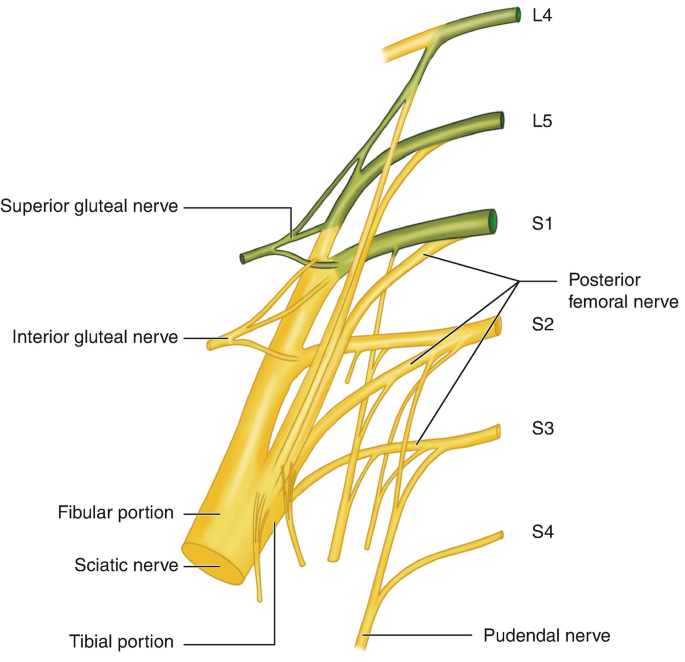
Sacral Plexus
Introduction
The sacral plexus is a neural network made up of the lumbosacral trunk (L4, L5) and the sacral spinal nerves (S1–S4).
The sacral plexus is situated on the posterior pelvic wall, behind the internal iliac arteries and ureter, and ahead of the piriformis muscle.
The plexus has multiple branches, including anterior, posterior, and one terminal branch. These branches give motor and sensory innervation to the posterior thigh, most of the lower leg, the whole foot, and a portion of the pelvis.
Structure
The sacral plexus is formed by:
- The lumbosacral trunk
- The anterior segment of the first sacral nerve.
- Parts of the anterior divisions of the second and third sacral nerves.
The nerves of the sacral plexus converge at the lower section of the larger sciatic foramen and form a flattened band with many branches emerging from its anterior and posterior sides. The band continues as the sciatic nerve, which splits on the back of the thigh into the tibial nerve and the common fibular nerve.
These two nerves may emerge independently from the plexus, and their independence can be demonstrated by dissection. The sacral and lumbar plexuses are occasionally united to produce a single large nerve plexus known as the lumbosacral plexus. The lumbosacral trunk joins the two plexuses.
Root
The sacral plexus is a neural network made up of the lumbosacral trunk and sacral spinal nerves. The lumbosacral trunk is created by the lumbar spinal neurons L4 and L5. The trunk then descends into the pelvis to reach the roots of sacral spinal nerves S1 through S4, which originate from the spinal cord.
Branches
The sacral plexus has several branches that may be categorized into three categories: posterior, anterior, and terminal. The posterior branches are derived from the posterior divisions of the spinal nerves’ anterior rami, whereas the anterior branches are generated from the anterior divisions. The sciatic nerve is the main and sole terminal branch, with two divisions: the tibial and common fibular (peroneal) nerves.
Posterior branches
Superior gluteal nerve
The superior gluteal nerve is composed of the posterior divisions of the anterior rami of the L4, L5, and S1 spinal nerves. It enters the gluteal area via the larger sciatic foramen, which is located on the superior border of the piriformis. The superior gluteal nerve then runs laterally beneath the gluteus medius, innervating the tensor fasciae latae, gluteus medius, and gluteus minimus muscles.
Inferior gluteal nerve
The posterior divisions of the anterior rami of the L5, S1, and S2 spinal nerves all contribute to the inferior gluteal nerve. It follows a similar course via the larger sciatic foramen but is inferior to the piriformis muscle. It goes superficially to the sciatic nerve and innervates the gluteus maximus muscle.
Perforating cutaneous nerve
The perforating cutaneous nerve is similarly made up of completely posterior divisions, this time coming from the fibers of the anterior rami of spinal nerves S2 and S3. It enters the larger sciatic foramen, above the gemelli and obturator internus, and pierces the sacrotuberous ligament and gluteus maximus. This nerve supplies cutaneously to a little region of skin on the inferior medial section of the buttock.
Pelvic splanchnic nerves
The pelvic splanchnic nerves branch from the anterior rami of spinal nerves S2, S3, and S4. They innervate the pelvic cavity and pelvic floor muscles both parasympathetically and motorically. The parasympathetic output connects to the inferior hypogastric (pelvic) plexus. Its motor component serves the bladder and the distal section of the large intestines (starting with the left colic flexure). It is also involved in clitoral (or penile) erection.
Nerve to piriformis
The nerve to the piriformis muscle originates from the dorsal branches of spinal nerves S1 and S2, or solely S2, and enters the muscle’s anterior surface to supply it.
Anterior branches
Nerve to quadratus femoris
The nerve to the quadratus femoris is derived from the anterior divisions of the anterior rami of spinal nerves L4, L5, and S1. The nerve goes inferiorly beneath the sciatic nerve, towards the quadratus femoris. Along the way, it supplies the inferior gemellus muscle and an articular branch to the hip joint.
Nerve to obturator internus
The nerve to the obturator internus originates from the anterior divisions of spinal nerves L5, S1, and S2. The nerve runs inferior to the piriformis and exits the pelvis by the larger sciatic foramen, where it sends a branch to innervate the superior gemellus muscle. It then travels around the ischial spine, re-entering the pelvis via the smaller sciatic foramen and piercing the obturator internus.
Posterior cutaneous nerve of the thigh
The posterior cutaneous nerve of the thigh (also called the posterior femoral cutaneous nerve) is the only other branch of the sacral plexus that receives fibers from both the anterior and posterior divisions of the anterior rami.
Its fibers originate from:
S1 and S2 spinal nerves’ anterior rami are divided posteriorly.
Anterior divisions of spinal nerves S2 and S3.
The nerve enters the posterior thigh through the larger sciatic notch, traveling below the piriformis, deep to the inferior gluteal artery, and above the Gemelli, obturator internus, and sciatic nerve.
The nerve has an anteroposterior and superior range of cutaneous and fascial supply between the anterior and posterior axillary lines, extending from the buttock to the middle of the calf muscle.
The posterior femoral cutaneous nerve also gives rise to gluteal branches, which provide cutaneous supply to the buttock contour, and perineal branches, which innervate the skin of the lateral perineum (two-thirds of the posterolateral aspect of the scrotum in males, or labium majus in females) and the adjacent region of the upper medial thigh.
Pudendal nerve
The pudendal nerve is formed when the anterior divisions of spinal nerves S2, S3, and S4 join on the anterior aspect of the piriformis (posterior to the inferior gluteal artery). The pudendal nerve passes inferiorly across the sacrospinous ligament before entering the pudendal canal alongside the pudendal vessels. The pudendal nerve gives rise to:
The inferior rectal nerve provides innervation to the external anal sphincter, anal canal, and perianal skin.
The perineal nerve provides cutaneous supply to a portion of the posterior scrotum (vulva), urethral and vaginal mucous membranes, and motor innervation to perineal muscles.
The dorsal nerve of the clitoris/penis, which supplies cutaneous innervation to this area.
Nerve connecting the levator ani and iliococcygeus muscles.
The sacral plexus’s last two branches are the nerves to the levator ani and iliococcygeus muscles. It gives motor innervation to the pelvic region of the muscles that bear their names.
Sciatic nerve
The sciatic nerve is the sacral plexus’s terminal and biggest branch, produced by the anterior and posterior divisions of the anterior rami of spinal nerves L4–S3.
The nerve exits the pelvic cavity through the larger sciatic foramen. It penetrates deep into the gluteus maximus and inferior gluteal artery. It runs along the posterior surface of the Gemelli, piriformis, quadratus femoris, and ischial fibers of the adductor muscle. The sciatic nerve begins to branch about halfway between the ischial tuberosity and the greater trochanter, supplying the hamstring muscles and adductor magnus ischial fibers.
At the tip of the popliteal fossa, the nerve usually separates into the common peroneal and tibial nerves. These two nerves innervate the muscles and joints of the leg and foot. The inferior gluteal artery supplies the sciatic nerve with vasa nervorum (a tiny artery that provides arterial blood to peripheral nerves).
Examination
Sensory testing detects lumbosacral radiculopathy with intermediate sensitivity. However, prior knowledge of MRI results might lead to bias.
In clinical practice, the diagnosis of lumbosacral radiculopathy should always be made using a combination of sensory, motor, and deep tendon reflex testing, rather than just one test result.
Clinical Importance
Lumbosacral Plexopathy
A lumbosacral plexopathy is a neurological illness that affects either the lumbar or sacral plexus. They are extremely uncommon disorders caused by nerve bundle injury.
A plexopathy is considered when symptoms cannot be pinpointed to a single nerve. Patients may have neuropathic symptoms, numbness or paralysis, and muscular atrophy.
One of the most common causes of lumbosacral plexopathy is diabetic amyotrophy, commonly known as lumbosacral radioplexus autophagy. In this case, elevated blood sugar levels harm the nerves. Another reason is idiopathic plexopathy, which is the lumbosacral counterpart of Parsonage-Turner syndrome (brachial plexus-related). Tumors and other local invasions can induce plexopathy by compressing the plexus.
Treatment is determined by the underlying cause of the symptoms. Tumors and space-occupying lesions should be eliminated whenever possible. High-dose corticosteroids can be beneficial in diabetic and idiopathic conditions.
FAQs
How many sacral plexus are there?
Keeping the nerve roots in order can be challenging, despite their small number of only seven. Here are a few strategies that might help you keep things straight. All the nerves of the sacral plexus originate from three nerve roots. Except for the sciatic nerve, which contains five nerve roots.
What is the easiest way to remember the sacral plexus branches?
When trying to recall the sequence in which the peripheral nerves of the sacral plexus appear, ‘Sassy Irish Sailors Pester Parrots’ can be beneficial, signifying ‘Superior (gluteal), Inferior (gluteal), Sciatic, Posterior (femoral), Pudendal’.
What are the symptoms of a sacral plexus injury?
Common symptoms of lumbosacral plexus injuries include pain in the lower back and buttocks that spread down the leg.
Sensory alterations affect the top of the foot.
Weakness in the outer thigh muscles.
Deep pelvic discomfort radiates down the front of the thighs.
What is a plexus made of?
Plexus is a network of nerve roots that join to form terminal branches. As ventral (motor) and dorsal (sensory) roots exit the spinal cord, they quickly converge within the spinal canal to create a spinal nerve.
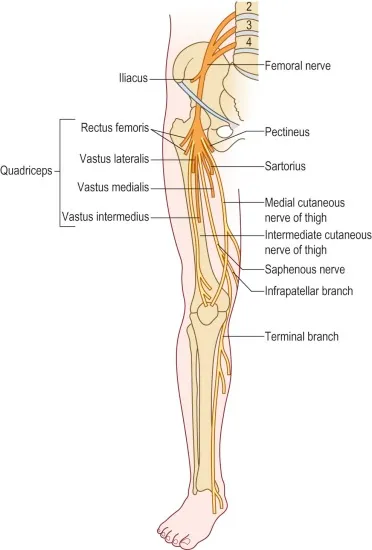
What nerves are found in the lumbosacral plexus?
The primary nerves that branch from the lumbar plexus include the iliohypogastric, ilioinguinal, genitofemoral, lateral femoral cutaneous, obturator, and femoral nerves as well as the lumbosacral trunk.
References
- Sacral plexus. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/sacral-plexus
- TeachMeAnatomy. (2023a, July 8). The sacral plexus – spinal nerves – branches – TeachMeAnatomy. https://teachmeanatomy.info/lower-limb/nerves/sacral-plexus/
- Wikipedia contributors. (2024f, October 13). Sacral plexus. Wikipedia. https://en.wikipedia.org/wiki/Sacral_plexus


One Comment