Peripheral Artery Diseases (PAD)
Peripheral artery disease is characterized by a narrowing of the vessels that transport blood from the heart to different areas of the body. The most prevalent kind, The condition known as peripheral artery disease is characterized by a narrowing of the vessels that transport blood from the heart to different areas of the body.
The most prevalent kind, known as lower-extremity PAD, causes the legs and feet to receive less blood supply. Just 10% of people have upper-extremity PAD, which affects the arms, hands, and fingers.
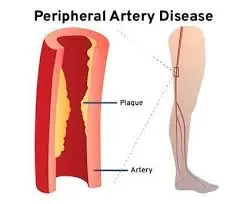
Atherosclerosis causes coronary artery disease and PAD. When fatty plaque accumulates in the arteries, it causes atherosclerosis, which narrows or stops the arteries in the heart, brain, arms, legs, pelvis, kidneys, and other organs.
Introduction
Peripheral artery disease (fats and cholesterol) builds up in the blood vessels in your arms or legs, causing peripheral arterial disease. As a result, your blood has a harder time delivering nutrients and oxygen to the structures in those places. Although PAD is a chronic condition, it can be improved by exercise, a lower-fat diet, and quitting smoking.
Narrowed arteries in peripheral arterial disease (PAD) cause less blood to flow to the arms and legs. Another name for this ailment is peripheral arterial disease.
The legs or arms, generally the legs, do not receive adequate blood flow to meet demand in PAD. Claudication, or leg discomfort when walking, is one symptom that may result from this.
Atherosclerosis, an accumulation of fatty tissue in the arterial walls, is typically indicated by peripheral arterial disease. Exercise, a good diet, and abstinence from tobacco use and smoking are all part of the treatment for PAD.
What is the illness of the peripheral arteries?
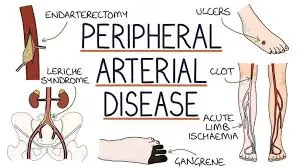
Plaque accumulation in the arteries of your legs is known as peripheral arterial disease (PAD). Your leg arteries transport blood that is rich in oxygen and nutrients from your heart to your arms and legs. This is also known as peripheral arterial disease.
Shaped like hollow tubes, capillaries have a smooth covering that prevents arterial from clotting and facilitates continuous blood flow. Plaque, which is composed of fat, cholesterol, and other chemicals, progressively accumulates inside the walls of your arteries when you’ve developed peripheral arterial disease. This narrows your arteries gradually. This is additionally recognized as peripheral arterial disease.
A lot of plaque deposits have soft interiors and rigid exteriors. Platelets, which are disc-shaped molecules in your blood that aid in clotting, might enter the area when the hard surface cracks or tears. Your artery may get even smaller as a result of blood clots that develop around the plaque.
Blood cannot flow through arteries to support organs and other tissues if plaque or a clot of blood narrows or stops them. This damages the tissues beneath the obstruction and ultimately results in gangrene, which is death. The soles of your feet are where this occurs most frequently.
PAD can get worse faster for some persons than for others. Numerous additional elements are important, such as your general health and the location of the plaque in your body.
The study of epidemiology
More than 200 million adults globally suffer from PAD, and in those over 70, the prevalence might reach 20%. The prevalence of PAD seems to be the same among older men and women, even though it has historically been thought of as a disease that affects males. Since the majority of PAD patients do not exhibit the stereotypical claudication symptoms outlined in textbooks, underdiagnosis of the condition in the primary care context may be a serious problem.
Smoking has the most effect on the severity of PAD and quadruples the risk of getting it. Smokers with PAD have shorter lives and are more likely to get critical limb ischemia and amputation than non-smokers. Race, ethnicity, diabetes, hyperlipidemia, and hypertension are additional risk factors for PAD.
Pathophysiology
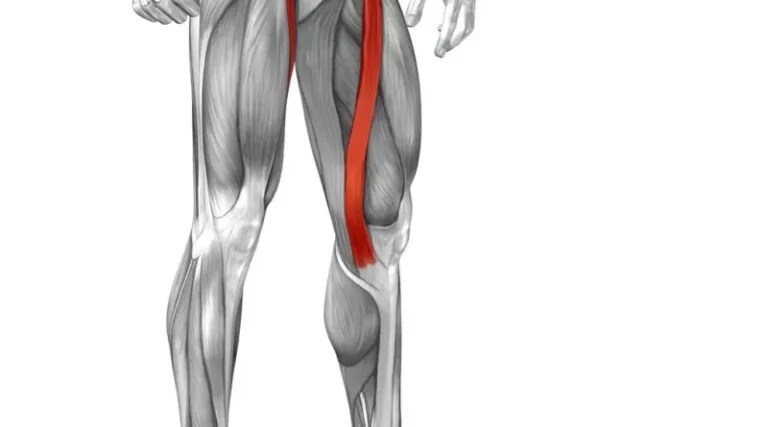
The iliac, femoral, and abdominal aortic arteries are typically affected by atherosclerotic disease in PAD. Details of the intricate relationships between cholesterol and vascular cells that underlie the pathophysiology of atherosclerosis. On the inner of arteries, atherosclerotic plaque gradually accumulates. The arteries dilate to maintain vascular flow in the early stages of PAD to make up for the plaque accumulation. Atherosclerotic plaque begins to constrict the arterial flow channel when the artery can no longer dilate.
Occasionally, atherosclerotic disease of the aorta or emboli of cardiac origin may be the cause of abrupt ischemia. Where arterial bifurcation occurs or where artery branches abruptly take off, emboli are typically most prevalent. The most frequent location for emboli is the femoral artery, which is followed by the iliac, aortic, and popliteal arteries.
The extent of arterial constriction determines the hemodynamic effects of atherosclerosis. A 75% reduction of cross-sectional area, which is typically regarded as flow limiting, results from a 50% decrease in vessel diameter. Blood flow changes to smaller arteries that run parallel to the sick artery as the constriction worsens or blocks the artery entirely. The system of smaller vessels never provides as much blood circulation as the major artery, even if this collateral flow maintains distant perfusion.
The defining characteristic of PAD and its common symptoms is this restriction of blood flow. To fulfill the increased energy requirement during ambulation, the lower extremity muscles need more blood flow. When walking, patients with PAD reach a point where collateral blood flow reaches its maximum and the lower extremity muscles are no longer able to get any further perfusion.
The patient with PAD eventually slows down or stops walking as a result of this supply-demand imbalance, which results in transient muscular ischemia that produces discomfort, cramping, or exhaustion. The ischemia symptoms go away when the blood supply catches up with the muscle’s decreased energy needs, which can be achieved by slowing or stopping the muscle.
The pathophysiology of claudication caused by PAD is described by brief muscular ischemia, and this cycle of blood flow limitation raises energy demand.
Patients with PAD typically have adequate collateral blood flow, so their symptoms only appear when they walk or engage in other activities that raise their energy demands. In rare instances, the PAD worsens over time, and the blood flow is unable to keep up with the lower extremities’ resting metabolic needs.
Ischemic rest pain, which is frequently defined as an unbearable, scorching agony in the soles of the feet, can be caused by inadequate perfusion to the nerves. Ischemic ulcers and non-healing wounds are examples of tissue loss caused by insufficient blood flow. In the worst situations, gangrene can develop and cause the toes or entire forefoot to turn black and mummified.
Causes
Atherosclerosis, a disorder in which lipids, cholesterol, and other chemicals accumulate in and on the artery walls, is frequently the cause of peripheral artery disease (PAD). We refer to the accumulation as plaque. Plaque can cause arteries to narrow, preventing blood flow. Plaque builds up in the arterial systems of the lower extremities in PAD.
Peripheral arterial disease is caused by atherosclerosis that forms in the arteries of your legs or, less frequently, your arms. Peripheral vascular disease is caused by a buildup of fatty plaque in the walls of your blood vessels, similar to atherosclerosis in the coronary arteries of your heart. Your blood vessels become increasingly constricted as plaque accumulates, eventually being blocked.
Symptoms
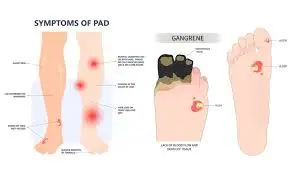
Peripheral artery disease (PAD) may not cause symptoms, or symptoms may be minimal.
Symptoms of PAD include:
- Intermittent claudication, or pain, cramping, or discomfort in the legs or buttocks, is typically the initial sign of PAD. When you’re active, this occurs, and when you’re sleeping, it disappears.
- Walking-related leg pain.
- Arm or leg muscle soreness or cramping, usually in the calf.
- Arm or leg muscle soreness that starts with exercise and goes away with rest.
- After walking, climbing stairs, or engaging in other activities, one or both hips, thighs, or calves may experience painful cramping.
- Arm pain, including cramping and aching when writing or knitting.
Peripheral vascular disease affects half of its patients with no symptoms. Lifetime accumulation of PAD is possible. The symptoms might not show up till later in life. Symptoms won’t show up for many people until their artery narrows by 60% or more.
To begin therapy as soon as feasible, discuss your PAD symptoms with your healthcare physician. It is crucial to discover PAD early to start the appropriate treatments before the condition worsens to the point where consequences like a heart attack or stroke occur.
The symptoms of peripheral artery disease include:
Mild to severe muscle pain that wakes you up, makes it difficult to walk or exercise, occurs during rest or when you lie down if the condition is severe, and manifests as coldness in the lower part of the leg or foot, particularly when compared to the other side.
Other symptoms of PAD may include:
- Shiny skin on the legs.
- Skin color changes on the legs.
- Slow-growing toenails.
- Sores on the toes, feet, or legs that won’t heal.
- Reduced or slowed growth of leg hair.
- Erectile dysfunction.
- A burning or hurting sensation in your toes and feet when you’re sleeping, especially when you’re lying flat at night.
- Your feet’s skin is cool.
- Your skin’s redness or other color changes.
- Increased incidence of soft tissue and skin infections, typically in the legs or feet.
- Unhealing foot and toe sores.
Risk elements
80% of people with PAD smoke or have smoked in the past, making tobacco use the most significant risk factor for PAD and its complications. Smoking increases the risk of developing PAD by 400% and causes symptoms to appear nearly ten years earlier than in nonsmokers of the same age.
Peripheral artery disease (PAD) risk factors include:
- The presence of peripheral artery disease, heart disease, or stroke in the family.
- Diabetes.
- High blood pressure.
- High cholesterol
- Growing older, particularly after the age of 65 or after the age of 50 if you have atherosclerosis risk factors.
- Being overweight.
- Smoking.
Despite being distinct conditions, coronary artery disease and PAD are connected. Those who possess one are probably also in possession of the other. Peripheral artery disease (PAD) increases the risk of heart attacks, strokes, coronary artery disease, and transient ischemic attacks (mini-strokes). The likelihood of peripheral artery disease in the legs is one in three for a person with heart disease.
Not surprisingly, several risk factors are similar to both diseases. The reason for this is that the arteries in your arms and legs undergo the identical alterations as the arteries in your heart due to these risk factors.
Complication
Atherosclerosis-induced coronary artery disease (PAD) complications include:
- Severe ischemia of the limbs. Tissue death results from an injury or infection in this syndrome. Gross wounds on the hands and feet that don’t heal are one of the symptoms. Amputation of the afflicted limb may be part of the treatment.
- Heart attack and stroke. The heart and brain’s blood vessels may also be impacted by plaque accumulation in the arteries.
If left untreated, PAD patients may require amputation, which involves removing all or a portion of the foot, leg, or sometimes, the arm. This is particularly true for those who also have diabetes.
The consequences of PAD can go beyond the afflicted limb because of the interdependence of your body’s vascular system. Individuals who have atherosclerosis in their legs frequently also have it in other body areas.
What physical effects does my peripheral artery disease have on me?
Claudication, a word in medicine for leg pain that begins with walking or exercise and subsides with rest, is the most common symptom of PAD. Your leg muscles aren’t receiving enough oxygen, which causes agony.
The dangers of PAD extend well beyond difficulties walking. A nonhealing pain on either the feet or legs is more likely to occur if you have peripheral vascular disease. These sores may develop into gangrene, or patches of dead tissue, in situations with severe PAD, necessitating the removal of your foot or limb.
What phases does peripheral artery disease go through?
Healthcare professionals can assign a stage to your PAD using either the Fontaine or Rutherford systems.
The simpler Fontaine phases are as follows:
- I: Symptomless (asymptomatic).
- IIa: Leg pain with exercise, or mild claudication.
- IIb: Claudication ranging from moderate to severe.
- III: Ischemic rest pain, or leg discomfort that occurs while you’re at rest.
- IV: Gangrene or ulcers.
Avoidance
Maintaining a healthy lifestyle is the best defense against peripheral artery disease (PAD)-related leg pain. This implies:
- Avoid smoking.
- Consume foods that have a content low in saturated fats, trans fats, and sugar.
- Engage in regular exercise, but with your care provider to determine the optimum kind and quantity for you.
- Maintain a healthy weight.
- Control your diabetes, cholesterol, and blood pressure.
- Get enough rest.
- Control stress.
Evaluation and Diagnosis
How may peripheral artery disease be identified?
Usually, a physical examination, a review of your medical information, and one or more diagnostic procedures are required to diagnose PAD.
Your physician will inquire about your symptoms and any known risk factors for PAD, including a history of cardiovascular disease, Hypertension, diabetes, and smoking. During a physical examination, your doctor will look for lesions or ulcers on your feet, check for weak circulation in the muscles of your arms and legs, and check your skin for symptoms of PAD.
Along with a physical examination, a provider will go over your risk factors and medical history. Noninvasive tests might be prescribed to assist diagnose and assess the severity of PAD. The following tests can assist in determining whether you have a blood vascular blockage:
Ankle-brachial index (ABI).
Lower extremity PAD is diagnosed by ABI. You lie flat on your back with your arms and legs at the same level as your heart for this non-invasive test. After that, a Doppler ultrasonography probe is used to listen to the arterial pulse and measure the blood pressure in the arms and ankles.
The arterial pressure ratio in the ankle relative to the arm or brachial artery is the basis for the ABI for the right and left sides of the body. An ABI of 0.9 to 1.4 is regarded as normal; if the ABI is less than 0.9, lower extremity PAD is diagnosed.
Doppler pressure testing in segments.
To stabilize your blood pressure, you lie flat on an exam table for fifteen minutes throughout this test, which is usually performed with an ABI. After that, three or four blood pressure cuffs are placed at various locations on your arm or leg.
The doctor checks each cuff’s blood pressure using Doppler ultrasonography. Your doctor may be able to determine the location of the restricted or blocked artery if there is a significant enough variation in blood pressure at various arm or leg levels.
- Practice ABI. If your resting ABI is normal but you have claudication, your doctor may order this test. You will walk on a treadmill before undergoing an ABI test for this test. It is employed to identify PAD in the lower extremities.
- Duplex arterial. This test can identify the regions that are significantly narrowed by measuring the flow velocity inside the arteries using an ultrasound probe. Additionally, it may see the calcium and plaque in the vessel walls. It is usually done in an office setting and is non-invasive.
Additional imaging tests, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, are usually accompanied by an intravenous contrast agent injection to improve artery visualization. These examinations give precise information about the arteries’ whole structure, including where diseased sections are located. They are usually saved for intervention planning, surgery, or certain situations where more anatomical data is required than what an ultrasound can offer.
An invasive test known as an angiography could also be required to identify arterial blockages.
Distinctive Diagnosis
- Deep vein Thrombosis
- Low back pain
- Transient thrombophlebitis
- The Raynaud phenomenon
- Trombonists Obliterans
- Sciatica
Management and Treatment
If you believe you may already have peripheral artery disease (PAD) or are at risk for developing it, consult your primary care physician, vascular medicine specialist, or cardiologist to begin a prevention or treatment program immediately. Research has indicated that exercise in blood pressure and cholesterol control can reverse the symptoms of peripheral vascular disease.
The patient’s symptoms determine how peripheral artery disease is treated. However, a diagnosis of PAD carries a considerable risk of disease and mortality regardless of symptoms. Therefore, the optimal medical therapy for each patient with PAD should be started right away.
How is peripheral artery disease treated?
PAD can be treated with procedures, drugs, and lifestyle modifications.
Treatments for peripheral artery disease have two primary objectives:
- Reducing your risk of cardiovascular events.
- Reducing the discomfort that comes with walking and enhancing your quality of life.
Lifestyle changes
Rehabilitation of PAD starts with implementing lifestyle modifications to minimize your risk factors.
The following adjustments can help you manage your condition:
- Stop using tobacco products. Inquire with your doctor about programs for quitting smoking.
- Consume a diet rich in fiber while being low in fat, cholesterol, and sodium to maintain a healthy balance.
- Keep fat to no more than 30% of your daily caloric intake.
- No more than 7% of your calories should come from saturated fat.
- Avoid items that include partially hydrogenated and fermented vegetable oils, as well as trans fats.
- Get moving. Begin a regular fitness regimen, like going on walks.
- One way to treat PAD is to walk. Regular walkers can enhance the distance they can cover before experiencing leg pain.
- Control other medical disorders, such as diabetes, high blood pressure, or high cholesterol; maintain a low-stress level; yoga, meditation, and exercise may assist; and take proper care of your feet and skin to avoid infection and lower the chance of consequences.
Drugs
You can use pharmaceuticals to treat problems including diabetes, high blood pressure (antihypertensive drugs), and high cholesterol (statin drugs). These medications lower your risk of heart attack and stroke while treating the risk factors for PAD.
An antiplatelet drug like clopidogrel or aspirin may be prescribed by your doctor. To increase your walking distance, they might also recommend cilostazol. People with intermittent claudication can exercise for longer periods before experiencing leg pain thanks to this medicine.
Antiplatelet medications, lessen the chance of blood clots and, thus, the risk of heart attack and stroke. These drugs, like clopidogrel or aspirin, may lessen the symptoms of PAD and improve walking distance for those with lower extremity PAD.
Statins can help lessen the risk of cardiovascular disease, lower cholesterol, halt the advancement of atherosclerosis, and lower the risk of PAD complications.
Regardless of cholesterol, statins are advised for people with PAD. Cilostazol is a vasodilator that can help persons with lower extremity PAD walk farther and lessen claudication pain.
A groin puncture is usually used for endovascular interventions, which are minimally invasive treatments. To improve blood flow to the limb, wires, catheters, and other specialized devices can be introduced to the narrowing area and utilized to open the blockage under the supervision of X-rays and sophisticated imaging.
The following endovascular methods are used to treat PAD:
- Angioplasty. A medical professional guides a catheter with a balloon attached to its tip to the constricted or obstructed section of the artery. The balloon is then inflated, forcing the artery to open and blood flow to resume. Occasionally, a medication that helps stop blood vessel re-narrowing is applied to the balloon. The balloon and catheter are taken out after the treatment.
- Stenting. To help keep the narrowed portion of the artery open during balloon angioplasty, the physician may occasionally place a stent—a mesh wire tube—into the artery. When significant blockages can quickly narrow back or recoil during balloon angioplasty, stents may be employed. A drug may also be applied to the stent to stop the blood vessel from constricting once more.
- An atherectomy. An atherectomy is a minimally invasive technique used to clear an artery of plaque. To enhance blood flow, a medical professional performs an atherectomy by inserting a catheter with a revolving blade, burr, or laser into the artery that is impacted. Then, the device is used to remove or vaporize the plaque, therefore enlarging the artery.
Exercise regimens under supervision.
Walking pain in your legs can be alleviated with a supervised fitness program, which will enable you to walk farther. Walking on a treadmill under supervision at least three times a week is a standard component of an organized program.
Additionally, people with PAD should walk for at least 30 to 60 minutes each day at home. The “Start/Stop” exercise is the standard prescription:
- Continue walking until you have moderate discomfort, and then stop.
- Wait until all of the soreness has subsided.
- Step back out on foot.
Surgical or minimally invasive methods
After a few months of exercise and medication, leg pain may continue to be a concern in the day-to-day lives of some people with more severe PAD. More serious situations require people to increase blood flow to heal a wound or reduce discomfort while at rest.
Severe discomfort and restricted mobility from more advanced PAD may necessitate endovascular (minimally invasive) or surgical treatment. Peripheral artery disease can be treated with several heart disease medications, including:
Operations involving surgery
A treatment known as an arterial bypass graft involves rerouting blood flow through an artery such that it avoids a constricted or obstructed portion. A graft, which is a blood vessel (usually a vein) taken from another part of the body or a tube made of artificial materials, is attached by the surgeon above and below the restricted or blocked piece of the damaged artery. After that, blood goes through the graft and avoids the constricted or blocked section of the artery.
By making an incision in the skin above the artery, a surgeon can do an endarterectomy, which involves cutting the artery open, physically removing plaque from it, and then using bioprosthetic material to close the artery to make it wider and less likely to narrow again.
- Angioplasty.
- Stents.
- Surgery to bypass peripheral arteries.
- Atherectomy.
Treatment complications for PAD
If you experience any problems following your surgery, you should speak with your healthcare physician. These might indicate an infection or other issues:
- Discomfort, blood, or swelling where the catheter entered your body.
- Chest discomfort.
- Breathlessness.
- Chills or fever.
- Lightheadedness.
- Your legs getting swollen.
- Pain in the belly.
- An open wound that is opening.
What is the recovery period following therapy for peripheral artery disease?
Your hospital stay could be one night or several, depending on the care you received. The recovery period following an atherectomy could be a few days. After an angioplasty, however, you will require a week. Following peripheral artery bypass surgery, recovery can take anywhere from six to eight weeks altogether.
How can I lower my chance of developing peripheral arterial disease?
You could be more motivated to avoid PAD if you are aware of your risk factors. Taking care of your circulation follows the same guidelines as maintaining the health of your heart:
- Control your weight.
- Consume at least five servings of fresh fruits and vegetables each day as part of a low-fat, low-sugar diet.
- Avoid tobacco products.
- On most days of the week, get at least 30 minutes of exercise each day with your doctor’s permission.
- You should talk to your healthcare professional about your PAD risk factors if you have heart disease. Report any leg pain, weakness, or numbness you may be experiencing.
Outlook/Prognosis
What can I anticipate if I have peripheral artery disease?
Like most medical conditions, PAD is more treatable if detected early by a healthcare professional. The rate at which peripheral vascular disease advances varies depending on several factors, such as your general health and the location of the plaque formation in your body.
Prospects for peripheral arterial disease
You will have peripheral artery disease for the remainder of your life. PAD cannot be cured, but it can be controlled. There are various methods you can prevent peripheral vascular disease from getting worse:
- Engaging in regular exercise.
- Consuming less fat and eating a balanced diet.
- Controlling your risk factors, including high blood pressure, diabetes, and cholesterol.
In what ways do I look after myself?
Maintaining proper foot hygiene is essential to avoiding nonhealing sores. People with PAD should take care of their feet by:
- Wearing shoes that are comfy and fit well.
- Check for blisters, cuts, cracks, scratches, or sores on your feet and legs every day. Check for calluses, corns, ingrown toenails, redness, and increased temperature as well.
- Not delaying the treatment of a minor skin or foot issue.
- Keeping your feet hydrated and clean. (An open sore shouldn’t be moisturized.)
- When your toenails are soft after taking a wash, trim them. Smooth them with a nail file after cutting them straight across.
For specific foot care, particularly if you have diabetes, your doctor might occasionally recommend that you see a podiatrist, or foot specialist. You can get help from a podiatrist if you have calluses, corns, or other foot issues.
When should I visit my physician?
Consult your physician if you:
Get a severe infection in your foot sore. The infection may spread to your bones, muscles, tissues, and blood. Going to the hospital can be necessary if your infection is severe.
Insufficient mobility to perform daily tasks.
Experience aches in your legs while you’re sleeping. Poor blood flow is indicated by this.
FAQs
What is the prevalence of peripheral artery disease?
Between eight and twelve million Americans suffer from PAD, making it a prevalent condition. However, medical practitioners can make mistakes in diagnosing or treating PAD. The real figures are most likely greater.
Which kind of peripheral artery disease is most prevalent?
Lower-extremity PAD is the most prevalent kind, when blood flow to the legs and feet is diminished. About 10% of people have upper-extremity PAD, which is less frequent and affects the arms, hands, and fingers.
Which three symptoms indicate peripheral arterial disease?
Intermittent claudication is the word for leg pain, soreness, heaviness, or cramping that occurs during walking or stair climbing and subsides with rest.
Leg hair and toenails may cease developing.
It’s possible that one foot feels colder than the other.
What is the illness of the peripheral arteries?
The blood vessel condition known as peripheral vascular disease (PVD) develops gradually. PVD may result from blood vessel spasms, narrowing, or occlusion. Any blood vessel outside of the heart may be impacted by PVD. This encompasses the lymphatic vessels, veins, and arteries.
What is the most effective way to treat PAD?
The goals of treatment for peripheral artery disease, or PAD, are to lessen symptoms and stop the illness from getting worse. The majority of the time, claudication drugs, exercise, and lifestyle modifications are sufficient to delay or even reverse the progression of PAD symptoms.
How can I do a home PAD test?
Raise your leg over the 60-degree mark and hold it there for 30 to 60 seconds. If you have discomfort, coldness, or numbness in your upper extremities, you may have a blood flow issue. If you experience any of these symptoms, make an appointment with a PAD expert, such as Dr.
Which vitamin is best for peripheral arterial disease?
Discovered that taking vitamins A, C, E, B6, and B12 was linked to a decreased risk of developing PAD. Additional investigation revealed a correlation between a lower prevalence of PAD and consumption of fiber, vitamins A, C, E, B6, folate, and n-3 PUFAs. The latest is Naqvi et al.
Can a PAD be cured by walking?
Regular physical exercise is one of the best strategies to prevent and treat peripheral artery disease, or PAD. Dr. Eduardo Sanchez walks us through a basic walking exercise that will help reduce the symptoms of PAD and strengthen our legs, which will make it easier to walk and climb stairs.
References
- Peripheral artery disease (PAD) – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/symptoms-causes/syc-20350557
- Peripheral artery disease. (2025, January 6). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17357-peripheral-artery-disease-pad
- About Peripheral Arterial Disease (PAD). (2024, May 15). Heart Disease. https://www.cdc.gov/heart-disease/about/peripheral-arterial-disease.html
- Peripheral artery Disease (PAD). (2023, September 13). Yale Medicine. https://www.yalemedicine.org/conditions/peripheral-artery-disease-pad




One Comment