected foot must carry some of your body weight.
- Hold the position for 15 seconds.
One leg Standing

- By doing these ankle-strengthening exercises, you can put greater weight on the wounded foot. Make sure your ankle can handle the strain before putting all of your weight on it. Lift the normal foot off the ground and stand on the damaged foot.
- Hold the position for 15 seconds.
- As you return your weight to your strong foot, maintain your center of gravity.
- Perform every ten times in a row.
Calf raising in standing
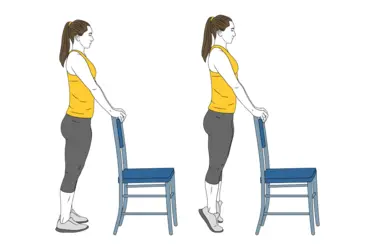
- Once your complete body weight can be maintained, try calf raises.
- Raise the healthy foot off the ground and place it on the foot that is injured.
- As you get up, lift your heel off the ground and place your foot just on the injured foot’s ball.
- Hold the position for 15 seconds.
- Restore your weight to your strong foot while maintaining your sense of equilibrium.
Sidestepping
- Stepping from side to side is an exercise that strengthens the ankles. Lay a rolled towel or other short object on the ground next to the injured foot.
- While standing on the suffering foot, cross over the towel.
- Then use your uninjured foot to cross over the stuff and raise yourself.
- When you step back over the towel, stay on the foot that is not injured.
- After that, stand up straight with both feet and cross the injured foot over the towel once more.
- As your recuperation advances, you can intensify this workout.
Neuromuscular Electrical Stimulation
- Foot drops are frequently treated using neuromuscular electrical stimulation (NMES), a form of electrical stimulation. It is a type of electric stimulation that helps your muscle learn to contract correctly again by artificially contracting it.
- When using NMES, your therapist will probably mention a few basic steps.
- The basic process is as follows.
- Keep your anterior tibialis muscle visible at the front of your shin.
- Your physical therapist will apply tiny adhesive electrodes on the front of your shin.
- After that, an electrical stimulation device will be linked to the electrodes.
- Your physical therapist will next activate the equipment and raise the stimulation level.
- Your shin’s front may probably begin to tingle.
- Until you can see your anterior tibialis muscle contracting, you should increase the intensity. Your ankle will inadvertently flex upward.
- Try to raise your ankle and toes even higher while using the NMES device to bend your ankle.
Use of Assistive Devices
Ankle-foot orthoses

- To help you walk correctly, your physical therapist could suggest that you utilize an aid. For this, a wheeled walker or a quad cane, which has a base with four modest feet, can be utilized. The proper use of your aid can be verified by your physical therapist.
- Sometimes you may become permanently paralyzed by your anterior tibialis muscle. If so, you may benefit from a specific kind of brace called an ankle-foot orthosis (AFO).
- By helping to lift your foot and toes off the ground, this brace reduces the chance that you will trip over your toes. You should no longer have a high steppage stride when you wear an AFO.
Elastic Band
- As a short-term solution for anterior tibialis weakness, raise your foot when walking with an elastic band.
- Tie the band around your leg just below the knee and wrap it around the ball of your foot. As you swing your leg forward, the elastic band keeps your foot up. Raising your toes off the surface no longer requires a high step.
- Naturally, wearing an elastic band around your leg all day might not be feasible. However, you can continue to move securely if you use it as a temporary solution.
Summary
The excessive lifting of the foot and toes during the swing phase of walking is a characteristic of steppage gait, a form of aberrant gait or walking pattern. With the correct diagnosis and a comprehensive treatment plan that includes physical therapy, patients can improve their walking patterns and reduce their risk of falling, even though steppage gait can seriously reduce movement and living standards.
FAQs
What is the difference between a slap gait and a steppage stride?
When the foot touches the ground, the gait becomes slapping. Occasionally, when walking, he attempted to raise his thigh to clear his toes, resulting in a steppage stride.
Which muscle is weak with a steppage gait?
Steppage gait requires a greater-than-normal bending of the knees, which raises the feet off the ground. Muscle atrophy and weakness typically affect the intrinsic foot and peroneal muscles as well as the leg muscles.
For what reason does steppage gait happen?
Although most people think that this disorder is related to foot issues, it is caused by a spinal injury or underlying condition. Steppage gait and drop foot are frequently caused by: ALS, amyotrophic lateral sclerosis MS, or multiple sclerosis.
What is the steppage gait known by another name?
A type of gait anomaly known as steppage gait (high stepping, neuropathic gait) is characterized by foot drop or ankle equinus as a result of lost dorsiflexion.
What kind of nerve injury results in a high gait?
Muscle atrophy or peroneal nerve injury (from spinal stenosis or a herniated disc, for example) can result in steppage gait.
References
- Patel, D. (2023c, May 5). Steppage Gait – Cause, Symptom, Treatment, Exercise – Samarpan. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/steppage-gait/
- Wikipedia contributors. (2024a, May 5). Steppage gait. Wikipedia. https://en.wikipedia.org/wiki/Steppage_gait
- Nori, S. L., & Das, J. M. (2023, August 7). Steppage Gait. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK547672/