Scissor Gait
Introduction
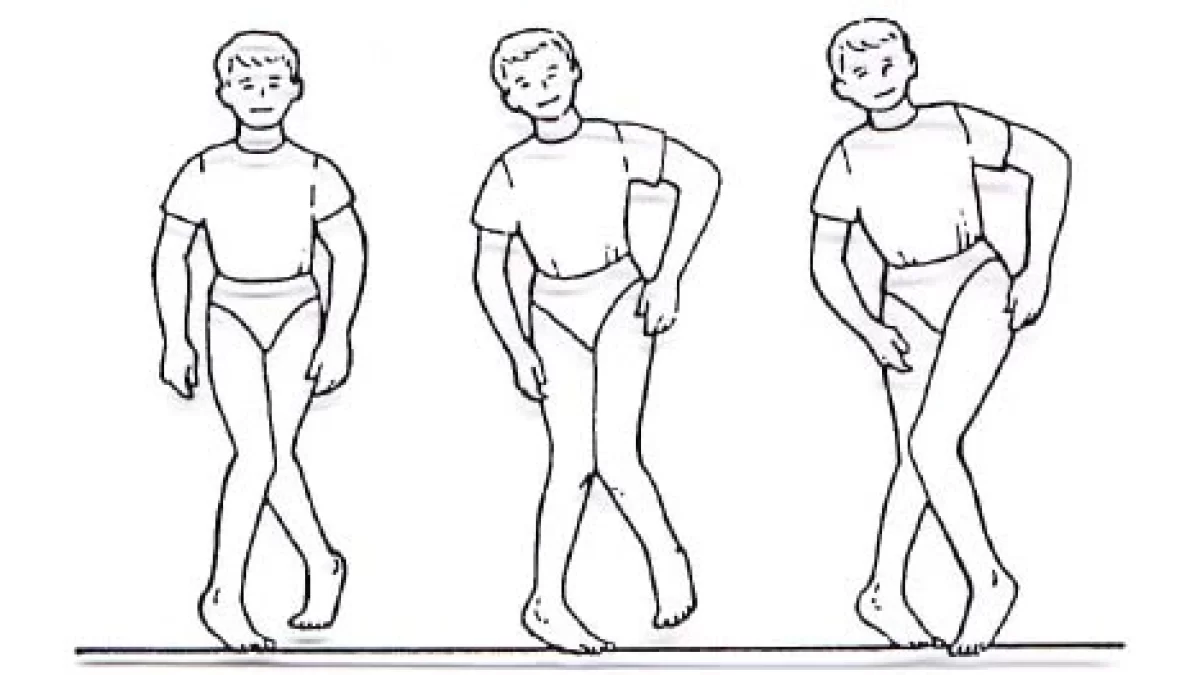
Scissor gait refers to an irregular walking pattern in which the legs cross or overlap while the person walks. A kind of spastic paraparetic walk when the adductor muscles are noticeably toned. In addition to excessive adduction that causes the knees and thighs to strike, or occasionally even cross, in a scissors-like motion, it is characterized by hypertonia and flexion in the legs, hips, and pelvis. Children with cerebral palsy often exhibit a scissor-like stride as they walk. The manner of walking is typical of a marionette walk.
Children with cerebral palsy (CP) frequently experience difficulties learning to walk because the disorder can cause major changes or impairments in gait. One mobility issue that might result from cerebral palsy is the development of the scissor gait. Mobility may become uncomfortable, laborious, and unusually slow when walking this way.
When a child develops spastic cerebral palsy, they often exhibit the scissor gait, which is an unnatural gait. The issue is associated with a gait caused by upper motor neuron damage. Parents may find this walking style comparable to a puppet’s movements or gaits. Furthermore, hypertonia results in varying degrees of flexion of the legs, hips, and pelvis, which makes crouching seem.
Walking irregularly due to tight adductor muscles results in the knees and thighs crossing in a scissor-like motion, while the abductors, the opposing muscles, weaken from inactivity. The child will remain on tiptoes unless the plantar flexor muscles are released through orthopedic surgery.
What is Scissor Gait?
The term “scissor gait” describes the way people who have spastic paraplegia walk. This walking style is similar to that of a marionette. Tight adductors produce extreme adduction, characterized by knees and thighs hitting, or occasionally even crossing, in a scissors-like movement, while the opposing muscles, the abductors, become relatively weak from lack of use. Hypertonia in the legs, hips, and pelvis causes these areas to flex to varying degrees, giving the appearance of crouching.
Patients with spastic cerebral palsy are most likely to have to walk on tiptoe unless an orthopedic surgical surgery releases the plantar flexor muscles.
Regardless of how severe or moderate the spastic CP disease is, these characteristics are most common with the scissors gait and typically lead to some degree of it:
Regardless of how severe or moderate the spastic CP disease is, these characteristics are most common with the scissors gait and typically lead to some degree of it:
- Stiffness and extreme leg adduction during a swing.
- Ankle’s plantar flexion.
- Knee flexion.
- Internal rotation and adduction at the hip.
- Increasing spastic muscular contractures.
- Complex upper limb assistance movements during walking.
Disorders associated with a Scissor Gait
- Arthrogryposis
- Spastic diplegia
- Pernicious anemia
- A cerebrovascular accident
- A disorder affecting the vertebrae in the neck called cervical spondylosis with myelopathy
- Liver Failure
- Multiple sclerosis
- Stroke
- Muscular Dystrophy
- Parkinson’s disease
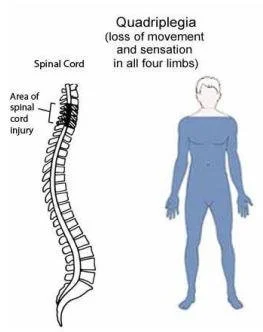
- Trauma to the spinal cord
- Tumor of the spinal cord
- Syphilitic meningomyelitis
- Syringomyelia
- Other kinds of cerebral palsy,
Diagnosis of the Scissor Gait
Medical History
- A medical professional will be paying a close eye on the patient’s walk. Together with any other indications of aberrant gait, they will search for the specific scissor-like action of the legs.
- The patient’s medical history, including any family history of neurological disorders, developmental delays, or trauma, will be questioned by the physician.
Neurological Examination:
- A thorough neurological examination will be carried out to evaluate muscle strength, reflexes, coordination, and sensory function. For this, tests such as the deep tendon reflex and the Babinski reflex may be applied.
Diagnostic Tests:
Other tests might be prescribed based on the suspected underlying cause, such as:
- Imaging study: Structural abnormalities in the brain that may be causing spasticity can be found with the use of MRI or CT scanning.
- Electromyography (EMG): This test measures nerve function by recording the electrical activity of muscles.
- Genetic Testing: In certain situations, underlying genetic problems may be found by genetic testing.
Treatment for the Scissor Gait
For children with cerebral palsy, early intervention is crucial to reducing the development of a scissoring gait. There are two techniques for dealing with a scissoring gait. To allow the muscles to freely contract and relax, spasticity must first be reduced. Second, the child needs to regularly work on enhancing their gait.
Several therapies that can help children with cerebral palsy reduce a scissoring gait will be covered below. Some interventions might be better than others, depending on how severe your child’s spasticity is. To choose the best and most advantageous course of therapy, consult your child’s pediatrician or physical therapist.
Medication
- Muscle relaxants like baclofen can help reduce muscular hyperactivity for the temporary relief of spasticity. Oral muscle relaxants taken multiple times a day usually only provide short-term relief from spasticity.
- Muscle relaxants may make your child feel sleepy, exhausted, or weak. They can also hurt the overall body. This might not be the greatest choice for folks whose legs are just spastic.
- Another option is an intrathecal pump, which is surgically implanted and can also be used to deliver medication for relieving the problem. Because the muscle relaxant in the pump is given directly to the spinal cord, the risk of side effects is reduced and lower dosages can be used.
Botox Injection
- Another therapy that helps children with cerebral palsy temporarily lessen stiffness is Botox injections. It functions by obstructing the nerve impulses that initiate muscular contraction.
- Following Botox injections, stiffness reduction should ordinarily persist for three to six months. Its effects might, however, wear off sooner based on your child’s spasticity severity and the quantity administered.
- It’s critical to realize that Botox and muscle relaxants may not be the best choices for long-term use because they only offer temporary relief.
- Children with cerebral palsy (CP) should take advantage of their decreased spasticity when using Botox, and they should pursue an intense gait training program to enhance their form.
Orthotics
- Braces and splints are examples of orthotic devices that can support appropriate musculoskeletal alignment and form.
- Uncontrollable tightness in children might give rise to improper types of development. By using an orthosis, spastic muscles can be prevented from gradually becoming tighter.
- Furthermore, orthotic devices such as SWASH (Sitting Walking And Standing Hip) orthoses or de-rotation straps can assist in maintaining leg symmetry and preventing crossing.
Surgery
- Children with cerebral palsy who have different types of surgeries might not be as spastic. In our practice, surgery is reserved for the last resort, in cases where no other course of action is available or effective.
- For instance, in cases where there is no other option, children who walk with a scissoring gait may benefit from adductor lengthening surgery. It is required for increasing the inner thigh muscles.
- Spasticity can be reduced using a specific dorsal rhizotomy treatment. Muscle contractions can be stopped and prevented by a surgeon by removing the overactive nerve fibers. Once the nerve fibers are destroyed, the muscles cannot grow back, thus they will not become spastic.
Physical Therapy for the Scissor Gait
- Children who have always had a scissor gait may still retain it even if their spasticity is significantly reduced. While surgery, muscle relaxants, and nerve blockers can reduce stiffness, they cannot teach your child how to walk correctly.
- Your youngster will find it awkward to walk without their scissoring gait if that is all they have ever known. Children will need to go to physical therapy sessions and learn new walking techniques to improve their form.
- A physical therapist will evaluate the mobility of your child and provide a customized exercise program to help them with their gait. The more people walk with proper form, the more comfortable and strong the brain networks behind that movement pattern may become.
Specific Physical Therapy Procedures
- Stretching: Regular stretching helps increase the range of motion and flexibility of your muscles.
- Strengthening Activities: Certain activities might help strengthen tight or weak muscles that contribute to scissor gait.
- Enhancing one’s ability to balance can help people walk more steadily and lower their chance of falling. This may entail undertaking tasks such as one-legged standing and walking on uneven terrain.
- Using sensory feedback to enhance bodily awareness is known as proprioceptive training.
- Assistive aids, such as crutches or braces, can help support gait and lessen the effects of scissor gait in some situations.
- Many people who have limb spasticity have trouble balancing and may use a walker to help them move around.
- People can practice bearing weight on their legs by using a walker, which may improve circulation and strengthen their bones and muscles.
- Some walkers have elements like straps or cushions that may keep the legs apart to prevent them from scissoring.
Complications related to Scissor Gait
Scissor gait can lead to several problems, including:
- Fatigue: A scissor gait can be physically demanding and requires a lot of energy, which leads to fatigue.
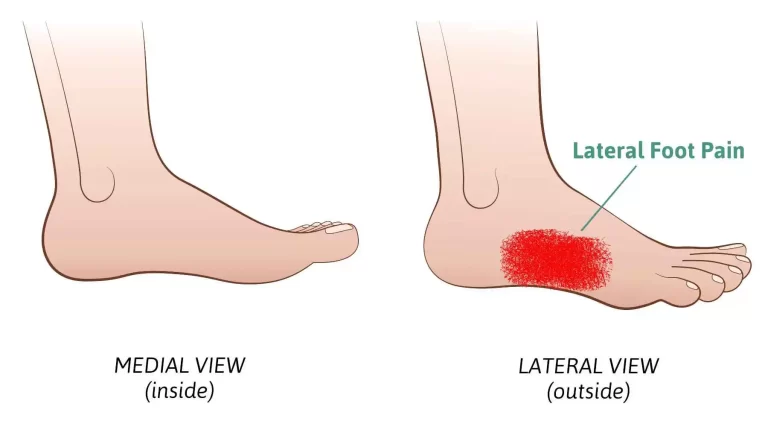
- Pain and discomfort: Persistent friction and leg crossing can cause pain and discomfort, which makes daily chores more challenging.
- Fall risk: Using a scissor motion when walking makes it harder to stay balanced, increasing the likelihood of tripping and falling.
- Decreased mobility: Playing sports, climbing stairs, walking long distances, and other physical activities may be challenging for those with a scissor gait since it restricts their legs’ range of motion.
- Social isolation: Due to walking-related issues, people with scissor gait might stay away from social gatherings and feel cut off from their peers.
- Restricted freedom: People with scissor gait impairments may be less independent and be forced to rely on others to assist them with daily tasks.
- Reduced quantity and quality of life: A person’s ability to work, interact with others, and follow their interests can all be significantly hampered by a scissor gait.
- Seeking medical help for scissor gait as soon as feasible is essential to minimizing these problems and improving results.
The dangers of an incorrectly managed Scissor Gait
The brain damage that causes cerebral palsy is a static disorder, which means that it won’t become worse with time. However, if cerebral palsy problems like spasticity are not adequately controlled, they may worsen.
The following are possible dangers linked to improperly controlled scissor gait:
- Abnormalities in development or stunted growth as a result of unequal muscular pull.
- Increased chance of falling as a result of inadequate balancing abilities.
- Knees rubbing against one another all the time increases the risk of pressure sores.
- A severely restricted degree of motion is caused by tight joints.
- Pain is caused by persistent joint strain and muscular tightness.
- Decrease in walking abilities.
Spasticity can get worse with age, but it can also be lessened with regular care. Seeking spasticity control as soon as possible is crucial to maximizing your child’s mobility. Children’s minds are more elastic than adult’s. This indicates that compared to adults, youngsters find it easier to adjust and develop new behaviors. Abnormal walking patterns can be replaced before they become set habits by practicing proper form and managing spasticity early.
Summary
A child that crosses their legs over one another when walking has a scissor gait. The gait generally suggests cerebral palsy, muscle weakness, stiffness, and other underlying problems. To identify the reason for the scissor gait, the doctor will conduct a comprehensive examination and may prescribe tests.
A scissoring gait can impair growth and balance if left untreated. Spasticity can get worse over time, so early intervention is crucial. Reducing spasticity and encouraging proper form are key components of managing scissoring gait effectively.
FAQs
What is a scissor gait?
A particular paraparetic spastic gait is distinguished by strongly toned adductor muscles. It is characterized by excessive adduction that causes the knees and thighs to hit, or occasionally even cross, in a scissors-like motion, along with hypertonia and flexion in the legs, hips, and pelvis.
Which symptoms are associated with scissoring?
A youngster with a scissoring gait walks in a characteristic way where their legs cross over one another with each stride, creating a scissor-like motion. This medical condition could indicate the presence of underlying musculoskeletal issues such as spasticity, contractures, or muscle weakness.
What does a scissoring gait represent?
When a child walks, their legs cross over one another, demonstrating a scissor gait. The gait usually suggests cerebral palsy, muscle weakness, stiffness, and other underlying diseases. To identify the reason for the scissor gait, the doctor will conduct a comprehensive examination and may prescribe tests.
Does scissoring indicate spasticity?
Overly strong deep tendon reflexes (such as the knee-jerk) clonus, or repetitive jerky movements, particularly in response to movement or touch. The process of scissoring involves folding the legs over as the scissors’ tips are linked together. The affected part of the body may be painful or deformed.
What are scissoring gait orthotics?
The orthotic device has blocks that are specifically made for it. To enable walking action, the blocks slide back and forth against one another during the gait cycle, fit pleasantly against the legs, and separate the legs. You can use belts for attaching the blocks to the legs.
References:
- Gait (scissors). (2018, January 1). https://gpnotebook.com/pages/uncategorised/gait-scissor
- Cota, B. B. (2022, May 4). Scissoring Gait and Cerebral Palsy: Causes, Risks, & Treatment. Flint Rehab. https://www.flintrehab.com/scissoring-gait-cerebral-palsy/
- Medical City Children’s Orthopedics & Spine Specialists. (2023c, December 9). Scissor Gait | Those with Cerebral Palsy | We treat this condition. https://medicalcitykidsortho.com/scissor-gait/
- Jain, W. B. D. J. K., & Jain, R. B. D. V. (2023, December 21). Scissor Gait – CP Case Study – Trishla Foundation. Trishla Foundation. https://www.trishlafoundation.com/scissor-gaits/
- Wikipedia contributors. (2023a, March 22). Scissor gait. Wikipedia. https://en.wikipedia.org/wiki/Scissor_gait
- Patel, D. (2023b, May 2). Scissor Gait – Cause, Treatment, Exercise, Gait Training. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/scissor-gait/#google_vignette