Patella Alta
Introduction
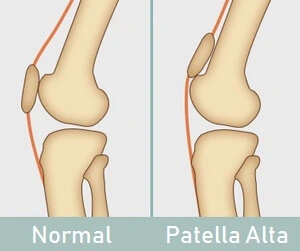
Patella Alta, commonly referred to as a high-riding patella, is a condition in which the kneecap (patella) is positioned higher than its normal alignment in relation to the femur.
- As a result, the knee loses stability and becomes more vulnerable to anterior knee pain and dislocation.
- Patella alta is usually a congenital disorder, but it can sometimes come from injuries to the knee, like a ruptured patellar tendon.
- Here, we look at what patella alta is, why it’s a concern, typical causes and symptoms, diagnosis procedures, and available treatments.
What Is Patella Alta?
The quadriceps tendon surrounds the patellofemoral joint, which is made up of the kneecap lying in a dip on the front of the femur bone, or lower thigh bone. This dip is known as the patellofemoral groove, but it is also referred to as the patella groove, trochlear groove, or intercondylar groove. From the base of the kneecap, the patellar tendon connects the kneecap to the tibia or shin bone.
The groove is significantly shallower here than it is further down, so there’s only a very minor barrier on either side of the kneecap.
Why Is Patella Alta A Problem?
When the knee is bent and straightened, the patella usually travels up and down the middle of the patellofemoral groove. The patella is retained firmly in place because the good depth of the groove prevents the kneecap from moving sideways.
However, because the kneecap is positioned higher than normal in the shallower region of the groove, there is less sideways stability in the patella alta.
Consequently, during knee flexion, the patella is pulled sideways over the low edge of the groove, potentially resulting in partial or total dislocation. It is estimated that approximately 30% of cases of recurrent patella dislocation are caused by patella alta.
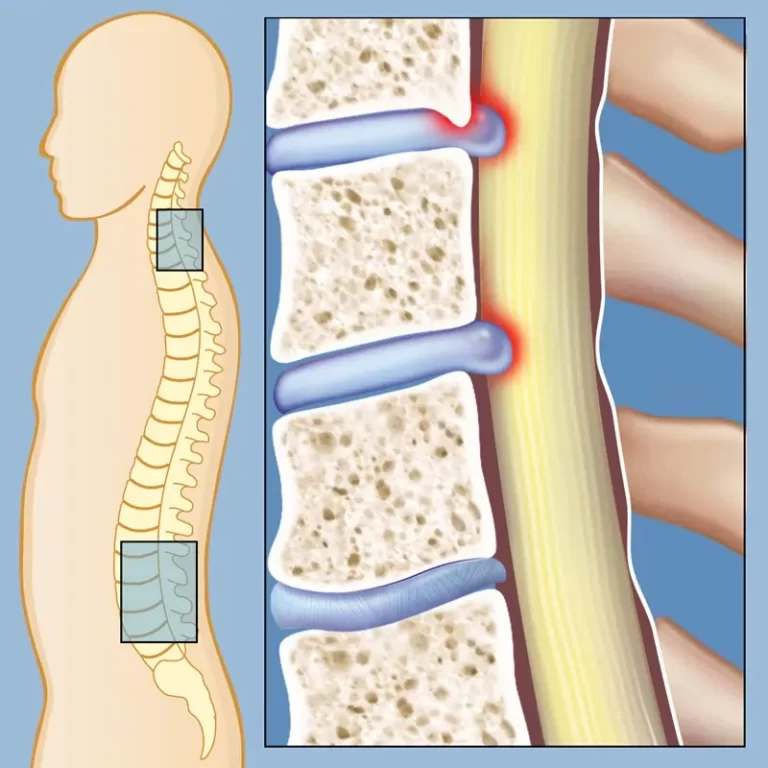
Patella dislocation or subluxation (partially dislocating) can cause chondromalacia and patellofemoral pain, commonly referred to as anterior knee pain.
Clinically Relevant Anatomy
The flat, triangular patella bone, which has one inverted corner, is situated in front of the knee joint. The patellofemoral joint is the region of the knee joint that lies between the patella and the femoral condyles. The patellofemoral articulation is absolutely necessary for the, which is attached to the patella by a common tendon, to function.
Another tendon is the patellar tendon, which connects the patella base to the tibia. These three bones are covered in articular cartilage, a very hard, smooth material designed to reduce forces of friction.
What Causes Patella Alta?
- The common causes of patella alta are as follows:
- Following a knee injury—typically a dislocated kneecap—patella alta may develop.
- Patella alta is most commonly observed in children who walk with bent knees and in conditions related to cerebral palsy and diplegia.
- Congenital defect: An embryo develops this flaw throughout development. An individual with this ailment has had patella Alta problems since birth.
- Long Patellar Tendon: Patella Alta is frequently seen by individuals whose patellar tendons are excessively long (more than 52 mm).
- Knee Injuries: A knee injury, usually a dislocation of the kneecap, may cause the Patella Alta to form.
- Brain palsy: Patella Alta is a frequent defect that may be associated with cerebral palsy, especially in children who walk with their knees bent.
- The patella alta may be brought on by an individual’s body structure. An individual with a tall build and a slender body type is most susceptible to this specific illness.
- Patella alta may result from patellofemoral pain. This particular ailment develops when a knee cap comes into contact with the thigh bone. A person who has this syndrome is more likely to develop patella alta disorder.
- Patella Alta can result from injuries to the knee. Given that playing sports and other physically demanding activities might cause the kneecap to pop out, this may be the main reason for the patella Alta’s medical condition. During the action, a quick shift in direction could make it happen frequently. A pulled-out kneecap would cause the patella to dislocate, which could lead to high-ride kneecap disorders.
- Patella Alta may also be caused by knee twisting. Any factor other than athletic activity, which is frequently linked to abrupt changes in direction, like jerks, could result in patella alta.
- Although sports injuries can cause patella alta, most cases of the syndrome are congenital or developmental in nature and unrelated to trauma. Although the etiology of patella Alta is not fully understood, excessively long patellar tendons (>52 mm) are thought to be one of the reasons.
Patella Alta Sign and Symptoms
Patella alta is a disorder when a person’s kneecap becomes dislocated and becomes abnormally positioned at the higher side of the femur bone. It produces few symptoms. This abnormality may result in a few distinguishable symptoms and indicators, such as:
- The patient may report pain in the patella region; however, as not all patella pain can be classified as a high-ride condition, accurate diagnosis is necessary for patella alta conditions.
- Patella alta is the primary cause of unsteady gait, hence anyone with unstable or irregular gait may have this disorder.
- Another severe indication of patella alta is a dislocated knee cap. The knee cap becomes painfully dislocated when the patella is bent more than it normally does, pulling the knee cap out of its natural grooves. The patella alta illness could be caused by any of these disorders.
The following are typical signs of patella alta:
- Instability: People who have patella alta frequently lament that their knee feels unstable or weak, especially when they’re running or walking.
- Recurrent Kneecap Dislocation: Individuals who have a high patellar tendon may frequently have knee dislocation. Few people have free will to freely push their kneecap in and out of the patellar groove, causing it to dislocate and subsequently reposition.
- It is particularly felt when crouching, walking up and down hills, sitting for extended periods of time, or climbing stairs.
- Sign of the camel’s back: the patella usually points forward. The patella points upward in people with high-riding patellas. The infrapatellar fat pad and tibial tuberosity are prominent in these patients, creating the appearance of an impact prominence akin to a camel’s back.
- The bilateral patella Alta allows for a better appreciation of the grasshopper’s eyes. A small number of patients may also exhibit patella Alta, lateral tilt, and externally rotated patellae.
Differential Diagnosis
First, your knee will be examined by your doctor to rule out patella alta. They will look at the connection between the femur and kneecap from different angles and with the knee in different configurations.
Patella alta is known to be associated with a wide range of illnesses, including:
- instability of the patellofemoral
- Patellofemoral dislocation recurring
- poliomyelitis and other neuromuscular disorders
- cerebral palsy that is spastic
- Osgood-Schlatter disease
- Sinding Larsen Johanssen Disease
- Friction syndrome of the patella tendon-lateral femoral condyle
- Chondromalacia patella
Outcome Measures
Since then, many approaches, such as those by Blackburne and Peel, Caton et al., and de Carvalho et al., have been developed in an attempt to categorize the patella position. Patella alta happens at higher ratios.
The Blackburne-Peel index can also be used to identify patella alta. The lengths of three surfaces must be measured in order to identify the presence or absence of a patella alta. The first length is a vertical line that ascends to the top of the inferior aspect of the patella articular surface from the horizontal line of the tibial plateau. The locations of both vertical lines are on the posterior aspect of the patella articular surface. The third length is shown as a horizontal line on the tibial plateau.
This technique is challenging to utilize with an MRI since it requires measurements across multiple areas. A ratio greater than one indicates the occurrence of patella alta.
The Caton-Deschamps index is a widely used radiographic tool for determining patellar height. This method is easy to measure on an MRI to determine the height of the patella. A normal patella ratio is between 0.66 and 1.33.
Diagnosis
Diagnostic Procedures
Although the cutoff values for both indices were rarely used on MRI, they were similar to those for conventional radiographs.
Physical Examination
Tests:
Full Knee Extension: When the knee is fully extended and relaxed, the kneecap can move very slightly from side to side.
Knee Slightly Bent: When the patella alta is flexed at a degree or so, it often displays the “camelback sign.” From the side, there are two humps that resemble the two humps on a camel. One is brought on by an upward-pointing high-riding patella, and the other by an expanded infrapatellar fat pad or bursa.
Knee Bent: When the knee is at a 90-degree right angle and the patella alta is present, the kneecaps point upward instead of forward and may be rotated, twisted, or tilted externally.
Fairbanks patellar apprehension test:
The positive test results indicate that lateral patellar instability is a substantial component of the patient’s problem. This may be so effective that when the therapist reaches for the knee, the patient pulls back on the leg or clutches the therapist’s arm to avoid contact.
Patellar glide test:
This test is used to evaluate the instability. A medial/lateral displacement of the patella with this test that is larger than or equal to three quadrants is consistent with ineffective lateral/medial constraints. Lateral patellar instability happens more frequently than medial instability.
Measurement of the patella alta
The following techniques are frequently employed:
- Install-Salvati ratio
- Modified Insall-Salvati ratio
- Blackburne-Peel ratio
- Caton-Deschamps index (knee)
- Blumensaat method
The Blackburne-Peel index
Using this technique, a knee lateral radiograph with 30 degrees of flexion is produced. Measurement of the lengths of three surfaces is required to determine the presence of a patella Alta. The horizontal tibial plateau line and the top of the inferior portion of the patella articular surface form the primary length, which is a vertical line. On the tibial plateau, the third length could appear as a horizontal line. This method needs measuring over multiple sections, which makes it challenging to apply on an MRI. A ratio of 0.5 to 1.0 is considered the typical value of the patella.
The Caton-Deschamps index
It is the radiographic method most frequently employed to assess patellar height. This is measured in 30 degrees of flexion on a lateral radiograph of the knee. It is the ratio of the length of the patellar joint surface to the distance between the upper limit of the tibia and the inferior aspect of the patellar articular surface. When the knee is flexed at a 30º angle on a lateral radiograph or sagittal knee CT or MRI reconstruction, the Caton-Deschamps index can also be determined. to measure the patella’s height.
Blumensaat technique
The lateral image of an x-ray taken at 30 degrees of flexion is also processed using this procedure. As a reference line, it makes use of the Blumensaat line or the roof of the intercondylar notch. It is reported where the patella’s lower pole is located in relation to the Blumensaat line. In a 30-degree flexion, the patella’s lower pole typically contacts this line. Additionally, the millimeter distance in millimeters between the lower patellar pole and the Blumensat line is indicated.
Complications in Patella Alta
The two primary problems associated with patella alta are instability and patellofemoral arthritis. An individual with patella alta is typically more susceptible to developing another patellar instability issue. The patella became involved around a flexion arc if the dislocation or bending was of a very elevated form. There is a bend of about 20 to 30 degrees at the angle. It suggests that the patella is not very stable over time.
However, the longer patellar tendon has a greater windscreen wiping effect, or more activity, as you can put it. Because of the patellar tendon’s growth, it becomes extremely unstable and slides side to side. Because of the elevated riding patella, pressure is placed on the kneecap, potentially resulting in greater wear and tear, articular cartilage injury, and knee pain. In the end, patellofemoral arthritis may also arise in a variety of circumstances.
Treatment:
Medical Treatment
A tibial tuberosity osteotomy may be necessary for patients with patella alta. The patellar ligament’s connection is transferred from the kneecap to the tibia during this treatment. Because the patella is attached to this ligament as well, it travels downward. Increased quadriceps angle can be related to patella alta; this can be corrected by inwardly shifting the patellar ligament’s bone attachment.
A few things that could happen after the procedure include infection, stiffness in the knee joint, injury to the nerves, and recurrent instability. Since pain and swelling will limit the knee’s range of motion, physical therapy and exercise should be performed following surgery to minimize these side effects. Your muscle control will also improve with physical therapy. You should take three to six months off while you heal.
Physical Therapy Treatment:
The patella’s resting height can be changed by manual gliding before knee extension, potentially alleviating knee pain. Tape can be used to fix the positioning problem with the patella, hence correcting patellar alignment. Patients stated that they were taking fewer medicines, that walking was not too difficult for them, and that their average pain level was a VAS score of 12.
Ice Packs: Using ice packs on a regular basis may also help with patella alta symptoms. Ice packs used for the knees can help relieve discomfort, swelling, and inflammation. They may also be helpful for long-term knee issues or injuries. These could be anything from single-use, throwaway packs to specialty ice packs and knee brace inserts with superior cryotherapy. The top ice wrap for you can be selected from the five varieties discussed below, or you can compare models and read reviews.
Knee Brace: The indications and symptoms of a high-riding patella may be lessened by using a brace while wearing one. To keep the brace from riding up, it should preferably feature a tubular section that rests above the kneecap. Knee braces come in a variety of fixing methods and support intensities. They also fluctuate widely in price and are available in a multitude of materials. Despite this, a study by Shellock et al. Patella, Alta, was present in four of the five knees in this study’s group that did not get better.
Patellar Taping: Taping can also be used to change the position of the patella. Taping is an often-used adjunctive or temporary method. Physiotherapists frequently use the tape to reduce the risk of recurrent injuries, enhance joint stability, increase athlete confidence, inhibit or facilitate muscle action, lessen the strain on damaged or vulnerable tissues, enhance proprioception, compress when edema is present, and encourage lymphatic drainage.
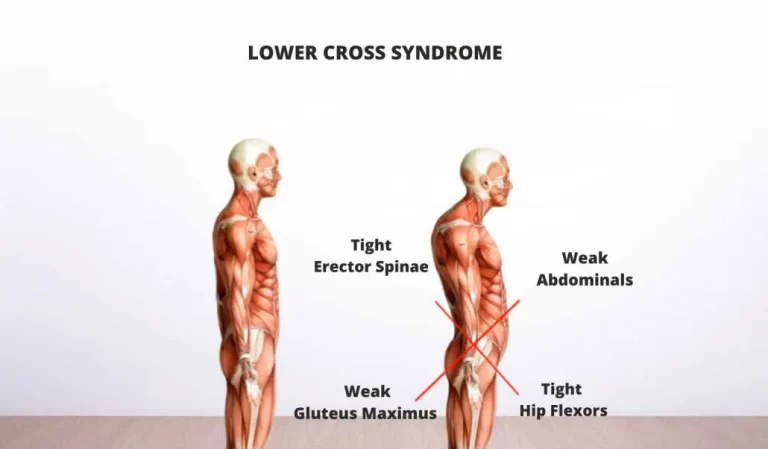
Strengthening the muscles in the buttocks, kneecap, and knee can help realign a high-riding patella, reducing pain and improving knee stability. Treatment for knee pain and prevention of recurrence can be achieved with exercise.
Quad crunches allow the knee to be fully extended while simultaneously maintaining and strengthening the quad muscles. knee or leg straight, Tighten the muscle at the front of your thigh by lowering your knee all the way. Your thigh muscles should be taut. Hold for three seconds. Repeat 10–20 times every 3–4 hours. If you are experiencing difficulty getting your knee to fully extend, try lifting your leg off the bed a little bit by rolling up a towel under your ankle. Next, carry out the exercise as instructed. The knee can straighten by being gently raised by gravity.
Short Arcs: With minimal knee movement, this exercise strengthens and improves control over the quadriceps muscles. Either lie flat on your back or sit up straight with your leg outstretched on a level surface, such as a bed. Place a cloth that has been folded up and roughly 10 cm in diameter under the knee and/or As you draw your toes nearer to your body, tighten your thigh muscles. Hold for three to five seconds, then gradually descend. Ten to twenty times, repeat. You can push yourself farther by increasing the weight by putting on a shoe or using a little ankle weight, for example, and increasing the difficulty level.
Straight Leg Raise (SLR): Assume a prone position, keeping your hips straight and your legs relaxed on the floor. With the foot flat on the floor, your unaffected leg should be bent at the knee to a 90-degree angle. As you gradually lower the leg to the floor, release the breath slowly. Repeat ten more times after unwinding. The movement should tighten your hips, thighs, and abdomen when done correctly.
The Clamshell: Lay on your side and stack your hips and feet. Bring your knees in close to your body until your feet are parallel to your butt. Put a hand on the other hip to keep it from sinking back. This is where you should start. Maintaining your abs firm and your feet together, raise one knee as high as you can without rotating your hips or raising the other knee off the ground. At the peak of the movement, engage your glutes and hold for one second before lowering one knee slowly to the starting position. After 20 total repetitions, switch to the other side and repeat.
Surgical Treatment
When conservative measures fail to relieve severe cases of patella alta, such as when the kneecap keeps dislocating, surgery becomes necessary, for patella alta, there are various surgical techniques available, such as:
At this moment, the patella and the patellar tendon attachment are pushed downward.
The tibial tuberosity is taken out of the front of the shin bone, shifted downhill, and then secured in place with wires and a screw during a tibial tuberosity osteotomy.
Lateral Release: Lateral release surgery can be used to loosen the excessively tight structures on the outside of the knee that are causing the patella to ride high. Go over the process in more detail in the section on lateral release.
A patellectomy, which is only advised in cases of severe patellofemoral arthritis or when all other surgical treatments have failed, involves the total removal of the patella.
FAQs:
Can the patella Alta be used for sports?
They frequently exhibit strong athleticism and seem to excel at basketball, the step and leap, and the high jump. The knee cap’s high degree of mobility and propensity for dislocation during sports activities are the patella Alta’s problems.
How can someone be diagnosed with patella alta?
The dislocation of the kneecap is the primary sign of patella alta. A dislocation may result from the patella bending more than usual, pulling the knee out of its groove. Because it wears down the cartilage, having a misplaced patella might lead to further problems with the patella.
What is the course of patella alta?
The patella will only engage in the trochlear groove later within the flexion arc (that is when the knee is bent beyond the typical 20 to 30 degrees) if the patella is sitting too high (patella Alta). This suggested that a higher proportion of time could see the patella becoming less stable.
Patella Alta: is it really real?
Patella Alta is assumed to be the source of recurrent patella dislocation in about 30% of instances. The cartilage on the back of the kneecap is susceptible to damage if the patella dislocates or subluxates (partially dislocates). This can also result in chondromalacia and patellofemoral discomfort, often known as anterior knee pain.
Is the patella alta a displacement?
People who have patella alta, or a patella or kneecap that is located higher up on the femur than usual, are also more likely to experience a dislocation since the patella should travel farther during knee flexion before fully engaging in the femur’s groove or track.
Is surgery necessary for your patella alta?
Surgery can be used to effectively treat a patient whose patella alta is causing them particular problems, such as instability and/or patellofemoral wear and pain, by moving the patella downward as much as is required to return it to its natural position.
Can a dislocation result from patella alta?
Patella alta (high riding patella), trochlear dysplasia or lateral femoral condyle hypoplasia, and severe lateral patella tilt are among the anatomical characteristics that contribute to dislocation.
How long does healing take after surgery for patella alta?
Most of the time, you can return home the following day with your knee immobilized in a brace. You should be able to support your own weight with the brace after about two weeks; most people can stand on their own without a brace after six weeks.
Do you have patellar tendon surgery scars?
You most likely won’t require crutches or a cane for almost a month after surgery, but a few days afterward you should be able to start walking and bearing some weight on your knee. Most of the time, the pain feels like you ran into a table.
Painful patellar surgery?
You will be in pain, but it should be tolerable. During the initial few days following surgery, a tiny amount of drainage may occur at the surgical site.
References
- Patel, P. (2023, December 13). Patella Alta – Cause, Symptoms, Treatment, Exercise. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/patella-alta/
- Darji, H. (2023, May 26). Patella Alta – Cause, Symptoms, Treatment, Surgery. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/patella-alta/#google_vignette