Deep Tendon Reflexes
Definition
Deep Tendon Reflexes (DTRs) are involuntary, automatic responses to a stimulus applied to a tendon, typically involving the muscle it is connected to. These reflexes are essential for assessing the integrity of the nervous system, particularly the motor and sensory pathways.
When a typical person taps a muscular tendon vigorously, the two-neuron reflex arc that involves the spinal or brainstem segment innervating the muscle causes the muscle to contract instantly. The efferent neuron is an alpha motoneuron located in the anterior horn of the cord, whereas the afferent neuron, whose cell body is located in a dorsal root ganglion, innervates the muscle or Golgi tendon organ connected with the muscles.
Gamma motoneurons in the anterior horn, which feed a set of muscle fibers that control the length of the muscle spindle itself, are a way by which the cerebral cortex and several brainstem nuclei influence the sensory input of the muscle spindles.
- Hyporeflexia is the lack of or reduced reaction to tapping. It typically denotes a condition affecting one or more of the elements that make up the two-neuron reflex arc.
- The term “hyperreflexia” describes clonic or hyperactive reflexes. These typically signify a suprasegmental lesion, or a lesion above the level of the spinal reflex pathways, which interrupts corticospinal and other descending networks that affect the reflex arc.
The deep tendon reflexes are conventionally ranked in the following order:
- 0 indicates no answer; this is always out of the ordinary
- 1+ indicates a faint but unmistakable reaction that might or might not be typical.
- 2+ is a quick reaction; typical
- 3+ A quick answer (3+) that might or might not be typical
- 4+ = a tap causes a clonus, a recurring reflex that is always absent.
The patient’s reflex history, the state of the other reflexes, and an examination of related findings such as muscle tone, muscle strength, or other disease-related indicators will determine if the 1 + and 3 + responses are normal or not. Reflex asymmetry points to abnormalities.
A physical examination might include testing many types of reflexes, and each test provides information about the health of the nervous system components that support the reflexes. Because of their safety, affordability, accuracy, and speed of execution even in the absence of specialist equipment, they have been a standard component of neurological examinations for more than a century.
The subjective assessment of amplitude by a physician determines the MSR grade, and there is a broad range of possible normal values. Asymmetric results or those that occur in conjunction with other abnormalities are very helpful; isolated hyper- or hyporeflexic MSR in isolation without other findings is usually not regarded as problematic.
Anatomy and Physiology
This causes the first five MSRs mentioned above, but not the jaw jerk. These Ia afferent neurons then send an afferent signal to the spinal cord, where they form a direct synapse with an alpha motor neuron. The muscle contracts as a result of the efferent impulse being transmitted back to it by this activated motor neuron.
An inhibitory interneuron that prevents the opposing (flexor or extensor) muscle group from activating during the reflex is activated when an MSR is initiated. This signal originates from the Ia afferent stretch neuron. As an example, at the knee, the quadriceps oppose the hamstring, thus when the knee jerk reflex is triggered, the quadriceps are stimulated to contract while the hamstring motor neurons are inhibited. In general, the descending corticospinal tract dampens the reflex by modulating the monosynaptic junction between the motor neuron and the muscle spindle stretch afferent neuron.
Since the musculoskeletal, peripheral, and central nerve systems are all included in this reflex arc, a wide range of pathologies can cause changes in reflexes. The spinal segment and peripheral nerve are the bottom motor neuron components of the reflex, and the descending corticospinal tract is the top motor neuron component innervating the reflex arc. Different alterations in the reflex are caused by pathology in either case (see below for clinical importance).
It’s imagined similarly with the jaw jerk. Proprioceptive signals are an afferent signal that travels from the mandibular nerve to the trigeminal nerve‘s mesencephalic nucleus. Rather than the corticospinal tract, the corticobulbar provides the innervation of the modifying upper motor neuron.
Equipment
From specialist to improvised, a range of tools are employed to elicit a response; however, specialized hammers are often preferred. Based on their head design, the most popular specialized reflex hammers can be classified into three types: round (Babinski, Queen Square), T-shaped (Tromner, Buck), or triangular/tomahawk-shaped (Taylor). Both are good for evoking reflexes; however, Taylor may be less successful at evoking reflexes that are more resistant (hyporeflexia).
A clinician’s fingertips, which can be useful for extremely reactive patients, the rim of a smartphone, or the chest piece of a stethoscope are examples of often-used makeshift instruments.
Preparation
First 5 MSR
The ideal position for the patient is one in which the joint may hang at an approximately 90-degree angle and the muscles above and below it can be fully relaxed. In order to test the biceps reflex, for example, the elbow will naturally hang limply at nearly 180 degrees of extension. However, it can be supported to approximately 90 degrees while remaining fully relaxed by placing it on the patient’s thigh if they are seated, or by supporting it in the clinician’s arm. When evaluating any reflex, the heads of the infants should be positioned midline.
Jaw Jerk
It is ideal for the patient to be positioned with their jaw hanging loosely and open. The mouth ought to be somewhat open as a result.
Technique
This group presents all the deep tendon reflexes that are frequently employed. Reflex examinations are typically more convenient to incorporate into a screening test when done in conjunction with other examinations of that body area. However, when a suspected or confirmed anomaly in the reflexes is found, the reflexes should be inspected collectively, with close attention to the testing technique.
It is ideal to get valid test findings while the patient is uneasy and not paying attention to what you are doing. Following a basic explanation, mix in questions or remarks that are meant to elicit a lengthy speech from the patient about other subjects, along with precise instructions. Try the following if you are unable to elicit any reaction from a particular reflex (ankle jerks are typically the most challenging):
- many postures of the limb.
- Ask the patient to slightly tense the muscle that is being examined. To do this, the patient can contract a muscle that isn’t being tested vigorously.
- When testing the opposing extremity, have the patient create a fist with one hand in the upper extremity.
- The patient has linked the fingers of both hands together so that the arms can pull firmly on each other. Just before you are about to tap the tendon, give the command “pull.”
- Generally speaking, the more you can divert the patient’s attention from your task, the more likely it is that you will get the reflex. Examples include asking the patient to count or name the children.
- Sitting on the side of the bed or examination table is the ideal position for the patient. Excellent is the Babinski reflex hammer. Apply a quick, yet gentle, tap. For the action, use your wrist rather than your arm. When testing an extremity, it can be helpful to quickly shift the limb and conduct the test while eliciting the reaction from several positions. Vary the force and record any difference in the reaction.
Take note of the reflex response’s following characteristics:
- Hammer force required to produce a contraction
- Rate of contraction
- Contractional strength
- length of the contraction
How long does the relaxing phase last?
Other muscles not examined and their response. Tapping the brachioradialis tendon can cause reflex activity, such as a hyperactive biceps or finger reflex. It’s known as “overflowing” a reflex.
Always proceed straight to the opposite side for the same reflex after achieving it on one side so that you may compare them.
Jaw Jerk
Put the point of your index finger on your slightly open, relaxed jaw.
Biceps Reflex
The arm is in the middle of its range of motion. With your fingers curled over the elbow and your thumb firmly over the biceps tendon, give it a quick tap. The elbow will bend in the forearm.
Triceps Reflex
Place the patient’s forearm on the thigh or cradle it on your own, keeping the arm halfway between flexion and extension. There is a forearm extension.
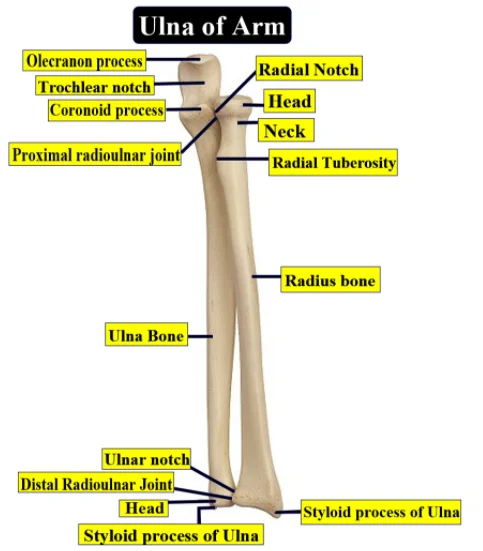
Brachioradialis Reflex
Supporting the patient’s arm is necessary. At the wrist, locate the brachioradialis tendon. It inserts at the base of the radius’s styloid process, often one centimeter to the lateral side of the radial artery. When in doubt, instruct the patient to hold the arm as though it were in a sling, flexed at the elbow, and halfway between supination and pronation. Then, defy your resistance by flexing the patient’s forearm at the elbow. At that point, the brachioradialis and its tendon will be prominent.
- Flexion of the forearm is the biceps reflex. When the brachioradialis tendon is tapped to activate the biceps reflex, you will feel the tendon contract.
- The brachioradialis reflex is the sole one that is typically aroused. However, these reflexes may also be activated in the event of an overactive biceps or finger jerk.
Finger Jerk
Ask the patient to lightly curl his fingers over your index finger in the same manner that a bird clings to a tree branch. Then elevate your hand such that the curled fingers are supporting the hand of the patient. Quickly tap your fingers to transfer the force to the patient’s coiled digits. The patient flexes their fingers in response.
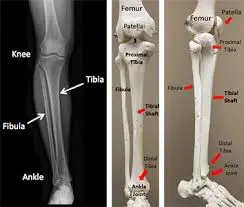
Knee Jerk
Lean the knees out to the side of the bed and feel the contraction of your quadriceps with one hand. When the patient is in bed, flex their knee slightly by putting their forearm beneath both of their knees and contracting their quadriceps while extending their lower leg. Adduction of the ipsilateral thigh can occasionally occur along with a hyperactive reflex.
If the opposing thigh’s adduction and lower leg’s extension are hyperactive, they can potentially happen at the same time. Keep in mind that this so-called leg extension or crossed thigh adduction indicates that the reflexes in the opposing leg are overactive. Regarding the condition of the reflex in the leg being examined, they don’t tell you anything. If there’s no answer, use the Jendrassik technique.
Ankle Jerk
Place one hand beneath the foot’s sole while the patient is seated, then softly dorsiflex the foot. When caring for a patient who is in bed, bend the knee, slightly invert or evert the foot, and hold the foot and lower leg in your arm. Next, give the tendon a tap.
In the event that the patient does not react, have them face a chair and kneel with their feet protruding over the seat, their knees pressed on the chair’s back, and their elbows resting on top of their back. If that isn’t successful, try the Jendrassik maneuver. When monitoring patients who may have thyroid problems, this position is ideal for observing the relaxation phase of the reflex.
Basic Science
The spindle is innervated by the afferent neuron, which has its cell body located in a sensory ganglion. This neuron fires in response to a stretch in the muscle spindle, which monosynaptically excites alpha motoneurons in the spinal cord’s anterior horn. The second neuron, an alpha motoneuron, provides the muscle being tapped or momentarily stretched.
The intricate mechanics that underlie the spindle’s functioning are highly intricate, but a great deal of information about them is now available in the literature, and more information is being contributed on a regular basis. The typical muscle fibers are mixed together with the thin, spindle-shaped structure known as the muscular spindle. Nuclear bag fibers and nuclear chain fibers are the two types of elongated, poorly staining fibers that make up each spindle. Everyone has more than one nucleus. Since they are located inside the fusiform structure as opposed to the surrounding “extrafusal” fibers that comprise the contractile part of the muscle, they are referred to as “intrafusal” muscle fibers.
Primary and secondary afferent sensory terminals are the two types that innervate the spindle fibers. The spindles ignite based on the speed and degree of elongation applied to the core nuclear areas of the intrafusal fibers.
The dorsal horn receives impulses from the spindle receptors and routes the information in four ways:
- (1) to the cortex
- (2) to synapse directly on an alpha motoneuron, causing the muscle innervated by the spindle, the agonist, to contract immediately
- (3) to synapse on an inhibitory neuron, which in turn synapses on an alpha motoneuron that goes to a muscle antagonistic to the one innervated by the spindle, therefore, there is concurrent relaxation of the antagonist as the agonist contracts
- (4) to the cerebellum via the dorsal spinocerebellar tracts.
The path followed by the afferent impulses from the muscle spindles’ sensory nuclei is described in the preceding paragraph. Now remember that the intrafusal fibers, a contractile element, make up the second component of the spindle. Gamma motoneurons, tiny neurons found in the anterior horn that are impacted by the cerebellum, cortex, and other brainstem nuclei, regulate the contraction of the ends of intrafusal fibers and consequently the strength of the central parts. The ability for these supraspinal regions to “set” and, eventually, control the sensitivity of the spindle is most likely the purpose of this motor innervation of a sensory component.
This interneuron then synapses on an alpha motoneuron, which sends the impulse to the agonist. As a result, the tendon organ eventually results in the agonist’s relaxation and, through interneurons, the antagonist’s facilitation.
In order to maintain muscle tone and, eventually, limb posture, the spinal reflexes that are set up by the previously mentioned systems work to keep the muscle fibers tuned to a given length and tension.
Clinical Significance
A lesion in the reflex arc itself is indicated by absent stretch reflexes. Localization is typically made possible by concomitant symptoms and signs:
- Lesion involving the afferent arc of the reflex, either nerve or dorsal horn, resulting in absent reflexes and sensory loss in the distribution of the neuron feeding the reflex.
- The efferent arc is affected by either the efferent nerve the anterior horn cells, or both, resulting in an absent reflex accompanied by paralysis, muscle atrophy, and fasciculations.
- The most frequent cause of missing reflexes nowadays is peripheral neuropathy. A number of conditions and poisons, such as lead, arsenic, isoniazid, vincristine, and diphenylhydantoin, as well as vitamin deficiencies and diseases like pellagra, beriberi, and pernicious anemia, are among the causes. Any or all parts of the reflex arc may be affected by neuropathies, which might be primarily sensory, motor, or mixed (see Adams and Asbury, 1970, for an excellent overview). Stretch reflex disorders do not cause a disruption in this response unless the affected muscle is deemed incapable of contracting. This can occasionally happen in conditions like muscular dystrophy and polymyositis.
- When there is an “upper motor neuron lesion,” or disruption of the cerebral supply to the lower motor neuron, hyperactive stretch reflexes are observed. Localizing the lesion is made possible through analysis of related findings.
- The degree of lesions along the neuraxis can be excellently inferred from the stretch reflexes. In the event that the brachioradialis and biceps reflexes are normal, the triceps reflex is absent, and the lower reflexes (ankle, knee, and finger jerks) are hyperactive, the lesion.
- Reflex laterality is also beneficial. For instance, if every reflex on the left side of the body is hyperactive while the reflexes on the right side are normal, this indicates that a lesion is occurring somewhere above the level of the most hyperactive reflex on the left side of the body, disrupting the corticospinal pathways to that side.
- A useful brochure to have in your backpack for testing and assessing muscles regarding their innervation is Aids to the Investigation of Peripheral Nerve Injuries.
FAQs
Where is the DTR assessed?
Categorizing Deep Tendon Responses
Just behind the elbow is the triceps reflex.
On the radial aspect of the forearm, approximately 2 to 4 inches above the wrist, is the brachioradialis reflex.
Just below the patella is the quadriceps (patellar) reflex.
Just behind the ankle is the Achilles (ankle) reflex.
In neurology, what is DTR?
Reflexes are motor reactions to sensory stimuli that are used to evaluate the health of the motor system in patients who are conscious or unconscious. Deep tendon reflexes (DTRs) are the reflexes that are most frequently evaluated. The muscle contraction of the stimulated tendon should be elicited by a DTR.
How much is a typical DTR score?
On a scale of zero to four, deep tendon reflexes are rated. A response of zero denotes no response, whereas a response of four denotes a rapid, agitated response. Two is regarded as the normal score.
What makes someone lack reflexes?
Reflex-related neuropathy can be caused by some bacterial or viral illnesses. Neuropathy has been associated with Epstein-Barr virus, shingles, hepatitis B and C, HIV, and Lyme disease. Pharmaceuticals. Nerve injury is one of the negative side effects that may occur from prescription medications for serious conditions.
How do deep and superficial reflexes differ from one another?
Rather than muscle, skin-based sensory afferents trigger the superficial reflexes. Lower motor neuron (LMN) pathways, which are usually monosynaptic, mediate muscular stretch reflexes, or deep reflexes. An upper motor neuron (UMN) injury causes these reflexes to increase, whereas an LMN lesion causes them to diminish.
Which kinds of deep reflexes are there?
Always proceed straight to the opposite side for the same reflex after achieving it on one side so that you may compare them.
Jaw-dropping. With your jaw relaxed and roughly one-third open, place the tip of your index finger on it. …
Brachioradialis Reflex,
Biceps Reflex,
Triceps Reflex,
Ankle Jerk,
Knee Jerk,
Finger Jerk.
What is physical therapy for reflexes?
An unconscious, almost immediate movement in reaction to stimuli is called a reflex. Reflexes are instinctive reactions to stimuli that happen automatically and don’t require conscious thought since they happen along a reflex arc. Reflex arcs react to an impulse before it reaches the brain.
What is a typical knee-jerk reflex?
The patellar reflex is a stretch reflex that checks the L2, L3, and L4 segments of the spinal cord. The patellar reflex has been observed in a wide variety of animals, including dogs, cats, horses, and other mammalian species—most notably, humans.
Why does one not have a knee-jerk reflex?
PNS disease affecting either the efferent motor neurons or the afferent sensory neurons may be the cause of an absent or reduced patellar tendon reflex. The lesion is probably in the afferent sensory nerves if there is sensory loss along with a reduced or absent response.
DTR Medical: What is it?
DTR Medical operates under two unique business names: we produce single-use surgical tools under our own DTR Medical brand, and we also offer cleanroom contract manufacturing services to a variety of pharmaceutical and medical device manufacturers.
References
- Walker, H. K. (1990). Deep Tendon Reflexes. Clinical Methods – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK396/
- Zimmerman, B., & Hubbard, J. B. (2023, July 24). Deep Tendon Reflexes. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK531502/