Pseudogout
What is a Pseudogout?
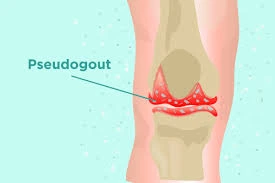
Pseudogout (calcium pyrophosphate deposition disease, CPPD) is a type of arthritis characterized by sudden, painful swelling in one or more joints, often the knee. It is caused by the deposition of calcium pyrophosphate crystals in the joint cartilage, leading to inflammation.
Symptoms resemble those of gout, but instead of uric acid crystals, calcium pyrophosphate crystals are involved. Diagnosis is typically made through joint fluid analysis and imaging.
Treatment focuses on relieving pain and inflammation, often with nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, or corticosteroids. Unlike gout, there is no specific treatment to reduce crystal deposits.
The knees are the most common joint affected by this ailment, however other joints may also be impacted. Adults over 60 are more likely to have it. Another name for pseudogout is calcium pyrophosphate deposition disease (CPPD).
Pseudogout is a type of arthritis that causes your joints to become stiff, swell, and hurt all at once. Because it produces symptoms that are similar to gout and come and go, it is known as pseudogout. An excess of uric acid in the blood leads to gout. Pseudogout is caused by an accumulation of calcium pyrophosphate dihydrate (CPP).
Older people are typically affected by pseudogout. Although calcium pyrophosphate crystals can cause arthritis in both men and women, men are more likely to develop pseudogout. Although it may not have a clear origin, pseudogout can occasionally occur in the context of trauma, surgery, or an acute medical condition. Although it usually affects the knee, it can also affect the shoulders, elbows, wrists, ankles, and feet.
Pseudogout is a type of arthritis that causes your joints to swell and hurt all at once.
A longer-term ailment known as chronic CPP crystal inflammatory arthritis also exists. It is known as osteoarthritis with CPPD when symptoms are present in certain individuals who have osteoarthritis and CPPD.
Although pseudogout can occur in any joint in the body, it most frequently occurs in:
- Knees.
- Hands and wrists.
- Shoulders.
- Hips and pelvis.
- Elbows.
- Ankles.
Other names for pseudogout are also used by medical professionals, such as:
- Calcium pyrophosphate deposition (CPPD).
- Calcium pyrophosphate arthritis.
- Chondrocalcinosis.
- The condition is referred to by all of these names.
Causes
Crystals of calcium pyrophosphate dihydrate have been connected to pseudogout in the affected joint. As people age, these crystals become increasingly common; over half of those over 85 have them. However, the majority of persons with these crystal deposits never get pseudogout. The reason why some people experience symptoms while others do not is unclear.
When calcium pyrophosphate crystals develop in the joint synovial fluid, pseudogout results. Additionally, crystals may accumulate in the cartilage and harm it. A crystal buildup in the joint fluid causes severe discomfort and swollen joints.
Pseudogout is caused by an accumulation of calcium pyrophosphate (CPP) in the affected joints. The excess CPP accumulates as tiny crystals in the fluid-filled synovial membranes and cartilage that cushion your joints. The symptoms of pseudogout flare up when the CPP crystals eventually clump together inside your joints.
The reason why your body produces more CPP is unknown to experts. According to certain research, pseudogout may be inherited, which means that parents may expose their biological children to the danger of getting it. It can develop in some persons following trauma or a joint-damaging accident. Pseudogout may be caused by specific metabolic or endocrine disorders, according to experts.
Calcium pyrophosphate crystals are found in the cartilage and joint fluid of many persons, particularly the elderly. The crystals might remain there indefinitely without harming anything. However, these crystals can occasionally cause an abrupt and severe inflammatory response for unknown causes.
As if they were bacteria entering the joint, white blood cells rush into the joint area and attempt to eliminate the crystals. This results in noticeable pain, swelling, warmth, and redness. Sometimes it happens for no apparent cause, but it is more likely to happen when there is physiologic stress, like after surgery or an acute medical sickness.
Many medical practitioners consider pseudogout to be a genetic disorder because it frequently runs in families. Additional contributing elements could be:
- Hypothyroidism, or an underactive thyroid.
- Hyperparathyroidism, or an overactive parathyroid gland.
- Excess iron in the blood.
- An excess of calcium in the blood is known as hypercalcemia.
- Magnesium deficiency.
Symptoms
The knees are most frequently affected by pseudogout. It affects the ankles and wrists less frequently.
The following are the most typical signs of pseudogout:
- Sudden, intense joint pain.
- Skin discoloration or redness.
- Swelling.
- Stiffness.
- Fluid buildup around the joint
- Chronic inflammation
A sensation of warmth or heat in or near a joint.
Flares or attacks are instances in which pseudogout symptoms occur and then disappear. Pseudogout attacks can occur without warning. Instead of experiencing symptoms gradually increasing over time, you will typically notice them all at once. The duration of a pseudogout flare-up might range from a few days to several weeks (or more).
Warmth, redness, swelling, and excruciating pain gradually appear in a joint over a few hours or a day in pseudogout. Usually, it just affects one joint. Although most other joints can be impacted, the knee is the one that is most frequently affected. Multiple joints being impacted at once is less frequent but still feasible. Sometimes the patient will also get a low-grade temperature. Even in the absence of medication, these symptoms usually go away in a week.
However, you should consult your physician immediately if you suffer from the above-described joint irritation. From the exterior, it is impossible to discriminate between different types of arthritis; for instance, pseudogout, gout, and infection are all identical. However, different types of arthritis require different treatments, and antibiotics are immediately needed for infections.
Risk factors
The following variables may raise your risk of developing pseudogout:
- Age. As one ages, the likelihood of acquiring pseudogout rises.
- Injuries to the joints. Pseudogout is more likely to develop in a joint that has had trauma, such as a major injury or surgery.
- Genetic illness. Members of some families are predisposed to developing pseudogout. Pseudogout tends to strike these individuals earlier in life.
- Imbalances in minerals. People who have too much calcium or iron in their blood or too little magnesium are more likely to develop pseudogout.
- Other health issues. An underactive thyroid or an overactive parathyroid gland has also been connected to pseudogout.
Although pseudogout can strike anyone, it is far more common in those over 65. Your risk of developing pseudogout may be increased by certain medical problems, such as:
- Hypomagnesemia.
- Hyperparathyroidism.
- Thyroid disease.
- Hemochromatosis (iron overload).
- Hypophosphatasia.
- Osteopenia.
- Chronic kidney disease (CKD).
Pseudogout may also be more common in people with other forms of arthritis, such as:
- Gout.
- Osteoarthritis.
- Rheumatoid arthritis.
- Post-traumatic arthritis.
Diagnosis
How is pseudogout diagnosed by medical professionals?
A physical examination and a few tests will be used by a medical professional to diagnose pseudogout. In addition to examining your joints, your healthcare practitioner will inquire about your symptoms. Inform your provider:
- When symptoms first appeared.
- If the symptoms appear to be intermittent.
- Whether certain activities or times of day appear to exacerbate (or alleviate) the symptoms.
To make sure you have more CPP crystals in your joint fluid, your doctor could do an arthrocentesis, or joint aspiration. After inserting a needle into your joint and extracting some fluid, they will send the sample to a laboratory. A lab technician will use a microscope to examine the joint fluid sample.
The most reliable method of confirming pseudogout is often to look for extra CPP crystals in your joint fluid following an aspiration.
Aspirating a joint can be painful, particularly if you have significant joint symptoms. To help you feel less pain during the aspiration, your doctor may prescribe numbing medicine.
Imaging tests may also be used by your provider to check for chondrocalcinosis, which is a marker of CPP accumulation. Your healthcare professional may use the following tools to obtain images of your joints and surrounding tissue:
- An examination of joint fluid by extracting it from the joint (arthrocentesis) to detect crystals of calcium pyrophosphate
- X-rays.
- CT scan (computed tomography scan).
- MRI (magnetic resonance imaging).
- Ultrasound.
This ailment can occasionally be misinterpreted as the following since it shares symptoms with other conditions:
- Rheumatoid arthritis (RA), a chronic inflammatory condition that can impact multiple organs and tissues, and osteoarthritis (OA), a degenerative joint disease caused by cartilage loss
- Gout, which frequently results in excruciating inflammation of the toes and feet but can also impact other areas
Treatment
Gout and pseudogout improve faster with medication, even though they usually go away on their own without therapy. Additionally, someone who experiences gout or pseudogout frequently would want to take medication every day to avoid more bouts.
To enable the most effective treatment strategy, a precise diagnosis of pseudogout is essential. The intensity of your symptoms, along with your other medical conditions and medications, will all play a role in selecting the best course of action.
Acute episodes of pseudogout can be treated with three different types of medications. Nonsteroidal anti-inflammatory medications, like naproxen or ibuprofen, work well. Additionally, colchicine can reduce inflammation.
Steroids are also quite effective, whether taken orally or injected directly into the joint. Nevertheless, each of these medications has advantages and disadvantages, and each patient should receive treatment that is specific to them. The same drugs can be used to stop pseudogout attacks if a person experiences them frequently.
Medical Treatment
To control your symptoms and lessen the frequency of your pseudogout spells, your doctor will recommend therapies. Medications are the most often used therapies, and they include:
- NSAIDs: Ibuprofen and naproxen are examples of over-the-counter NSAIDs (nonsteroidal anti-inflammatory medications) that reduce inflammation and relieve pain. Not everyone can safely take NSAIDs, particularly if they have specific medical issues. Before beginning an NSAID regimen or taking them for longer than ten days in a row, consult your doctor.
- Corticosteroids: These anti-inflammatory drugs are prescribed by doctors. Your doctor may prescribe oral medications or administer a cortisone injection straight into the affected joint.
- Colchicine: Colchicine is a prescription drug that lowers pain and inflammation. It works particularly well if taken within 24 hours of the onset of a pseudogout bout. To lessen the frequency of your symptom flares, your doctor can advise you to take a low dose for an extended length of time.
- Biologic injections: To treat pseudogout attacks, your doctor might recommend canakinumab or anakinra injections. Colchicine functions similarly to these medicinal drugs. The U.S. Food and Drug Administration (FDA) has approved them to treat various forms of arthritis, but they are not yet authorized to treat pseudogout. This implies that they can be more costly than alternative treatment choices and that your insurance might not cover them.
Other medications used to treat pseudogout include:
- Hydroxychloroquine (Plaquenil, Quineprox)
- Methotrexate (Rheumatrex, Trexall)
- Anakinra
Your doctor may suggest lifestyle modifications in addition to medicine to help control your symptoms and lower your chance of experiencing another gout episode. For instance, your physician might advise you to:
- Reduce your alcohol intake, if you drink.
- Lose weight, if you’re overweight.
- Quit smoking, if you smoke.
Moreover, certain alternative medical treatments have also demonstrated potential.
Physical Therapy
The pain, swelling, and lack of movement that come with pseudogout can be alleviated with physical therapy. Both acute and chronic pseudogout symptoms may be significantly reduced by seeing a physical therapist.
Rice protocol
- Rest, ice, compression, and elevation are referred to as Rice.
- Rice, a popular at-home remedy for minor injuries including sprains and twists, may be known to you.
- Rice is also a good at-home remedy for swelling, inflammation, and joint discomfort.
Rest
- Taking a day or two off from your regular physical activities will help you rest your joints. Altering routine physical activities and movements is another way to give your joints a break.
- Your physical therapist can demonstrate various techniques, equipment, postures, and movements that can help relieve joint stress.
Ice
- Applying a cold compress to your joints can help minimize pain and swelling. When you have chronic pseudogout, cold can help you focus on something else and lessen the intensity of your suffering.
- Try soaking a towel in cold water or placing some ice in a tiny plastic bag if you don’t have a cold pack at home.
Compression
- It is well known that compression increases blood circulation, which benefits your joints in several ways. Improved circulation reduces pain and inflammation and aids in joint healing.
- You may be able to utilize braces, tape, gloves, or compression stockings to help with your troublesome joints.
Elevation
- Locate a posture that raises your sore joint if you can. Inflammation and edema can be reduced by elevating your joints.
- This could entail lying down with your elbow or foot propped up on a pillow or sitting with your feet on a footstool. Additionally, your physical therapist may suggest elevation-based stretches or exercises.
Exercises
- To help you maintain your range of motion and reduce discomfort and stiffness, your physical therapist can demonstrate several exercises.
- Moderate range of motion exercises can promote fluid circulation during active flare-ups of pseudogout. Explore the whole range of motion in your affected joints by moving them as gently as possible.
- For days when your pseudogout is not bothering you, your physical therapist can also teach you strengthening exercises.
- Try low-impact exercises for your overall health and pain management, such as walking, cycling, or swimming.
Edema Control
- The swelling that results from having too much fluid in one area of your body is called edema.
- Wrapping your joints can help you manage swelling in its early stages. You can limit the amount of space available for fluids to accumulate by covering your joint.
- By pushing the fluid out of your joint, you can avoid the discomfort, stiffness, and decreased mobility that come with edema. If you have chronic pseudogout and have begun to notice the development of your symptoms, this is an excellent alternative.
- Wrapping your joint is best done before the edema has worsened. Before wrapping, consider applying cold and elevating your joint if it is already fairly swollen.
Joint drainage
An affected joint’s pressure and pain can be reduced by removing a portion of the joint fluid. The fluid is extracted with a needle. Additionally, the procedure aids in the removal of some of the joint’s crystals. After that, a corticosteroid and numbing drug are injected into the joint to reduce inflammation.
Home care
Gout episodes can be avoided and uric acid levels lowered with the use of several natural therapies.
The foods are:
- Tart cherries
- Magnesium
- Ginger
- Diluted apple cider vinegar
- Celery
- Nettle tea
- Dandelion
- Milk thistle seeds
However, these might not be sufficient on their own to treat gout. Some meals can aid in the fight against inflammation. Individuals can experiment with eating a lot of the following foods:
- Fruit: Citrus fruits, cherries, strawberries, and raspberries are all good choices.
- Salmon, herring, tuna, sardines, scallops, and anchovies are among the fish that people can sample.
- Nuts: Walnuts, pine nuts, almonds, and pistachios.
- Beans: Antioxidants are especially abundant in kidney and pinto beans.
- The recommended daily intake of olive oil is two to three teaspoons.
- Whole grains include things like oatmeal, brown rice, and quinoa.
- Red bell peppers, tomatoes, eggplant, and potatoes are examples of nightshade vegetables. It is best to keep an eye on symptoms when consuming these meals because some people think they cause flare-ups of arthritis.
Pseudogout flare-ups may benefit from home remedies. Among the examples are:
- NSAIDs. NSAIDs that are available over-the-counter, like naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, and others), are frequently beneficial.
- Give the joint some rest. For a few days, try not to use the affected joint.
- Ice. The inflammation linked to flare-ups can be lessened with the use of cold packs.
Foods to Avoid
Purines, which your body converts to uric acid, are found naturally in some meals.
Foods high in purines can be tolerated by most people. However, if your body has problems eliminating too much uric acid, you might want to stay away from the following foods and beverages:
- Red meats
- Organ meats
- Certain seafood
- Alcohol
Even if sugar-sweetened drinks and foods that contain fructose don’t include purines, they can still be harmful. Certain meals are beneficial for gout sufferers and help lower the body’s uric acid levels.
Complication
In addition to causing joint injury, the crystal deposits linked to pseudogout can also resemble the symptoms of rheumatoid arthritis or osteoarthritis.
Additionally, flare-ups are more frequent and severe in people with untreated pseudogout. Some persons with pseudogout have neck pain or headaches. This may occur if CPP deposits develop around your upper neck’s thick bone.
Prevention
Is it possible to avoid pseudogout?
As of right moment, pseudogout cannot be prevented. However, scientists are investigating the precise mechanism by which your body generates the excess CPP that results in it.
You can lessen the frequency of symptom flares by taking care of any additional medical conditions you may have.
Symptoms occur more frequently in certain people by nature than in others. If you have a pseudogout attack, it’s not your fault and you didn’t do anything unhealthy or incorrect. Usually, there are no obvious causes (triggers) that you can change or stay away from.
- Limit how much alcohol you drink.
- Limit your intake of foods high in purines, such as organ meat, beef, hog, lamb, and seafood.
- Eat a diet high in veggies and low in fat and dairy.
- Maintain a healthy weight.
- Avoid smoking.
- Exercise regularly.
- Stay hydrated.
Prognosis
You should anticipate intermittent flare-ups of your symptoms. If you don’t have pseudogout identified and treated by a medical professional, flare-ups may occur more frequently. Although CPPD cannot be cured, it can be managed with medication and changes in lifestyle.
The calcium pyrophosphate crystals, however, have the potential to worsen joint injury over time. In certain situations, this harm may lead to incapacity. Flares typically occur more frequently as people age, even if they are receiving treatment for pseudogout.
Pseudogout attacks often subside within ten days. Mobility issues and long-term joint damage might result from chronic CPP crystal arthritis. The severity will vary depending on the underlying ailment if CPPD is caused by another sickness.
What medical conditions may be associated with pseudogout?
Pseudogout can occasionally be linked to additional conditions like:
- The thyroid disorders hypothyroidism and hyperparathyroidism
- A genetic bleeding problem called hemophilia makes it difficult for blood to clot normally.
- A disorder called ochronosis results in the deposition of a dark pigment in the connective tissues, including cartilage.
- The accumulation of an aberrant protein in the tissues is known as amyloidosis.
- An unusually high blood iron level is known as hemochromatosis.
What makes gout different from pseudogout?
Pseudogout is named for its resemblance to gout, another form of arthritis that presents with comparable symptoms. Pseudogout is fake gout because pseudo is a prefix meaning false.
When there is an excess of uric acid in the blood (hyperuricemia), sharp crystals of uric acid form in your joints, causing inflammation and gout.
Pseudogout is caused by an accumulation of calcium pyrophosphate (CPP), a different mineral, in your joints. For this reason, calcium pyrophosphate deposition is another name for pseudogout. The act of putting anything is called deposition.
The joint where your big toe joins the rest of your foot is the most frequently affected by gout. Pseudogout is far more common in larger joints and rarely occurs in the MTP joint. Both gout and pseudogout are forms of arthritis that are caused by crystals building up in the joints.
Gout is caused by crystals of urea (uric acid), whereas pseudogout is caused by crystals of calcium pyrophosphate.
Are foods able to cause pseudogout?
Attacks of pseudogout are typically not caused by food or beverages. However, it may cause bouts of gout. That is one of the main distinctions between gout and pseudogout.
Gout flares can be caused by consuming alcohol or specific foods. When your body breaks down foods or beverages that contain compounds called purines, it may produce more uric acid. For this reason, a low-purine diet is frequently used to treat gout.
To maintain your general health or treat any diseases you may have, your healthcare professional may advise you to eat or refrain from particular foods. However, calcium pyrophosphate crystals do not accumulate in the body in the same manner as uric acid, hence pseudogout is typically unrelated to dietary factors.
FAQs
What circumstances lead to pseudogout?
Risk factors for pseudogout, such as hypermagnesemia.
Excessive parathyroidism.
Thyroid conditions.
Iron overload, or hemochromatosis.
Hypophosphatemia.
Osteopenia.
Chronic kidney disease (CKD).
What metabolic factors contribute to pseudogout?
Crystals of calcium pyrophosphate dihydrate have been connected to pseudogout in the affected joint. As people age, these crystals become increasingly common; over half of those over 85 have them. However, the majority of persons with these crystal deposits never get pseudogout.
What is the most effective way to cure pseudogout?
NSAIDs, or nonsteroidal anti-inflammatory medications. NSAIDs of prescription strength include indomethacin (Indocin) and naproxen (Naprosyn)… Colchicine (Colcrys, Mitigare). This gout medication, corticosteroids, works well for pseudogout when taken in small doses.
Where does pseudogout most frequently occur?
Podagra, which first appears in the joints in 50% of gout cases and finally becomes implicated in 90% of them, is also seen in individuals with pseudogout and other illnesses. Other sites of arthritis – The instep, ankle, wrist, finger joints, and knee are affected by gout; big joints (such as the knee, wrist, elbow, or ankle) are affected by pseudogout.
At what age does pseudogout often manifest?
One form of arthritis is calcium pyrophosphate deposition (CPPD), commonly referred to as “pseudogout.” Crystals of calcium pyrophosphate (CPP) accumulate in the blood and land in joint cartilage in CPPD. Although it may occur early in life, CPPD is more common in people over 60.
Which essential oil is best for arthritis?
In rats with induced arthritis, researchers discovered that turmeric essential oil prevented joint swelling 95–100% of the time. Additionally, they discovered that the essential oil was 68 percent successful in reducing acute inflammation when the turmeric was postponed until after it peaked.
How is pseudogout diagnosed?
By examining the synovial fluid in the joint cavity, doctors can make the diagnosis of pseudogout. Under a microscope, joint fluid is examined as part of the routine diagnostic procedure to check for the presence of CPPD crystals among inflammatory cells, or neutrophils. X-rays can be utilized for diagnostics as well.
How can one distinguish between pseudogout and gout?
You can have discomfort or episodes more frequently if you have persistent gout. Attacks by pseudogout are similarly abrupt. But the discomfort can last for days or weeks and normally doesn’t change. Some folks may have persistent pain or discomfort.
Reference
- Pseudogout – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/pseudogout/symptoms-causes/syc-20376983#:~:text=Pseudogout%20has%20been%20linked%20to,By%20Mayo%20Clinic%20Staff
- Pseudogout (Chondrocalcinosis or CPPD). (2024, September 10). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/pseudogout-chondrocalcinosis-cppd
- Pseudogout – Diagnosis and treatment – Mayo Clinic. (n.d.). https://www.mayoclinic.org/diseases-conditions/pseudogout/diagnosis-treatment/drc-20376988
- Pseudogout. (2022, February 15). ColumbiaDoctors. https://www.columbiadoctors.org/treatments-conditions/pseudogout#:~:text=What%20is%20pseudogout?,feet%20may%20also%20be%20involved.
- Kinman, T. (2023, March 8). Gout: Symptoms, causes, and treatments. Healthline. https://www.healthline.com/health/gout#takeaway
- Osborn, C. O. (2018, November 2). Essential oils for gout. Healthline. https://www.healthline.com/health/gout/essential-oils-for-gout
- Barrell, A. (2021, September 29). What is pseudogout, and how does it differ from gout? https://www.medicalnewstoday.com/articles/pseudogout#remedies
- Calcium pyrophosphate deposition. (2023, August 21). https://patient.info/bones-joints-muscles/calcium-pyrophosphate-deposition-pseudogout