Pott’s Spine Disease
What is Pott’s spine disease?
Pott’s spine, also known as spinal tuberculosis or tuberculous spondylitis, is a form of tuberculosis that affects the vertebrae of the spine. It occurs when Mycobacterium tuberculosis, the bacteria responsible for tuberculosis, spreads from the lungs to the bones of the spine. This condition often leads to the destruction of the vertebrae, causing pain, deformity, and neurological complications due to spinal cord compression.
Spinal TB, or Pott disease, is typically caused by the hematogenous spread of tuberculosis from other locations, most commonly the lungs. The typical extra-pulmonary form of tuberculosis (TB) is known as spine TB and is one of the oldest known diseases in human history.
In developing countries with dense populations, spinal tuberculosis (TB) has a greater morbidity and fatality rate than other illnesses.
The vertebrae most often affected by spinal TB are the lumbar and lower thoracic, followed by the cervical and middle thoracic vertebrae. According to reports, 3 to 5% of occurrences involve the second cervical to the seventh cervical region, and atlantoaxial articulation is less frequent. The most often affected region was the lamina, which was followed by the transverse, articular, spinous, and pedicle processes.
Through the intervertebral disc gap that separates two neighboring vertebrae, the infection may spread. The disc is normal if only one vertebra is impacted; however, if two vertebrae are impacted, the avascular disc collapses due to the inability to obtain nutrition. The disc tissue dies in a process known as caseous necrosis, which causes vertebral constriction, vertebral collapse, and eventual spinal injury. Often, a dry soft-tissue mass develops, and superinfection is not common.
An abscess is frequently caused by an infection that travels from the lumbar vertebrae to the psoas muscle. The disease has recently demonstrated an increasing incidence in industrialized countries, especially among immunocompromised individuals as a result of international migration and tourism. Over the past few decades, there has been a concerning increase in the prevalence of multidrug-resistant bacterial strains of tuberculosis in underdeveloped countries, posing a serious threat to the international community. As a result, the illness is still a serious worldwide public health threat today.
What are the causes of Pott’s spine disease?
- An infection can go to the spine from the lungs. Hematogenous spread refers to the spread that occurs through blood.
- When someone has an active tuberculosis infection, they can spit, sneeze, cough, talk, and other bodily fluids that release aerosol particles into the air. Up to 40,000 aerosol droplets can be released with each sneeze, and all it takes for TB to spread is one contaminated droplet.
- Prolonged contact with infected patients, immunodeficiencies like HIV, alcoholism, drug addiction, overcrowding, malnourishment, poverty, and a lower socioeconomic status are some of the established risk factors for tuberculosis.
- Mycobacterium TB typically causes spinal involvement when it hematogenous spreads into the thick vasculature of the cancellous bone of the vertebral bodies. Either a genitourinary tract infection or a lung lesion is the main site of infection.
- Either the venous or arterial pathways are used for spread. The anterior and posterior spinal arteries give rise to an arterial arcade that generates a rich vascular plexus in the subchondral region of each vertebra. The hematogenous dissemination of the illness to the paradisiacal regions is facilitated by this vascular plexus.
- A system without valves in the vertebra called Batson’s paravertebral venous plexus permits blood to flow freely in both directions based on the pressure created by the intrathoracic and intra-abdominal cavities during intense actions like coughing. Again, greater infection is disseminated to several vertebrae by the vertebral venous system in patients with noncontiguous vertebral tuberculosis.
- Initial symptoms of spinal TB are felt in the anterior inferior region of the vertebral body. After that, it extends into the disc or core region of the body. Central, anterior, and parietal injuries are the most common forms of vertebral involvement. The disc is unaffected in the core lesion, and vertebra plana are the result of the vertebral body collapsing. Complete compression of the vertebral body is indicated by vertebral plana.
- The disc is frequently included in younger individuals due to its increased vascularization. The disc is not particularly affected in old age since avascularity is seen at a higher age. Because its segmental arteries bifurcate to deliver blood to two adjacent vertebrae, spinal TB affects more than one vertebra.
- Multiple nearby vertebrae are involved in the disease’s spread beneath the anterior or posterior longitudinal ligaments. It is suggested that the reason for the subligamentous spread of infection in mycobacterial infections is a deficiency of proteolytic enzymes.
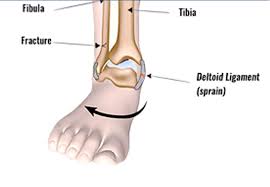
- The destruction of the intervertebral disc space and the surrounding vertebral bodies, the collapse of the spinal elements, and anterior wedging, which results in the formation of gibbous (a palpable deformity caused by the involvement of multiple vertebrae), are characteristic features of spinal tuberculosis.
- The most frequently affected regions are the lower thoracic and upper lumbar spines. Usually, more than one vertebra is impacted, with the vertebral body being impacted more frequently than the posterior arch.
- Because the disc is more vascularised in younger people, this is where the involvement primarily occurs. Due to its age-related avascularity, the disc is not particularly involved in old age.
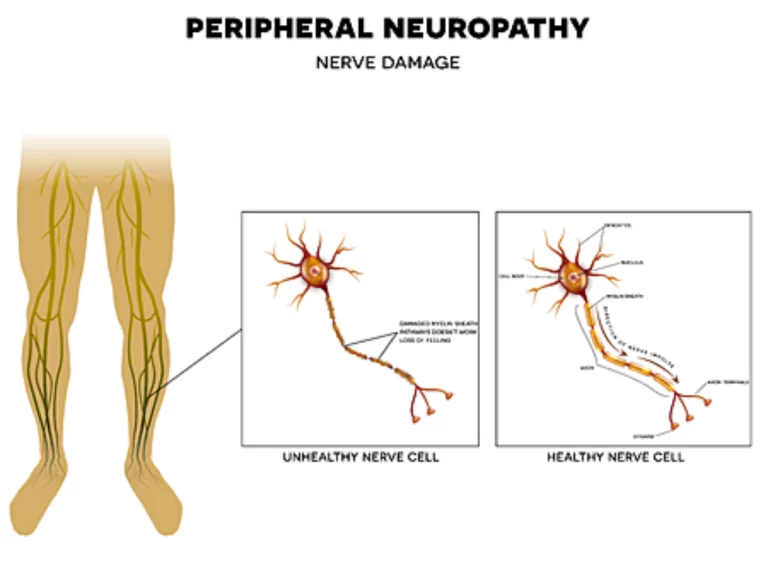
- In the active stage of spinal tuberculosis, early-onset paraplegia develops and requires intensive therapy. Adults with Pott’s spine are frequently affected by this kind of paraplegia, which has a better prognosis. Because the intervertebral disc and bone have been destroyed in each of these cases, paraplegia has resulted from the production of pus and debris-granulation tissue.
- Extensive tuberculous deterioration may result in concertina collapse, a compression fracture that does not affect the intervertebral disc.
- Meningomyelitis is caused by intrinsic causes that might directly affect the spinal cord, the area around the meninges and roots, or the blood vessels that supply the spinal cord.
- A neurological consequence known as “late-onset paraplegia” can develop in a patient who has recovered from tuberculosis after varying amounts of time. A late-onset paraplegia may appear two to three decades following an active infection. It frequently has a connection to noticeable spinal abnormalities.
What are the symptoms of Pott’s spine disease?
- A cold abscess, gibbous, a noticeable spinal deformity, and localized pain, tenderness, stiffness, and spasms of the muscles are among the characteristic clinical characteristics of spinal tuberculosis. When a tuberculous infection spreads to nearby ligaments and soft tissues, a cold abscess gradually develops.
- Spinal tuberculosis is a slowly developing, sneaky illness. The illness can last anywhere from a few months to many years in total, with an average disease length of four to eleven months. Patients typically only seek guidance when they are experiencing excruciating pain, a noticeable deformity, or neurological problems.
- Approximately 20–30% of cases of osteoarticular TB have constitutional symptoms. The basic constitutional signs of tuberculosis—malaise, hunger and weight loss, night sweats, evening fever, generalized body pains, and fatigue—signify the presence of active disease.
- POTS is characterized by a number of symptoms, such as headache, palpitations, tremors, nausea, weariness, blurred vision, difficulty thinking and concentrating (brain fog), intolerance to exercise, and lightheadedness (sometimes accompanied by fainting).
- The most common sign of spinal tuberculosis is back pain. The intensity of pain varies from a persistent, dull hurting to a severe, incapacitating pain. Pain is usually restricted to the site of involvement and is most frequently found in the thoracic cavity. The pain may be exacerbated by weight bearing, coughing, and spinal motion due to pathological fracture, progressive disc disintegration, and spinal instability. In half of the instances of spinal TB, the only sign was chronic back pain.
- When the cervical and thoracic areas are involved, neurologic impairments are common. Early neurologic involvement may develop into tetraplegia or total paraplegia if ignored. Any moment and at any stage of the spinal disease can result in paraplegia. The degree of neurological signs depends on the inclusion level of the spinal cord.
- Upper extremity function remains normal if the thoracic or lumbar spine is involved, but lower extremity problems worsen with time and eventually result in paraplegia. Due to damage to the lumbar and sacral vertebrae, patients with cauda equina compression experience pain, weakness, and numbness, but their affected muscle groups’ reflexes are either absent or severely reduced. This is in contrast to the cauda-equina syndrome, which is characterized by hyperreflexia caused by spinal cord compression and bladder involvement.
- A chilly abscess forming around the spinal lesion is another telltale indication of tuberculosis in the spine. The creation of abscesses is frequent and can get very large. The damaged region of the spinal column determines the size of a cold abscess. A retropharyngeal abscess is created in the cervical region when pus builds up posterior to the prevertebral fascia. The abscess may travel to the mediastinum and penetrate the esophagus, trachea, or pleural cavity. Significant pressure effects, such as dysphagia, hoarseness of voice, or respiratory pain, might result from a retropharyngeal abscess. The cold abscess typically manifests in the thoracic spine as a fusiform or bulbous paravertebral swelling, and it may also cause posterior mediastinal lumps.
- The most typical symptom of the cold abscesses formed at the lumbar vertebrae is swelling in the groin and thigh. On the medial aspect of the thigh, an abscess may form after descending beneath the inguinal ligament.
- One important aspect of spinal TB is spinal deformity. The location of the tuberculous vertebral lesion determines the kind of spinal deformity. The most frequent spinal deformity resulting from thoracic vertebral injuries is kyphosis. The number of affected vertebrae determines how severe the kyphosis is. Up to 20% of cases may still show a 10° or greater increase in kyphotic deformity following treatment. Torticollis deformity is a possible presentation of atlantoaxial TB.
Differential diagnosis of Pott’s spine disease?
- Pyogenic spondylitis, osteoporotic, metastasis, multiple myeloma, brucella spondylitis, and lymphoma are common differential diagnoses. Most cases of brucella spondylitis occur in middle-aged people. Usually included is the lumbar spine, which is followed by the cervical and thoracic spines. Although there is disc involvement and a limited amount of soft tissue in the paraspinal area, brucella spondylitis instances do not exhibit gibbous development.
- Any age can develop pyogenic spondylitis, which often affects the cervical and lumbar spines. There are visible signs of epidural abscesses, substantially increasing lesions, destruction of vertebral bodies, and intervertebral discs. The posterior elements are spared in pyogenic spondylitis, and gibbus deformity is typically absent. The sparing of the pedicles in osteoporosis often affects the thoracic vertebrae. In addition to the loss of several vertebral bodies, osteoporotic vertebrae typically exhibit reduced bone density.
- Most often, the thoracic region is affected by metastatic disease. Metastatic disease involves the lamina, pedicles, and posterior wall of the vertebral body; intervertebral disc heights are not affected. Multiple myeloma and lymphoma can also impact the intervertebral discs. It is always important to consider the possibility of metastatic spine disease in older people suffering from vertebral collapse.
Diagnosis of Pott’s spine disease?
The characteristic clinical appearance, systemic constitutional manifestation, evidence of prior TB exposure or concurrent visceral TB, and neuroimaging modalities are used to make the diagnosis of spinal tuberculosis.
Spinal tuberculosis is also diagnosed by skin examinations and hematological tests such as polymerase chain reaction (PCR), erythrocyte sedimentation rate (ESR), enzyme-linked immunosorbent assay (ELISA), complete blood count (CBC), and Montoux test. Samples of bone tissue or abscesses are obtained in order to stain for acid-fast bacilli (AFB) and isolate organisms for culture, antibiotic sensitivity, and histology; CT-guided or ultrasonography-guided needle biopsy & aspiration or surgical biopsy.
Plain radiographs
When a patient has spinal TB, plain radiographs are typically the first examination performed. Bone mineral loss is required for radiolucent abrasions to show up on a plain radiograph.
Either atrophy or protrusion into the disc tissue’s vertebral body causes the disc space to narrow. A varied degree of kyphosis results from anterior wedging or collapse with continued advancement. A paravertebral abscess forms in the anterior type of lesion due to the accumulation of necrotic material and tuberculous granulation tissue. The bird’s nest appearance is a fusiform or globular radiodense shadow seen in the thoracic spine region on plain radiographs.
In the dorsal spine of children, the anterior form is far more common. The central form of abrasions manifests as concentric collapse, vertebral body inflation, and disintegration. The posterior arches the spinous process, pedicle, lamina, and transverse process as well as the atlas’s lateral masses, erosion of the ribs next to it in the thoracic region, pedicular or laminar destruction, or the posterior cortex of the vertebral body with relatively sparse intervertebral discs and a sizable paraspinal mass—are all included in the appendiceal or neural arch type of lesion.
Computed tomography
Compared to a plain radiograph, computed tomographic scanning provides better bony detail for irregular lytic lesions, disc collapse, sclerosis, and disruption of bone circumference. However, CT is not as good at illustrating how the disease affects neural structures and how it extends epidurally.
On a CT scan, the pattern of bone loss may clearly be seen as fragmented, osteolytic, sclerotic, and subperiosteal. It works great for directing a percutaneous diagnostic needle in areas that are somewhat inaccessible or potentially harmful. Practically speaking, the presence of calcification within the abscess indicates spinal tuberculosis. One of the methods used to evaluate cord compression in cases of spinal tuberculosis (TB) was CT myelography, however, it has since been replaced.
Magnetic resonance imaging (MRI)
A gadolinium contrast agent is injected intravenously, and then non-contrast T1-weighted (T1W), T2-weighted (T2W), and short tau inversion recovery (STIR) sequences are performed in the axial, sagittal, and coronal planes. Following this, contrast-enhanced T1W sequences are performed. Abnormal signal intensities exhibiting hypointense on T1W and hyperintense on T2W sequences with the heterogeneous augmentation of the vertebral body are characteristics of Pott’s spine on MRI.
When separating fluid from fatty components in non-contrast sequences, STIR sequences come in handy. Prevertebral, paravertebral, and epidural abscesses were among the characteristic findings, along with the destruction of two neighboring vertebral bodies and opposing end plates, the intervening disc’s disintegration, vertebral body edema, and other conditions. MRI has a significant role in the high specificity and sensitivity diagnosis of spinal tuberculosis.
MRI is superior to most other imaging modalities in that it can directly image in several planes and provides strong contrast resolution for soft tissues and bone. Granulation tissue and a cold abscess may be distinguished with great accuracy on magnetic resonance imaging (MRI) with the use of intravenous magnetic resonance contrast agents.
Compared to ordinary films, an MRI can reveal more extensive involvement. For patients with suspected TB spondylitis, MRI offered more precise anatomic localization of vertebral and paravertebral abscesses in various planes, which was not previously possible with more traditional diagnostic modalities. When CT results were uncertain, MRI provided a clear picture of the soft tissue disease’s extent and how it affected the cord, theca, and the foramen. For diagnosis, CT and MRI are both very useful, and tissue aspiration is a useful confirming procedure.
By demonstrating disc enhancement, gadolinium with diethylene triamine pentaacetic acid (Gd-DTPA) administration is used to measure the amount of soft tissue mass and distinguish postoperative spondylitis from a typical postoperative course. Disc enlargement is rare throughout the typical postoperative recovery period. It should be diagnosed as postoperative spondylitis if it is connected to nearby spinal bone marrow abnormalities.
It can be challenging to differentiate between pyogenic, tuberculous, fungal, and postoperative spondylitis, even if the pattern of improvement in TB spondylitis differs from that of other spondylitis cases. When attempting to differentiate between pyogenic and tubercular spondylitis, magnetic resonance imaging (MRI) is a highly helpful tool.
The most typical effects were cord compressions and kyphosis. If early decompression is carried out urgently at the outset of the disease, the neurological inclusion is comparatively benign. A neurological condition known as late-onset paraplegia can develop in patients who have recovered from TB of the spine after a varied amount of time. When detecting rare and challenging disease locations, such as the craniovertebral junction, MRI is incredibly helpful.
Few cases of sacroiliac joint tuberculosis (TB) have been reported, and it is even more uncommon for TB to coexist with spinal TB. The best imaging technology for identifying sacroiliitis in its early stages is magnetic resonance imaging (MRI). If diagnosis and treatment are postponed, sacroiliac joint TB may progress to later stages with substantial joint damage and periarticular abscesses. Early detection of sacroiliac joint pathology may be possible with the standard MRI screening of individuals under study for lumbar disc disease, which now includes a coronal STIR T2-weighted sequence.
Cytological and microbiological confirmation
For the early histological identification of spinal TB, the gold standard method is to use neuroimaging guided-needle biopsy from the affected area. Usually, enough material is obtained from a nearby abscess or the spine itself during a CT-guided needle biopsy. When further treatments, including decompression and maybe arthrodesis, are planned or when closed approaches have proven ineffective, an open spine biopsy is typically carried out.
In India, spinal TB was successfully diagnosed by fine needle aspiration biopsy performed under CT guidance. In order to determine the etiological diagnosis, surgery might be necessary. It is necessary to send biopsy material for cytologic, histologic, and bacteriologic investigations. Up to half of cases may show smear positivity for acid-fast bacilli, whereas most cases will show culture positivity. However, due to the difficulty in detecting mycobacterial bacilli from extrapulmonary locations, culture is not the gold standard for diagnosing spinal tuberculosis, just like it is for respiratory tuberculosis.
About 60% of individuals have their diagnosis of spinal TB confirmed by histologic testing. The most often seen cytological abnormalities are lymphocytic infiltration, granular necrotic background, and epithelioid cell granulomas. In as many as half of the cases, scattered multinucleated and Langhans’ large cells may be observed. Since false-negative biopsy results are frequent, the diagnosis of spinal tuberculosis must be based on radiological findings and clinical signs in the event that bacteriology returns negative data.
Polymerase chain reaction and other immunological tests
Traditional microbiological techniques, such as cultivating Mycobacterium tuberculosis on Lowenstein Jensen media and using Ziehl-Neelsen staining for acid-fast bacilli, have poor sensitivity and specificity. It also takes a while to cultivate Mycobacterium tuberculosis; it takes 7-8 weeks for the growth to show up. Thus, the primary basis for diagnosing tuberculosis is histological evidence.
The polymerase chain reaction has demonstrated extremely encouraging outcomes for the quick and early detection of the disease. As low as 10–50 tubercle bacilli can be found with this approach in a variety of clinical samples. Compared to smears, this test is more accurate and can be completed more quickly than cultures.
By quantifying interferon-gamma extracted in plasma from whole blood incubated with the Mycobacterium tuberculosis-specific antigens, the QuantiFERON-TB Gold test detects cell-mediated inflammatory responses in vitro to tuberculosis infection.
A positive smear or culture, a biopsy that confirmed the disease, or a positive response to antituberculosis treatment were used to classify the patients as having tuberculosis. A small number of individuals had a vertebral collapse that could not have been caused by anything other than tuberculosis. The examination yielded an estimated 84% sensitivity and 95% specificity.
Other tests
The majority of individuals with spinal TB typically have elevated erythrocyte sedimentation rates (ESRs) by several orders of magnitude. Following control of the active tuberculous lesion, the ESR returns to normal or nearly normal.
Leucocytosis and raised ESR are correlated in pyogenic infections, but patients with spinal tuberculosis exhibit significantly elevated ESR along with normal WBC.
Treatment of Pott’s Spine Disease?
Medical treatment for Pott’s spine disease:
Early antitubercular treatment should be started in patients with spinal tuberculosis. It is often necessary to start antituberculous treatment empirically, long before an etiological diagnosis is made. Etiological diagnosis may not be made at all in developing nations. Surgery might also be required for patients with spinal TB problems that have been identified.
The majority of antituberculous medications are highly permeable to tuberculous spinal abrasions. In severe spinal tuberculosis vertebral tissues, the distribution of antituberculosis medications such as rifampin, isoniazid, and pyrazinamide was assessed. Isoniazid concentrations in tuberculous foci were bactericidal in patients without vertebral sclerotic walls surrounding the foci.
The minimal inhibitory concentrations of pyrazinamide and rifampin in foci matched each drug’s level. In a different investigation, three medications produced an effective bactericidal concentration level in the osseous tissues around the spinal tuberculosis foci, with the exception of the 4 mm of osseous tissue that encircles the sclerotic wall. The findings suggested that during the procedure, osseous tissues within 4 mm of the sclerotic wall should be removed.
Antituberculous medication:
- The majority of patients (82–95%) with spinal TB respond extremely effectively to medical treatment, according to several studies. Pain relief, a reduction in neurological deficiency, and even the correction of spinal deformity are all clear results of the treatment.
- Individuals with craniovertebral junction TB, which has the potential to be dangerous, also respond well to medical intervention. Prior to scheduling surgery, patients with medically resistant spinal TB require a thorough reevaluation of their differential diagnosis.
Therapeutic regimen:
- According to the WHO treatment classification, spinal TB is classified as category 1. There are two phases to the category-1 antituberculosis therapy regimen: an intensive or initial phase and a continuing phase. Four first-line medications are used in conjunction during the 2-month intense phase of antituberculous therapy: isoniazid, rifampicin, streptomycin, and pyrazinamide. Isoniazid and rifampicin are the two medications permitted for four months during the continuation phase.
- The World Health Organisation recommends nine months of treatment for tuberculosis of the bones or joints due to the significant risk of disability and mortality as well as the challenges in determining treatment response.
- Regardless of age, the British Thoracic Society recommends a 6-month course of daily treatment consisting of rifampicin and isoniazid, augmented in the first two months by pyrazinamide and either ethambutol or streptomycin.
- Even if six months of treatment is seen to be adequate, many specialists still advocate for a 12- to 24-month duration, or until pathological or radiological evidence of disease regression is obtained. Short-term regimens and directly observed treatment may be used to ignore low compliance. With the exception of cases of spinal arachnoiditis or spinal TB, corticosteroids have no clear role in spinal tuberculosis.
Supportive measures:
- Prior to the antituberculous chemotherapy phase, a patient with tuberculosis of the spine was treated with a combination of common supportive treatments, extended recumbency, and rest. Treatment for people with pulmonary and bone TB used to be provided at sanitariums.
- Immobilization using a cast or brace was a traditional treatment method, however, it was eventually proven to be ineffective and was typically dropped.
Surgical Treatment for pott’s spine disease:
- However, a number of specialists believe that not all instances of spinal TB need to be operated on, nor do all cases need to be treated conservatively.
- A larger percentage of bony fusion, quicker bony fusion, less kyphosis, quicker pain relief, an earlier return to prior activities, and less bone loss were among the potential advantages of surgery. It also relieved compressed neural tissue more quickly. If fusion has not taken place, it may also avoid neurological issues that arise later on as a result of spinal kyphosis. According to one expert, pan-vertebral lesions, extensive kyphosis, resistant disease, an increasing neurological deficiency, and clinical worsening or lack of clinical progress should all be considered criteria for surgery.
- There are two kinds of surgical operations carried out. Debridement with spinal stabilization is the alternative procedure. This is a more involved procedure where bone grafts are used to perform the reconstructions. Artificial materials such as titanium, steel, or carbon fiber can also be used for stabilization.
- Excellent outcomes were obtained from the combination of medical and surgical care. Following a three-level posterior vertebral column resection and significant posterior decompression/instrumented fusion, anterior debridement/fusion with cage reconstruction is the surgical course of treatment.
- Early detection and prompt, wise surgical intervention are essential to successful management; the choice of which must be made in light of the patient’s age, the degree of antitubercular therapy (ATT) response, and clinical-radiological compression of the spinal cord and nerve roots.
Physical therapy Treatment for Pott’s spine disease:
The goal of treatment is to cure the illness and to avoid, identify, and treat any complications, such as paraplegia, as soon as possible.
Indications for Taylor’s brace spinal orthosis:

could be applied to reduce pain and stop cervical spine deformities:
- Taylor’s brace,
- collar,
- Minerva jacket
Spinal fusion or decompression procedures are often performed on patients with Pott’s disease in order to repair the structural deformity and stop additional neurological problems. There are no set standards that specify the kinds of treatments that will work for these people. However, therapy plans should be tailored to each patient specifically, taking into account any disabilities, functional restrictions, or impairments they may have at presentation.
Following spinal decompression surgery, PT management
- Exercises for Spinal Stabilisation:
- Exercise and Strengthening for Back-to-School
In comparison to alternative physical therapy interventions and self-care, spinal stabilization exercises yielded noticeably higher ratings in overall outcomes. However, in contrast to the other two treatment options, pain and impairment did not significantly improve.
PT Management Following Spinal Fusion Surgery
- Aquatic Therapy
- TENS (Transcutaneous Electrical Neuromuscular Stimulation)
- Training Above Ground (Walking Program)
- Aerobic Exercise
- Strengthening the Trunk
Research on the application of TENS has demonstrated that neuropathic pain can be reduced more effectively at higher frequencies. Pain, psychological distress, and impairment have all been shown to significantly diminish with aerobic exercise, physical therapy, and trunk strengthening therapies.
How to prevent Pott’s spine disease?
Individuals who do not currently have active tuberculosis but have a positive PPD test may reduce their risk by appropriately using antitubercular medications. In order to effectively cure tuberculosis, patients need to take their drugs as directed.
What is the prognosis of Pott’s spine disease?
- collapse of the vertebrae resulting in kyphosis
- compression of the spinal cord
- Sinus formation
- (Pott’s paraplegia) paraplegia
For patients without neurological impairments or abnormalities, the prognosis is usually favorable. Numerous studies demonstrate that 80% of cases improve with medical treatment alone, resulting in pain relief, neurological deficiency improvement, and spinal deformity correction.
In a newly published study, 92% of patients with neurologic abnormalities showed considerable improvement, and 74% of them went from being nonambulatory to being ambulatory. The majority of patients in research conducted in an endemic nation exhibited severe motor and sensory impairment. Although antituberculous medication was used to handle all patients, some also needed surgical intervention.
FAQs
Is it improper to walk in spinal TB?
In the event that the back pain gets worse, the patient may have numbness, stiffness, or weakness in their legs, making it difficult for them to walk or stand. Back pain is another indication of tuberculosis in the spine.
How long does Pott’s spine therapy last?
Traditional courses last anywhere from nine months to more than a year, but some studies recommend a six- to nine-month duration. The length of therapy should be customized and determined by the patient’s clinical stability and the remission of active symptoms.
How is Potts being treated?
Rifampin and isoniazid should be given for the duration of the therapy. A second round of medication is given during the first two months of treatment.
Does age affect the POTS spine?
The good news is that, although POTS tuberculosis is a chronic condition, about 80 % of teens grow out of it after they reach the end of their teenage years when the bodily changes of puberty are over. POTS TB symptoms typically go gone by the time a person turns 20.
What is the life expectancy of POTS disease?
There is no evidence of a shortened life expectancy and POTS tuberculosis is not a life-threatening condition.
Is the POTS spine regarded as a handicap?
If a patient fits both a Blue Book listing and the Social Security Administration’s (SSA) definition of disability, their POTS may be classified as a disability. You may be eligible for disability compensation if your POTS does.
References
- Mehta, Y. (2022, November 21). Pott’s spine – Cause, Symptoms, Diagnosis, Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/potts-spine/




One Comment