Trigger Point in Quadriceps
What is a Trigger Point in the Quadriceps?
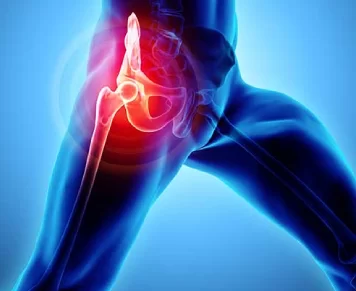
A trigger point in Quadriceps Located in the front of the thigh, the quadriceps are a set of four muscles that are essential for a variety of lower body activities, including running, jumping, and squatting. These muscles enable the bending of the hip and the extension or straightening of the knee. Trigger points are localized muscular tension and soreness areas that can cause pain and discomfort.
These muscles are prone to generating trigger points. Tight bands of tissue that impede blood flow and provide areas of enhanced sensitivity can occur when muscle fibers are inflamed or injured. Numerous symptoms, such as soreness, stiffness, weakness, and restricted range of motion in the afflicted muscle, may result from this.
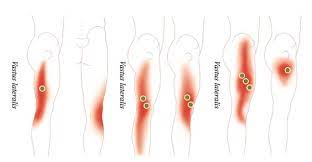
Depending on whatever particular muscle in the group is impacted, quadriceps trigger points might appear in various places. The rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius are muscles that make up the quadriceps. These muscles can all create trigger points, either on their own or in concert with one another.
It’s critical for athletes, fitness enthusiasts, medical professionals, and everyone else experiencing lower body pain or dysfunction to understand quadriceps trigger points. People can manage and reduce discomfort, enhance muscular function, and avoid further problems by being aware of quadriceps trigger points’ telltale signs and symptoms.
The quadriceps muscles’ architecture, trigger point causes and symptoms, common quadriceps trigger point sites, and efficient pain relief and muscular function restoration techniques will all be covered in this handbook. Furthermore, we will discuss ways to promote general musculoskeletal health and lower the likelihood of developing quadriceps trigger points.
Knowing your quadriceps’ trigger points can help you take charge of your physical health and improve your quality of life, whether you’re an athlete looking to reach peak performance, someone recuperating from a quadriceps injury, or just someone looking for relief from pain and stress in your muscles. Let’s explore this crucial subject and learn how to control quadriceps trigger points for an increased range of motion.
Quad Trigger Point Examples
Larger pains in the thigh, hips, and knees are frequently caused by quad trigger points. Tight quadriceps are very frequently the cause of back pain. Deep knee discomfort is frequently the result of a trigger point in the rectus femoris. The trigger point is actually in the hip region, although the symptoms are in the knee. You can really focus on this trigger point with a single-leg stretch, which is an excellent stretch for runners.
Tightness in the IT (illotibial) band is another condition closely linked to quad pain. This thick ring of tissue covers the outside portion of the thigh and extends from the hip to the knee. Knee soreness is frequently accompanied by IT Band Syndrome pain. A trigger point in the vastus lateralis of the IT band is frequently linked to aches there.
Few stretches can successfully work on this trigger point. See a physical therapist who can release the knots in your vastus lateralis and inquire about foam-rolling methods if interested.
Connected Symptoms
Finding the source of the issue and choosing the most effective treatment plans depend greatly on your ability to identify the symptoms connected to quad trigger points. Localized pain or discomfort is usually experienced when a quadriceps trigger point manifests. Muscle rigidity or a palpable “knot,” also known as a quad muscle knot, may accompany this.
It’s crucial to remember that each person may experience symptoms that differ significantly in intensity. While some people may only feel slight discomfort, others may describe excruciating pain. These “knots” in the quadriceps can also cause twitching, weakness, and restricted knee flexion range of motion. Trigger points in the quadriceps may occasionally result in referred pain that spreads to other locations. This is particularly true in the case of patellar tendon issues and anterior knee pain.
Reasons
Trigger points in the quadriceps are frequently caused by strain, trauma, or overuse. Tension in the quadriceps and deconditioning can also result from a sedentary lifestyle.
The Rectus Femoris trigger point
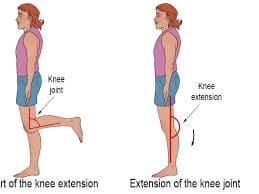
A sizable muscle in the front of the thigh, the Rectus Femoris is a member of the quadriceps muscular group. It runs downward to link to the patella (the knee cap) and tibia (the lower leg bone) after attaching to the pelvis above the hip joint.
When it tightens, the hip joint flexes, raising the knee, and the knee joint extends, straightening the leg.
This muscle’s trigger points can cause a weakening in the knee that is felt when descending stairs, as well as pain that is right over the knee joint.
Symptoms of the Rectus Femoris Trigger Point: Patients will complain of sharp, deep pain at the front of the knee and slightly above it in the lower thigh area if they have active trigger points in this quadriceps muscle. Depending on how they sleep, the pain can cause them to wake up during the night.
Additionally, a disease known as “buckling hip” may occur in some patients. If they aren’t holding on to the handrail, this usually happens when they are going downstairs and could result in a quick fall. The patient would frequently walk on their tiptoe with the bothersome leg in an attempt to make up for the buckling hip issue.
The vastus medialis trigger points
Located on the inner and front of the thigh, the Vastus Medialis is a muscle belonging to the quadricep muscular group. It connects to the femur, the largest thigh bone, and continues down the thigh to the patella, the knee cap, and the tibia, the largest lower leg bone.
The Vastus Medialis contracts to extend the leg at the knee joint and support the knee during walking and running, just like the other quadricep muscles.
This muscle’s trigger points cause severe discomfort in the inside of the lower leg above the knee as well as the knee joint itself.
Symptoms of the Vastus Medialis Trigger Point: Patients commonly describe their knee pain as having a toothache-like sensation when they have active trigger points in this muscle. Whenever they attempt to fall asleep, their pain will frequently get worse. A disease known as “buckling knee” may also affect these people, in which their knee gives out unexpectedly and they fall while walking.
The trigger points in the vastus lateralis
The largest muscle in the quadriceps muscle group is the vastus lateralis. It starts on the lateral aspect of the patella bone and attaches to the posterior-lateral aspect of the femur bone after traveling down the outside of the thigh. Lower leg extension at the knee is the result of this muscle contracting.
Pain is referred to the outside of the thigh by trigger points in the upper portion of this big muscle and to the knee by trigger points in the lower region.
Symptoms of the Vastus Lateralis Trigger Point: Individuals who have pain around the outside of their thighs and knees are said to have activated trigger points in their vastus lateralis muscle. When they walk, the pain usually becomes worse, and when they sleep, it gets better.
When they try to bend or straighten their leg, they could also complain of a stuck knee bone that doesn’t move up and down properly. If the leg is bowed slightly, it could lock. They frequently have to drag their foot and walk with their pained leg stiff.
The Trigger Points in the Biceps Femoris
The Semitendinosus, Semimembranosus, and Biceps Femoris are the three muscles that make up the Hamstring muscle group.
The fibula, a smaller lower leg bone located immediately below the outside edge of the knee joint, is where the Biceps Femoris joins after extending downward from the pelvic bone to the thigh bone, or femur. Leg bending occurs when the Biceps Femoris muscle contracts, flexing the knee. It is extensively utilized for jogging, walking, and other exercises. This muscle has trigger points that cause discomfort in the back of the leg, buttock, and back of the knee. They might also result in cramps similar to “Charlie Horse” episodes. Walking and sitting both cause pain, and it may keep you from sleeping The other thigh muscles will often become overworked and generate their own unique trigger points as a result of the muscle weakness caused by these trigger points.
Symptoms of the Biceps Femoris Trigger Point: Individuals who have active trigger points in their biceps femoris will typically complain of pain in their posterior leg or knee, which gets worse when they walk and frequently results in a limp. When they sit, the discomfort may be more intense in the buttocks and may keep them up at night.
Patients may also have knee and front-of-thigh pain, which are symptoms associated with trigger points in the quadriceps femoris. Because of their close biomechanical interaction, the hamstring and quadriceps muscle groups frequently experience trigger point activity together.
Assessment of the trigger point
The physical finding most frequently linked to a trigger point is the palpation of a hypersensitive bundle or nodule of muscle fiber with a tougher-than-normal consistency. A doctor’s sense of feel, patient complaints of discomfort, and tactile and visual studies of the local twitch response are all used to help localize a trigger point.
Along with a twitch reaction, this palpation will generate discomfort over the palpated muscle or radiate pain toward the reference zone. Trigger points, as are their pain reference zones, are repeatedly found in constant positions.
Treatment for trigger point in quadriceps
Physiotherapy, stretching, and massage are frequently advised as ways to help the quad muscles relax. By concentrating on particular quadricep trigger points, myofascial release techniques or trigger point therapy can be utilized to release the quadriceps.
If symptoms continue even after attempting these therapies, it is advisable to exclude other possible causes as the trigger points themselves might not be the main cause of the problem.
Postural correction: Recurrence can be avoided by treating underlying postural abnormalities or movement patterns that support the formation of trigger points.
Controlling the trigger points
It is crucial to eliminate conditions that predispose and perpetuate chronic overuse or stress injuries to muscles. Patients with persistent musculoskeletal pain can be treated pharmacologically with analgesics and drugs that relax and produce sleep. These individuals are frequently prescribed antidepressants, neuroleptics, or nonsteroidal anti-inflammatory medications.
Acupuncture, osteopathic manual medicine approaches, massage, acupressure, ultrasonography, applying heat or cold, diathermy, and transcutaneous electrical nerve stimulation are examples of nonpharmacologic therapeutic modalities that can be used to relieve tense muscles and accelerate healing. trigger-point injections with a local anesthetic, saline, or corticosteroid; dry needling; and the ethyl chloride Spray and Stretch treatment.
Using the Spray and Stretch approach, the goal muscle is passively stretched while ethyl chloride or dichlorodifluoromethane-trichloromonofluoromethane (Fluori-Methane) spray is applied topically. It is believed that the abrupt drop in skin temperature blocks the spinal stretch reflex and the higher center of pain perception, temporarily producing anesthesia. By allowing the muscle to passively stretch toward its normal length, the pain perception is lessened, allowing one to release trigger points, relax muscular spasms, and lessen referred pain.
Because it depletes the ozone layer, dichlorodifluoromethane-trichloro mono-fluoromethane, a benign and nonflammable vapor cooling spray, is no longer commercially accessible for use in other applications. Nonetheless, compared to the original volatile vapor coolant, ethyl chloride, its use is safer for the patient and the doctor. A general anesthetic with a quick onset of action, ethyl chloride turns combustible and explosive when 4–15% of its vapor is inhaled. Despite this, ethyl chloride is still a widely used agent due to its ability to function as a local anesthetic and have a higher cooling impact than dichloride fluoromethane-trichloro mono fluoromethane.
The type of trigger point and the physician’s skills and experience both play a major role in the decision to treat it manually or with an injection. Physical therapy can be an effective treatment for trigger points that are in the acute stage of creation (before more pathologic alterations emerge). Additionally, manual techniques are recommended for individuals with severe needle phobias or when the trigger point is located in the middle of a belly muscle that is difficult to reach with an injection (such as the psoas and iliacus muscles). Teaching the patient how to properly self-manage their pain and dysfunction is the aim of manual therapy. When contrasted with injection techniques, manual procedures are more likely to need multiple treatments, and the results might not become completely evident for a day or two.
Trigger-point injection and dry needling of trigger points have gained widespread acceptance, despite the relatively small amount of research on the subject. This therapeutic technique is frequently mentioned as the most effective strategy to attain the best results and is one of the most successful treatment alternatives accessible.
Patients with symptomatic active trigger points that twitch in response to pressure and cause a pattern of referred pain are candidates for trigger-point injection. It was discovered that dry needling was just as successful as injecting an anesthetic solution like lidocaine (Xylocaine) or procaine (Novocaine).On the other hand, compared to patients who had a lidocaine injection, dry-needling patients experienced more severe and prolonged post-injection discomfort.
the use of dry needling versus lidocaine injection for trigger point treatment, 58% of patients experienced total pain alleviation immediately following the injection, while 42% of patients said their pain was only moderate (1-2/10 on the pain scale). To relieve myofascial pain, both dry needling and injections containing 0.5 percent lidocaine were equally effective. Myofascial discomfort is not the same as postinjection soreness, which frequently occurs, particularly following the application of the dry needling technique. These findings confirm the views of the majority of researchers, who believe that the mechanical disturbance caused by the needle is the key therapeutic element in both injection and dry needling.
The Trigger-Point Injection Method
Injecting trigger sites can be an efficient way to deactivate them and deliver fast symptom relief. This table lists the tools required for trigger-point injection.
Tools Required for Trigger-Point Injection
- Gloves made of rubber
- pads of gauze
- Alcohol-based skin cleansing pads
- 3- or 5-milliliter syringe
- Procaine (Novocain, 1 percent) or lidocaine (Xylocaine, 1 percent, without epinephrine)
- Depending on the injection site, different lengths of 22-, 25-, or 27-gauge needles may be used.
- Sticky bandage
- severe needle phobia
Issues with Trigger-Point Injections
- Syncope caused by vasovagal
- skin infection
- Pneumothorax: Never point a needle at an intercostal area to prevent complications from pneumothorax.
- Avoid needle damage by never putting the needle into the hub.
- Avoid hematoma formation by providing direct pressure for a minimum of twenty minutes following injection.
Before injection precautions
Before injection, greater bleeding tendencies should be investigated. Capillary bleeding causes ugly ecchymosis and worsens postinjection pain. To prevent more bleeding, patients should stop taking aspirin daily at least three days before injection. To induce muscle relaxation, the patient should be positioned in a comfortable or recumbent position. The simplest way to accomplish this is to put the patient in a supine or prone position. If the patient experiences a vasovagal reaction, this positioning may also assist them prevent damage.
Choose Your Needles
The location of the muscle being injected determines the needle size to use. To break up the contraction knots in the trigger point, the needle has to be long enough to reach them. Generally, a 1.5-inch, 22-gauge needle can adequately reach the majority of superficial muscles. A 21-gauge, 2.0-inch needle is typically required for thick subcutaneous muscles, such as the gluteus maximus or paraspinal muscles in individuals who are not obese. To reach the deepest muscles, like the gluteus minimus and quadratus lumborum, a hypodermic needle measuring 2.5 inches and gauged at 21 is needed. A smaller diameter needle might be less painful, but it might not provide the doctor with the necessary mechanical disruption of the trigger point or sufficient sensitivity while entering the subcutaneous tissue and surrounding skin. In addition, a very taut muscle band may deflect a thinner gauge needle, preventing the trigger point from being punctured. Since the hub is the weakest point of the needle and may break below the skin, it should always be long enough to avoid having to be entered into it.
Injection Solutions
Typically, 1% lidocaine or 1% procaine is used as an injectable solution. Injectables used for trigger-point therapy have also included diclofenac (Voltaren), botulinum toxin type A (Botox), and corticosteroids. These drugs have, nevertheless, been linked to considerable myotoxicity. Among all the injectable local anesthetics, propeciaine holds the distinction of being the least myotoxic.
Method of Injection
The practitioner separates a trigger point by squeezing between the thumb and index finger or between the index and middle finger, depending on which is most relaxing after the trigger point has been identified and the surrounding skin has been cleaned with alcohol. The needle is then advanced into the trigger point at an acute angle of 30 degrees to the skin by inserting it 1 to 2 cm distant from the trigger point using sterile procedures.
By applying pressure on both sides of the injection site, the stabilizing fingers make sure that the muscle fibers are sufficiently tense to permit the trigger point to pierce while keeping it from rolling away from the approaching needle. Applying pressure also lessens the chance of internal bleeding in the subcutaneous tissues, which could irritate the surrounding muscle. You can prevent pneumothorax, a potentially fatal condition, by not pointing the needle at an intercostal gap.
The doctor should alert the patient about the likelihood of acute pain, twitching of the muscles, or an unpleasant sensation as the needle makes contact with the taut muscular band before inserting the needle into the trigger point. To guarantee that the needle is not inside a blood vessel, the plunger should be removed before administration. As soon as the needle enters the trigger site, 0.2 mL of anesthesia should be delivered. After withdrawing the needle to the level of the subcutaneous tissue, it is redirected superiorly, inferiorly, laterally, and medially. This procedure is repeated in each direction until the local twitch response stops being elicited or the sensation of resisting muscle tautness disappears.
Management following injection
To make sure there are no more painful spots, the area should be palpated after the injection. Any palpably felt painful spots should be identified, needled, and injected. To encourage hemostasis, pressure is then administered to the injection site for two minutes.10 For skin coverage, a basic adhesive bandage usually works well. Trigger point therapy works even better when the affected muscle area is stretched right after injection. The ideal way to accomplish this is to have the patient actively move each injected muscle through its whole range of motion three times, each time reaching its fully extended and fully shortened positions.
Most of the time, postinjection soreness is to be expected, and the injection was successful based on the patient’s reported improvement of the referred pain pattern. Reinjecting trigger points is not advised until the postinjection discomfort subsides, which typically happens three to four days following the injection. However, re-evaluation of the injected sites may be required. If two or three previous efforts at an injection in a particular muscle have failed, it is not advised to try that muscle again. In the week following trigger-point injections, patients are encouraged to stay active and use their muscles to the fullest extent possible. However, they are advised to refrain from intense exercise, particularly in the first three to four days following injection.
Trigger point therapy for pain in the knees and thighs
One of the most common pain conditions that people fear is knee discomfort. Sports-related knee injuries are common and are associated with the possibility of needing knee surgery. The “balance” of muscle effort while walking, running, and other exercises is crucial to the knee joint’s appropriate functioning. This “balance” can be upset, and the typical mechanics of the knee joint itself can be changed, by active trigger points in the thigh muscles.
These trigger points usually transmit pain to the knee joint; therefore, it is important to recognize this discomfort as an indication that the thigh muscles have been overworked and require time to heal.In addition to causing discomfort, these trigger sites frequently result in abrupt knee bowing or weakening. Trigger Point Therapy works well for a variety of knee pain conditions, including hard-to-heal post-surgical situations. Trigger point therapy is a neuromuscular treatment intended to reduce pain, treat muscle imbalances, and expedite the healing process following an accident. After stretching the muscle, your physiotherapist will apply pressure to any “knots” or areas of tension in the muscle. This facilitates healing and relieves tense muscles.
Quadriceps trigger point stretching exercises
While standing, flex your quadriceps.
How to do it: Use one hand to balance on a wall or cling to the back of a chair.
Raise a foot behind your body and place your hand over your ankle.
Maintain a straight back and closely spaced knees.
With caution not to overstretch it, bring the heel in toward the buttocks.
After holding the leg for up to 30 seconds, gently release it.
Continue after switching sides.
The quadriceps are the main muscles addressed: the front of the thigh should feel stretched when standing.
Advice: Avoid bending or twisting your back.
Be aware that this posture may place too much strain on the ligaments and knee joint. Avoid doing this stretch until you’ve spoken with a medical professional who is appropriately qualified if you have knee pain or damage.
injury for which stretching could be beneficial: straining the hip flexors. fracture avulsion in the pelvis. pubic osteitis. tendinitis in the iliopsoas. bursitis in the trochanter. strain on the quadriceps. tendinitis in the quadriceps. syndrome of patellofemoral pain. tendinitis of the patella. kneecap subluxation.
pelvic tilt anterior

As you take a modest step forward, stand up straight. Lean back and then away from your back leg while reaching up with both hands and pushing your hips forward.
You can adjust the stretch’s intensity by pressing your hips forward.
stretching the muscles: Rectus femoris is the main muscle. Psoas primary. Iliac. Sartorius.
The Rectus abdominis is a secondary muscle. abdominis transversus. Obliques both internal and external. Lumborum quadratus.
injury for which stretching could be beneficial: straining the hip flexors. fracture avulsion in the pelvis. pubic osteitis. tendinitis in the iliopsoas. bursitis in the trochanter. strain on the quadriceps. tendinitis in the quadriceps.
Half-lying to stretch the quads
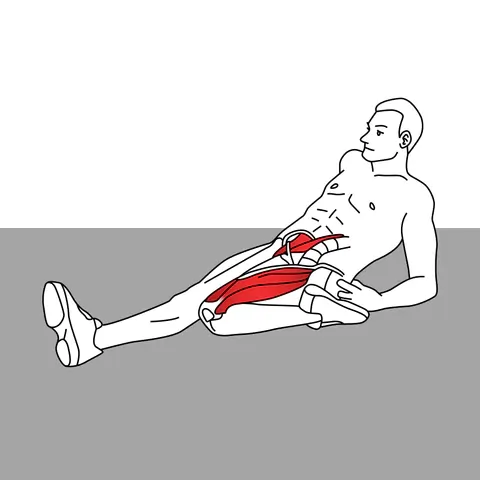
Position your foot next to your buttocks while bending one knee and sitting on the ground. Then tilt backward gradually.
Be aware that this posture may place too much strain on the ligaments and knee joint. Avoid doing this stretch until you’ve spoken with a medical professional who is appropriately qualified if you have knee pain or damage.
stretching the muscles: The Rectus femoris is the main muscle. Vastus intermedius, lateralis, and medialis.Psoas major and iliacus a secondary muscle
injuries for which a stretch could be helpful: straining the hip flexors. fracture avulsion in the pelvis. pubic osteitis. tendinitis in the iliopsoas. bursitis in the trochanter. strain on the quadriceps. tendinitis in the quadriceps. syndrome of patellofemoral pain. tendinitis of the patella. kneecap subluxation.
Stretch your quadriceps in a supine
Bend one or both knees while sitting on the ground, tucking your legs beneath your buttocks. Then tilt backward gradually.
Be aware that this posture may place too much strain on the ligaments and knee joint. Avoid doing this stretch until you’ve spoken with a medical professional who is appropriately qualified if you have knee pain or damage.
stretching the muscles: Rectus femoris is the main muscle. Vastus intermedius, lateralis, and medialis.Psoas major and iliacus a secondary muscle
injuries for which stretching could be beneficial: straining the hip flexors. fracture avulsion in the pelvis. pubic osteitis. tendinitis in the iliopsoas. bursitis in the trochanter. strain on the quadriceps. tendinitis in the quadriceps. syndrome of patellofemoral pain. tendinitis of the patella. kneecap subluxation.
Stretch your anterior hip flexors.
Start by getting down on your knees.
Bring your right leg forward so that your foot is flat on the ground, your knee bent 90 degrees, and your right thigh parallel to the floor.
Make sure your shin is pointed straight back (not left or right) and keep your left knee on the floor.
Place your hands on your hips, tuck your pelvis under you, clench your glutes, and bring your thumbs down.
Move your weight forward while maintaining a straight back until you feel a stretch in the front of your left leg and groin.
Stretch your left arm up overhead and slightly to the right for a deeper stretch.
Continue on the opposite side.
Stretching the muscles
Primary: Iliacus muscle. Major and minor Psoas.
The rectus femoris is a secondary muscle. Sartorius.
injury for which a stretch could be helpful: straining the hip flexors. fracture avulsion in the pelvis. pubic osteitis. tendinitis in the iliopsoas. bursitis in the trochanter. strain on the quadriceps. tendinitis in the quadriceps.
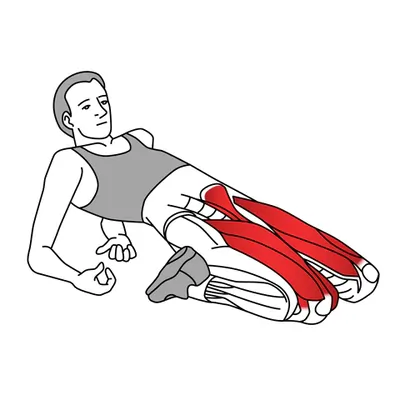
Hip flexor side-lying stretch

With your legs bent to parallel your hips, take a left-side position on the floor. A 90-degree angle should be formed by your shins and thighs.
Reposition your right foot so that your right hand is softly gripping the top of your ankle.
With your right hand, carefully and gradually drag your foot to bring your leg around behind you. Keep your pelvis tucked down and watch out not to arch your back. Your right hip flexor and the front of your thighs should both feel stretched. On the other side, repeat.
How to take care of yourself
When used correctly, self-treatment techniques for quad trigger points can successfully reduce discomfort and improve muscular function.
To begin treating these muscular “knots” on your own, you must first determine which trigger points are involved. Once they’ve been located, you can release them using a variety of methods.
These methods can involve muscle energy techniques, ice treatment with stretching, or self-myofascial release using an instrument like a foam roller, tennis ball, lacrosse ball, etc.
By extending the quadriceps muscles, you can help to ease tense muscles and increase blood flow. For best results, it is imperative to keep the stretch mild and steady.
Heat therapy: Using heat to the affected area might aid in pain relief and muscle relaxation.
Ice therapy: Applying ice to the affected area might help lessen discomfort and inflammation.
How to use muscle energy for the quads
MET is a form of manual therapy that enhances joint mobility and muscle function by utilizing the patient’s muscle energy, or power. This is how it operates:
When performing isometric muscle contractions: the therapist extends the quadriceps. Next, the therapist gives the patient a counterforce to work against while they contract the quad. This is carried out carefully and under control. In general, only 15% of one’s effort is needed.
Stretching and Relaxation: Following an isometric contraction, the muscle is given a brief opportunity to relax. The muscles will then be effectively stretched even further by the therapist as they move the tissues to their new range of motion.
Repeated motions: Until no additional range of motion is obtained, this process is repeated five or more times.
Other things to consider regarding quadriceps trigger points are as follows:
Although they are a widespread issue, trigger points are not always simple to identify.
Trigger points cannot be treated in a way that works for everyone. The degree of your symptoms and the underlying reason behind your trigger points will determine the most appropriate course of action for you.
Trigger points can be treated effectively, allowing you to resume your regular activities.
Advice for Joyful Muscles:
Press the painful spot to find the location of the muscle knot. A knot in your muscle may be actively painful, or you may not even be aware of it until you apply pressure to it.
Determine the ideal pressure. It might make you laugh and cry at the same time when you apply the perfect amount of pressure” to a muscle knot because it hurts so good. But if you press too hard, it can make you weep for forgiveness!
Both the muscle and the muscular knot may feel sensitive when you gently massage them. Pressing on the muscle knot might occasionally cause the symptoms of referred pain to recurrance.
Why the best method for releasing trigger points is acupuncture:
The trigger point is mechanically disrupted by the acupuncture needle.
It breaks the muscle’s cycle of energy crisis. Once the muscle reaches its maximum length, it resumes its regular blood flow and metabolism, enabling it to perform at its peak level.
- Not much hurts from acupuncture.
- Since direct pressure to the trigger point is necessary for many release techniques, it is inherently uncomfortable. A trigger point is frequently too sensitive to take much more mechanical stimulation. The extremely sensitive tissues above and surrounding the trigger point can be penetrated by a needle without causing any discomfort. Truly, no other method can match this level of accuracy.
- Acupuncture produces outcomes right away.
- After a single, carefully positioned needle is inserted into a trigger point, there will be a twitch, lessened muscle tension, and an increase in range of motion. For someone who has been coping with pain and dysfunction in that muscle for weeks, months, or even years, such quick feedback is incredibly satisfying.
Instruments to help reduce quad pain
- THE ORIGINAL TM 18″
- THE roadster TM 11″
- TIGER BALL
- THE LONG ONE TM 22″
- THE curve ball
Prevention is key
Overuse, strain, or prolonged muscle contraction can cause trigger points to develop. To obstruct the trigger point from initiating,
- Gradually increase training loads: Avoid overdoing it too soon and make sure you recuperate enough in between sessions. To guarantee that your body can heal itself effectively, have plenty of good sleep.
- Retain your muscle balance and range of motion: This calls for some effort. Take your body through the OPPOSITE range of motion that is required for your sport regularly. Lengthening the agonist and strengthening the antagonist is a sensible generalization. This entails strengthening the rhomboids and other upper back muscles as well as expanding your pectoral range of motion for cyclists who spend hours in the saddle with a forward shoulder posture. Lengthening the hip flexors (quadriceps, psoas) and building the hip extensors (hamstrings, glutes) are usually beneficial for runners.
- Removal of adherences.
- To restore taut, strained muscular tissue, you must engage in regular exercise. Muscles that are flexible and delicate don’t break. With your fingertips, a foam roller, or a lacrosse ball, For eight to twelve seconds, apply direct pressure on a tight muscle band. By squeezing the muscle and moving it through its range of motion, adhesions can be broken up before a trigger point occurs.
Quad Trigger Points: What Are They?
The quadriceps are resilient muscles that withstand a great deal of strain. However, this also implies that extending your quadriceps and treating your quadriceps pain can be difficult.
Trigger points can be found in the quadriceps muscles in a few different places. In essence, quadriceps trigger points are knots in the quad muscles that produce pain and discomfort both there and elsewhere.
Generally, they respond well to solitary or active isolated stretches as well as efficient targeted massage. For efficient alleviation, you must understand how to stretch your quadriceps.
Why Doesn’t Stretching Always Help at the Trigger Point?
A trigger point-containing muscle will be too painful to fully extend. There’s no way you can extend the muscular band sufficiently without experiencing pain and the ensuing inhibitory reflex.
Furthermore, straining a stretch won’t help to relieve the trigger point and will frequently cause harm (muscle tension). Consider a trigger point to be similar to a rubber band knot. The band will snap if it is stretched, but the knot won’t come free. To give that rubber band its full stretch again, you need to first unwind the trigger point
Summary
Myofascial trigger points, which are hyperirritable areas within the quadriceps muscle group, are trigger points in the quadriceps that can produce transferred pain, discomfort, and regional pain. Overuse of muscles, bad posture, injuries, or stress are common reasons. Pain, stiffness, weakness, and restricted range of motion are some of the symptoms. Postural correction, heat or ice therapy, manual therapy, stretching, and strengthening exercises are commonly used in treatment. It is crucial to get professional advice in order to ensure an accurate diagnosis and customized treatment aimed at symptom relief and recurrence prevention.
FAQS
Trigger points: what are they?
Small, taut knots of muscle fibers known as trigger points can form in any muscle, including the quadriceps. They are frequently brought on by injury, strain, or overuse. A trigger point can produce pain when it is pressed, not just in the vicinity of the point but also in other body areas.
What are the advantages of treating trigger points?
When a muscle is injured, inflammation results. Your body senses this and becomes wounded, which makes you defend the muscle to prevent more damage. The pressure used in trigger point therapy “reprograms” the neuromuscular system to lessen discomfort. This encourages the muscles to return to their original state. Recovery is aided when there is a decrease in inflammation and the patient has less pain and tightness.
Do trigger points subside?
Your trigger points will likely just cause you inconvenience and go away on their own if they are infrequent and little. However, if they persist, they could become more numerous (myofascial pain syndrome), exacerbate other illnesses, and cloud your diagnosis.
Which three categories of trigger points exist?
Trigger points come in three varieties: passive, satellite, and active. When touched, active trigger points hurt and can produce pain in other body parts. Although they don’t always hurt when touched, passive trigger sites can hurt in different parts of the body. While less painful than active trigger points, satellite trigger points are similar to them.
What distinguishes trigger points from pressure points?
The term “trigger point massage” speaks to the idea that damage or inflammation in one part of the body can cause discomfort in another. The phrase “pressure point massage” emphasizes that the goal of the therapy is to help the body heal by applying pressure to the appropriate areas.
What occurs when a trigger point is massaged?
By allowing waste products to be flushed out and new blood to enter, massage helps to release trigger points. By increasing the amount of oxygen in the area and causing the muscles to relax, helps you feel less pain.
To how much are trigger points painful?
A dull, agonizing pain, a burning sensation, or numbness can all be examples of transferred pain. Sweating, moist eyes, chills, lightheadedness, and acute exhaustion are further symptoms. Conversely, latent trigger sites are renowned for remaining undetected for years before causing discomfort.
Which drugs are administered via trigger point injection?
Local anesthetics like lidocaine or bupivacaine are used to numb the injection site; the numbness normally goes away in two to six hours.
Steroid triamcinolone (Kenalog) is used to relieve pain and inflammation.
At home, how do you handle trigger points?
Apply an ice pack to the affected area if pain worsens immediately after physical exertion. Try using a heating pad to help relieve muscle stiffness if you wake up with sore muscles or if the aching soreness lasts for a long time. By rubbing the trigger point, you can help the muscle relax and the knot becomes less tight.
Can trigger points be brought on by stress?
Anxiety and stress. Anxious and worried people may be more prone to develop trigger points in their muscles. individuals might be more prone to tense their muscles. Repeated straining of the muscles, such as clenching, exposes them to trigger points.
How much force is appropriate to press a trigger point?
Continue applying pressure for 30 to 90 seconds, or until the tissue begins to soften or release. As the point releases, the customer frequently reports an improvement in their symptoms. The best benefits are obtained with 90-second holds, but even 30 seconds will make a difference.
Is heat beneficial for trigger points?
Fortunately, this subject is a little easier! To begin with, heat is beneficial for muscles. In particular, it is one of the few treatments for delayed onset muscular soreness (DOMS) and aids in the calming of muscle trigger points.
What lack results in trigger points?
insufficiencies lack vitamins. You may experience trigger points if your diet is deficient in vitamin C, folic acid, iron, vitamin D, or vitamin B.
Do trigger points appear on an MRI?
While an MRI or X-ray cannot identify a trigger point, they can show an underlying medical issue. In the neck or head area, trigger point pain might present as a tension headache, tinnitus, joint discomfort, and eye problems.
Which cream works best for knots in muscles?
Menthol
Naturals with icy heat.
Advanced Relief Patch, Icy Hot.
Gel Patch for Salonsip.
Aspercreme Gel for Heat Pain Reduction.
Max Aspercreme.
Zero Degrees BenGay.
Mentholatum Cold Therapy for Sports Pain.
Ultra Tiger Balm.
Which dietary supplements aid in the triggering of points?
Consider taking supplements for iron, folic acid, vitamin B, and vitamin C if your diet isn’t able to provide you with all the vitamins you need. Exercise and enough hydration can help prevent trigger points from developing in the first place or stop them from growing significantly worse.
Which vitamins work well with trigger points?
Myofascial pain alleviation has been linked to many important vitamins and minerals, including biotin, folic acid, potassium, salt, calcium, iron, and zinc, as well as vitamins A, B1, B2, B3,, C, D, E, K, B5, B6, B12.
What nutrition trigger points are required?
In the fight against pain, vitamins B1, B6, and B12, as well as folic acid and vitamin C, are crucial. Critically important minerals include potassium, magnesium, iron, and calcium. These minerals and vitamins are crucial to the physiology of muscular exercise.
References
- S. (n.d.). Pain in Your Quadriceps? How Targeting Quad Trigger Points Can Help. Stretch 22. https://stretch22.com/pain-in-your-quadriceps-how-targeting-quad-trigger-points-can-help/
- PainWhisperer.com | Trigger Point Therapy for Knee Pain. (n.d.). Pw. https://www.painwhisperer.com/trigger-point-knee-thigh-pain
- Winer, J. (2021, September 22). Trigger Point Therapy – 5 Great Stretches for the Quads. Niel Asher Education. https://nielasher.com/en-in/blogs/video-blog/trigger-point-therapy-5-great-stretches-for-the-quads
- Visnic, S. (2023, October 17). Quad Trigger Points | How To Find And Treat. Release Muscle Therapy. https://releasemuscletherapy.com/quad-trigger-points/
- Trigger Point Therapy – Manual Therapy – Physiotherapy – Treatments – Physio.co.uk. (n.d.). https://www.physio.co.uk/treatments/physiotherapy/manual-therapy/trigger-point-therapy.php
- Tail, T. (2024, February 3). Muscle Knots in Quadriceps. Tiger Tail USA. https://tigertailusa.com/muscle-knots-in-quadriceps/
- Alvarez, D. J., & Rockwell, P. G. (2002, February 15). Trigger Points: Diagnosis and Management. AAFP. https://www.aafp.org/pubs/afp/issues/2002/0215/p653.html
- G. (2020, March 19). Trigger Points: Why Stretching Is Not The Answer. Boulder Acusport. https://www.boulderacusport.com/2015/09/trigger-points-athletic-performance/