Pulmonary Embolism
Introduction
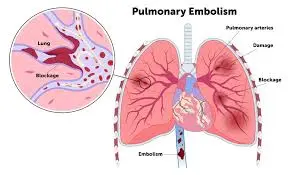
Pulmonary embolism (PE) is a life-threatening condition that occurs when a blood clot, usually from the deep veins of the legs (deep vein thrombosis), travels to the lungs and blocks blood flow. This can lead to shortness of breath, chest pain, and rapid heart rate.
PE requires urgent medical attention and is typically treated with anticoagulants or, in severe cases, thrombolytic therapy.
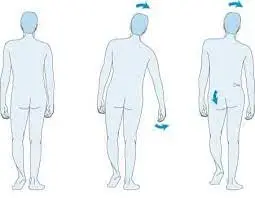
The blood clot typically begins in a vein that is deep in the leg and moves to the lung. In rare instances, the clot may form in a vein in a different area of the body. Deep vein thrombosis, also known as DVT, is the term used to describe a blood clot that develops in one or more of the body’s deep veins.
A pulmonary embolism can be fatal whenever one or more clots obstruct blood flow to the lungs. However, the chance of death is significantly decreased with early treatment. You can reduce your risk of pulmonary embolism by taking precautions against hemorrhaging in your legs.
A disorder where a blood clot blocks any number of arteries in the lungs. Blood clots that originate in the legs or, less frequently, other regions of the body (deep vein thrombosis, or DVT) are the most common cause of pulmonary embolisms. Chest pain, coughing, and shortness of breath are some of the symptoms.
The risk of death is significantly decreased by prompt treatment to break up the clot. Blood thinners, medications, or procedures can be used for this. Physical activity and compression stockings can help stop clots from developing in their initial place.
The Pathological Process
Particularly at the calf, stasis in the deep veins causes thrombus development. The degree of alterations in pulmonary blood flow and respiration depends on the patient’s initial cardiorespiratory condition as well as the size and quantity of emboli. A massive embolus can be lethal, yet a modest blockage of the pulmonary artery might not cause any symptoms.
In the latter instance, pulmonary embolism results in a mismatch between ventilation and perfusion, which raises pulmonary artery pressures and right ventricular effort. This leads to wasteful ventilation as it increases the dead space in the alveoli. As a result of a reduction in blood volume and coronary circulation to the left ventricle, the right heart eventually fails, followed by the left.
A Pulmonary Embolism: What Is It?
A blood clot in one of your lung’s blood arteries is called a pulmonary embolism (PE). This occurs when a clot from another area of your body, usually your arm or leg, travels to your lungs through your veins. A PE raises blood pressure in your pulmonary arteries, decreases oxygen levels in your lungs, and limits blood flow to your lungs.
An embolus is a blood clot that starts in a blood vessel in one part of the body, breaks off, and moves via the blood to another part of the body. A blood artery may become lodged with an embolus. An organ’s blood supply may be cut off as a result. An embolism occurs when an embolus blocks a blood artery.
The circulatory system of the body is composed of the heart, arteries, capillaries, and veins. The heart pumps blood into the arteries with tremendous force. Blood then enters the capillaries, which are microscopic blood arteries found in tissues. Blood is returned to the heart via the veins. Blood flow slows as it returns to the heart through the veins. A clot may occasionally form as a result of this slowed blood flow.
This is a serious medical situation. A pulmonary embolism can harm the heart or lungs and potentially result in death if treatment is delayed. Approximately one-third of pulmonary embolism victims pass away before receiving a diagnosis and treatment.
An embolism in the lungs can:
- Harm your lungs.
- Cause heart failure by putting stress on your heart.
- Depending on the size of the clot, it could be fatal.
- PE is rarely lethal if diagnosed and treated promptly.
What is the prevalence of Pulmonary Embolism?
One of the most prevalent heart and blood vessel conditions worldwide is pulmonary embolism. After heart attacks and strokes, it comes in third. Approximately 900,000 persons in the US receive a PE each year.
Causes
A pulmonary embolism happens when a mass, usually a blood clot, becomes lodged in a lung artery, obstructing blood flow. The most common cause of blood clots is deep vein thrombosis, which occurs in the deep veins in your legs.
There are frequently several clots involved. Each clogged artery prevents blood flow to certain parts of the lung, which could result in death. Pulmonary infarction is a term for this condition. Your lungs have a harder time supplying oxygen to the rest of your body as a result.
Blood “pooling” or accumulating in a specific area of your body, generally your arm or leg. After extended periods of inactivity, such as following surgery, bed rest, or a lengthy travel or plane ride, blood typically pools.
Damage to a vein, such as from surgery or a fracture (particularly in your leg, hip, knee, or pelvis). Other illnesses, such as cardiovascular disease (which includes heart attacks, strokes, atrial fibrillation, and congestive heart failure).
A change in the clotting factors in your blood. Certain cancers and those undergoing treatment with hormone replacement or birth control tablets may have elevated clotting factors. Blood clotting disorders can also result in abnormal or decreased clotting factors.
Sometimes things other than blood clots induce blockages in the blood vessels, including:
- The inside fat of a fractured long bone
- A portion of a tumor
- Bubbles of air
Signs and symptoms
The degree of lung involvement, the size of your blood clots, and whether you have preexisting heart or lung illness can all affect the symptoms of a pulmonary embolism.
Typical signs and symptoms include:
- Breathlessness. Usually, this symptom manifests abruptly. Breathing difficulties occur even when you’re at rest and worsen when you move.
- Chest discomfort. You can experience what feels like a heart attack. When you take a big breath, the sensation of pain is often intense. You may be unable to take a deep breath because of the pain. Additionally, you might feel it while you lean over, bend, or cough.
- Fainting. If your blood pressure or heart rate suddenly drops, you could faint. We refer to this as syncope.
Additional signs and symptoms of a pulmonary embolism include:
- Coughing out mucous that may be bloody or splattered with blood
- An erratic or fast heartbeat
- Dizziness or lightheadedness
- Sweating excessively
- A fever
- Usually located in the rear of the lower thigh, leg pain, edema, or both.
- Cyanosis is characterized by clammy or discolored skin.
Risk Factor
Blood clots that cause a pulmonary embolism can happen to anyone, but some things can make you more susceptible.
Which factors increase the risk of a pulmonary embolism?
Individuals who are susceptible to PE include those who:
- Have deep vein thrombosis (DVT), or a blood clot in their leg.
- Are not active for extended periods when traveling by airline, rail, or automobile (e.g., a long, cross-country car excursion).
- Have lately experienced vascular stress or injury, maybe as a result of varicose veins, fractures, or surgery.
- Are utilizing hormone replacement treatment or hormonal-based contraception, such as Birth control pills, patches, or rings.
- Suffer from a blood clotting condition.
- Have a blood clot history in your family.
- Smoking.
- Possess diabetes.
- Cancer.
- Possess a history of heart attacks, strokes, or heart failure.
- Possess either obesity (body mass index, or BMI) or overweight (BMI greater than 25).
- Have either given birth within the last six weeks or are pregnant.
- Had a central vein disease catheter inserted into their leg or arm.
- Your healthcare practitioner can take action to lower your risk of PE if you have experienced a blood clot and have any of these risk factors.
Health issues and therapies
You are at risk from certain medical diseases and treatments, including:
- Heart condition. Diseases of the heart and blood vessels, particularly heart failure, increase the risk of clot development.
- Cancer. Blood clot risk can be increased by certain malignancies, including those of the brain, ovaries, pancreas, colon, stomach, lung, and kidneys, as well as tumors that have disseminated. The danger is considerably increased by chemotherapy. Additionally, taking tamoxifen or raloxifene (Evita) and having a personal or family history of breast cancer increases your risk of blood clots.
- Surgery. One of the main causes of problematic blood clots is surgery. Because of this, clot-preventive medications may be used both before and after major surgery, like joint replacement.
- Conditions that impact coagulation. Blood is impacted by certain hereditary conditions, which increases the risk of clotting. Blood clot risk might also be increased by other medical conditions, such as kidney illness.
COVID-19 is the coronavirus disease of 2019. A pulmonary embolism is more likely to occur in people with severe COVID-19 symptoms.
Long stretches of inactivity
Longer than typical durations of inactivity increase the risk of blood clots, including:
- Rest in bed. Blood clots can occur if you are bedridden for a long time following surgery, a heart attack, a limb fracture, trauma, or any other major disease. Long lengths of time spent with your legs flat might cause blood to pool in your legs when the veins’ flow slows down. Blood clots may occasionally arise from this.
- Lengthy journeys. During long flights or vehicle rides, sitting in a tight spot reduces blood flow in the legs, increasing the risk of blood clots.
Additional risk factors
- Smoking. Some persons, particularly those with existing risk factors, are more susceptible to blood clots due to tobacco use for unclear reasons.
- Being overweight. Being overweight raises the chance of blood clots, especially in those who have other risk factors.
- Extra estrogen. Particularly in people who smoke or are overweight, the estrogen in birth control tablets and hormone replacement therapy can raise blood clotting factors.
- Pregnancy. Blood returns from the legs may be slowed by the baby’s weight resting against pelvic veins. When blood pools or slows, clots become more likely to form.
Issues
The consequences of a pulmonary embolism can be deadly. Approximately one-third of patients who have an untreated and undetected pulmonary embolism do not make it out alive. However, that number sharply declines when the illness is identified and treated quickly.
Additionally, pulmonary embolisms may result in pulmonary hypertension, a condition where the right side of the heart and lungs have excessively high blood pressure. Your heart has to work harder to pump blood through the arteries in your lungs when there are blockages in those vessels. Eventually, this weakens your heart and raises blood pressure.
Rarely, do tiny clots known as emboli stay in the lungs, and over time, the pulmonary arteries become scarred. This causes persistent pulmonary hypertension by limiting blood flow.
One consequence of a pulmonary embolism is:
- Cyanosis.
- Heart attack.
- Stroke.
- Hypertension of the lungs.
- Pulmonary infarction, or death of lung tissue.
Prevention
Pulmonary embolisms can be avoided by avoiding clots in your legs’ deep veins. Because of this, the majority of hospitals take strong steps to avoid blood clots, such as:
- Anticoagulants, or blood thinners. Before and after surgery, these medications are frequently administered to patients who are at risk of clotting. Additionally, they are frequently administered to hospitalized patients with certain medical disorders, such as heart attacks, strokes, or cancer complications.
- Compression stockings. By gradually squeezing the legs, compression stockings improve the efficiency of blood flow through the veins and leg muscles. They provide a straightforward, affordable, and safe method of preventing blood from accumulating in the legs both during and after surgery.
- Raising the legs. When at all feasible, and especially at night, elevate your legs. Use books or blocks to raise the bottom of your bed 4 to 6 inches (10 to 15 cm).
- Engaging in physical exercise. Getting moving as soon as possible after surgery can speed up recovery in general and help prevent pulmonary embolism. This is the primary reason your nurse might encourage you to get up and move on the day of surgery, even though the area where your surgical incision is hurting.
- Compression by pneumatics. During this procedure, thigh-high or calf-high handcuffs are used, which automatically fill with air and release it every few minutes. This promotes blood flow by squeezing and massaging your legs’ veins.
Precautions when traveling
Blood clots are rare when traveling, although they become more likely as long-distance travel grows. Consult your healthcare practitioner if you have blood clot risk factors and are worried about traveling.
To assist avoid blood clots when traveling, your healthcare practitioner may recommend the following:
- Be sure to stay hydrated. The greatest liquid for avoiding dehydration, which can hasten the formation of blood clots, is water. Steer clear of alcohol, which causes fluid loss.
- Stop sitting for a moment. Every hour or so, take a stroll around the aircraft cabin. Stop occasionally while driving and take a few short walks around the vehicle. Bend your knees deeply a couple of times.
- Get up from your chair. Every 15 to 30 minutes, lift your toes up and down and bend and move your ankles in circles.
- Put on supportive stockings. To encourage fluid mobility and circulation in your legs, your doctor might suggest these. Compression stockings come in a variety of fashionable hues and textures. To assist you in putting on the stockings, there are even gadgets known as stocking butlers.
Testing and Diagnosis
How do you diagnose a pulmonary embolism?
A healthcare professional will conduct the following tests to diagnose PE after reviewing your symptoms and risk factors:
CT Scan
CAT scan or computed tomography. This imaging exam creates fine-grained images of the body using X-rays and a computer. A CT scan provides information on the organs, muscles, fat, and bones. A contrast-enhanced CT scan improves the view of the lungs’ blood arteries. A dye-like material called contrast is injected into a vein to make the organ or tissue being studied more visible in the image.
Lung angiography.
Aneurysms (bulging of the blood vessels), stenosis (narrowing of the blood vessels), and blockages are among the problems that can be assessed using this X-ray image of the blood vessels. A tiny, flexible tube is inserted into an artery to administer a dye (contrast). On X-rays, this dye makes the blood vessels visible.
MRI
MRI stands for magnetic resonance imaging. This imaging test creates fine-grained images of the body’s organs and structures by combining radio frequencies, a magnetic field, and a computer.
US or duplex ultrasound
The purpose of this kind of vascular ultrasonography is to evaluate the structure and blood flow in the legs’ blood arteries. (It is common for blood clots from the legs to come loose and enter the lungs.) The US creates images of blood arteries, tissues, and organs using a computer and high-frequency sound waves.
Chest X-ray.
This imaging examination evaluates the heart and lungs. Information on the size, form, contour, and anatomical location of the cardiovascular system, lungs, aorta, pulmonary arteries, bronchi (big breathing tubes), and The middle part of the (area in the very center of the chest separates the lungs) can be seen on a chest X-ray.
Ventilation-perfusion V/Q
V/Q scan, or ventilation-perfusion scan. A tiny quantity of radioactive material is utilized to aid in the examination of the lungs during this nuclear radiology test. The flow of air into and out of the bronchi and bronchioles is measured using a ventilation scan. A perfusion scan assesses the lungs’ blood flow.
Laboratory examinations
Blood tests, such as the D-dimer level test, are used to determine the blood’s ability to clot. Testing for genetic abnormalities that could lead to irregular blood clotting may be part of further blood work. The amount of oxygen in the blood can be determined by measuring arterial blood gases.
Electrocardiogram
EKG stands for electrocardiogram. One of the quickest and easiest exams for assessing the heart is this one. Certain locations on the arms, legs, and chest are equipped with electrodes, which are tiny, sticky patches. Lead wires are used to connect the electrodes to an EKG machine. They measure, evaluate, and print the heart’s electrical activity.
Handling and Therapy
How do you treat a pulmonary embolism?
To keep a careful eye on your condition, medical professionals typically treat PE patients in hospitals. The degree of seriousness of the clot will determine how long your hospital stay and treatment for a pulmonary embolism will last. It might not be necessary for some folks to stay overnight. A pulmonary embolism, or pneumonia, is mostly treated with an anticoagulant, which is a blood thinner.
To increase blood flow within your pulmonary arteries, you might also have surgery, thrombolytic therapy, or interventional procedures, depending on the extent of the clot and how it affects other organs like your heart.
Anticoagulant drugs
The majority of the time, anticoagulant drugs (blood thinners) are used as treatment. Blood clotting is impeded by anticoagulants. This stops blood clots in the future. Like any medication, it’s critical to know when and how to take your thrombin and to adhere to your doctor’s instructions.
The kind of medication you take, how long you must take it, and the kind of follow-up surveillance you require will all depend on your diagnosis. For the laboratory and your provider to track how you are responding to the medication, make sure you maintain all of your follow-up appointments.
Prothrombin time tests, which measure how quickly blood clots, may be part of your follow-up when taking anticoagulants. This aids in determining whether you’re taking the recommended dosage.
Stockings with compression
Your legs’ blood flow is improved by compression stockings, often known as support hoses. They are frequently used by people who have deep vein thrombosis. Utilize them as prescribed by your physician. Typically knee-length, the stockings compress your legs to keep blood from accumulating.
Consult your healthcare practitioner about the proper usage, duration, and maintenance of your compression stockings. To keep compression stockings from getting damaged, it’s crucial to wash them as directed.
Treatment with fibrinolytics. These medications, often known as clot busters, are administered intravenously (IV) or intravenously (IV) to dissolve a clot. Only life-threatening circumstances call for the use of these medications.
Vena cava filter
To prevent clots from reaching the lungs, a tiny metal device may be inserted into the vena cava, the big blood channel that returns oxygen from the body to the heart.
Embolectomy of the lung
This type of surgery to remove a PE is rarely employed. Only in extreme situations—when your PE is very large, you are unable to receive anticoagulation and/or thrombolytic treatment because of other health issues, you have not responded well to those therapies, or your condition is unstable—is it usually done?
Thrombectomy by percutaneous means.
With X-ray guidance, a long, slender, and hollow tube (called a catheter can be inserted down the blood vessel to the embolism location. After the catheter is positioned, thrombolytic medication is used to dissolve the embolism, split it up, or draw it out.
Preventive therapy is a crucial part of PE treatment because it stops new emboli from forming.
Methods
Your doctor could suggest surgery or a tube to remove the blood blockage from your pulmonary artery if a PE is life-threatening or if no other therapies are working. Another alternative is thrombolytic treatment. Additionally, your doctor can suggest an interventional treatment when a filter is inserted into the biggest vein in your body. Before clots reach your lungs, they are caught by a vena cava filter.
Thrombolytic treatment
The clot is broken up using thrombolytic drugs, also known as “clot busters,” such as tissue plasminogen activator (TPA). Thrombolytics are always administered in a hospital’s emergency room intensive care unit, or ICU so that a healthcare professional can keep an eye on you. If you have a unique circumstance, such as high blood pressure or an unstable state due to pulmonary embolism, you might be prescribed this kind of drug.
Implications for Physiotherapy
After PE, mobility is essential to the patient’s recuperation. Bed rest and inpatient therapy are usually recommended after anticoagulation and thrombolytic treatments. Restoring a clean lung field and adequate oxygen uptake is the primary goal of physical therapy. Chest physical therapy can do this, and it can be advanced to incorporate endurance exercises including walking g or motorcycle ergometry.
Prognosis and Outlook
In the event of a pulmonary embolism, what can I anticipate?
An embolism of the lungs is a highly hazardous ailment that can cause death or chronic sickness if left untreated. A few hours after an embolism of the lungs occurs, some people pass away unexpectedly. This may occur before a diagnosis is made by a healthcare provider.
If you happen to have a coronary or lung problem, you are more likely to die from a PE. Even so, just 1% to 3% of patients who have a pulmonary embolism die from it, thanks to improved imaging techniques compared to earlier times.
Your overall health, the size of the blood clots and blockages, and the efficiency of your heart’s pumping action all affect your prognosis (outlook) after treatment.
Treatment-related complications or adverse effects
One potential adverse effect of drugs used to treat pulmonary emboli is bleeding. Your doctor will prescribe the appropriate dosage of thrombolytics or anticoagulants based on your circumstances. They can keep an eye on your condition by maintaining you in the hospital.
How quickly will I get better following treatment?
After a week of treatment, you ought to feel better. However, it may take months or even years for a pulmonary embolism to fully disappear.
Your heart must exert more effort to counteract the decreased blood flow and elevated blood pressure caused by PE. Months later, some patients also struggle to restore normal function in one of their heart chambers as a result of this. As a result, individuals can no longer tolerate as much physical exertion as they could before their pulmonary embolism.
Is it possible to avoid a pulmonary embolism?
You might be able to stop it, yes. A pulmonary embolism can be avoided in the following ways:
- Engaging in regular exercise. Spend a few minutes each hour moving your arms, legs, and feet if you are unable to walk around. Compression stockings might help promote blood flow if you know you’ll be sitting or standing for extended periods.
- Consuming a lot of water while avoiding alcohol and coffee.
- Avoiding tobacco products.
- Don’t cross your legs.
- Not dressing in apparel that is too tight.
- Reaching a healthy weight for yourself.
- Twice a day, spend 30 minutes elevating your feet.
- Discuss lowering your risk factors with your healthcare professional, particularly if you or any family members have experienced a blood clot.
Important facts about pulmonary embolisms A pulmonary embolism (PE) is a blood clot that forms in a blood vessel elsewhere in the body (usually the leg), travels to an artery in the lung, and then abruptly blocks the artery. Abnormal blood clots can form because of things like “sluggish” blood flow through the veins, abnormalities in clot-forming factors, and/or damage to the blood vessel wall. A wide range of conditions and risk factors have been associated with pulmonary embolisms, and the most common symptom of PE is sudden shortness of breath. PE is frequently challenging to diagnose because its signs and symptoms are similar to those of many other conditions and diseases.
FAQs
What is a pulmonary embolism’s primary cause?
A narrowed artery in the lungs is the cause of a pulmonary embolism. A blood clot that starts in a deep vein in the leg and moves to the lungs, where it lodges in a smaller lung artery, is the most frequent cause of this kind of blockage. The deep veins in the legs are where nearly all clots from forming that result in pulmonary embolism originate.
Is it possible to cure a pulmonary embolism?
The expectation is that your body will eventually break up the clot on its own. More harsh treatments might be required if it doesn’t. During hospitalization, an injection is administered; however, upon discharge, the patient will switch to a tablet regimen.
How may a pulmonary embolism be prevented?
Keeping up a nutritious diet.
Regular exercise.
When sitting or standing for extended periods (especially on long-haul flights), move your arms and legs frequently to control your weight.
Giving up smoking.
Consuming a lot of water.
How does one feel like a PE?
Breathlessness and chest ache that worsen with exertion or deep breathing are typically the initial symptoms of a pulmonary embolism. You should seek medical help immediately if you experience these symptoms. Although extremely treatable, pulmonary embolism is a dangerous condition. The likelihood of mortality is significantly decreased by prompt treatment.
Who is most vulnerable to pulmonary embolism?
Older age. Cancer as well as cancer treatment. Several illnesses include inflammatory bowel disease, high blood pressure, stroke, heart failure, and chronic obstructive pulmonary disease (COPD). Some medications include estrogen replacement treatment and birth control pills.
Is it possible to avoid blood clots by walking?
One of the best ways to prevent clots is to be active. When traveling, make sure to take lots of pauses. Every thirty minutes or so during lengthy automobile rides, get out of the vehicle and take a stroll. Every hour, if you can, get up from your seat as well as walk up or down the aisle on the bus, airplane, or train.
What are the initial symptoms of a pulmonary blood clot?
You could assume you’re experiencing a heart attack because of the intense chest discomfort that gets worse when you breathe in.
Dizziness, lightheadedness, or fainting as a result of an abrupt drop in blood pressure.
Cough, which could be bloody.
What causes blood clots?
The body uses blood clots to stop bleeding from injured blood vessels and aid in the healing process. Your body may acquire them as a result of trauma or injury sustained during operations or other medical treatments. They may also develop as a result of atherosclerosis, which is artery damage.
References
- Pulmonary embolism – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/pulmonary-embolism/symptoms-causes/syc-20354647
- Pulmonary embolism. (2024, December 30). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17400-pulmonary-embolism
- Pulmonary embolism. (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/pulmonary-embolism



6 Comments