Olfactory Nerve Disorders
Olfactory nerve disorders are conditions that affect the olfactory nerve, which is responsible for your sense of smell. A variety of problems about your sense of smell may arise from these disorders.
The olfactory nerve (CN I) is the first cranial nerve in your body.. This nerve regulates your sense of smell and olfactory system. The shortest sensory nerve is the first cranial nerve. It terminates in the interior, the top portion of your nose, having begun in your brain. A variety of illnesses, such as COVID-19, diabetes, and Alzheimer’s can impact cranial nerve 1.
If you experience problems with your sense of smell, it’s crucial to consult your healthcare professional. Numerous research indicates that certain individuals might benefit from scent training. According to researchers, this might be because identifying or even picturing a certain scent frequently stimulates different parts of the brain.
What is the olfactory nerve?
The olfactory nerve (CN I) is the first cranial nerve. It is also a component of the autonomic nervous system, which controls bodily processes. This nerve enables your sense of smell. The shortest sensory neuron in your body is the first cranial nerve. It originates in your brain and terminates in the inside, top portion of your nose.
Anatomy of the Olfactory Nerve
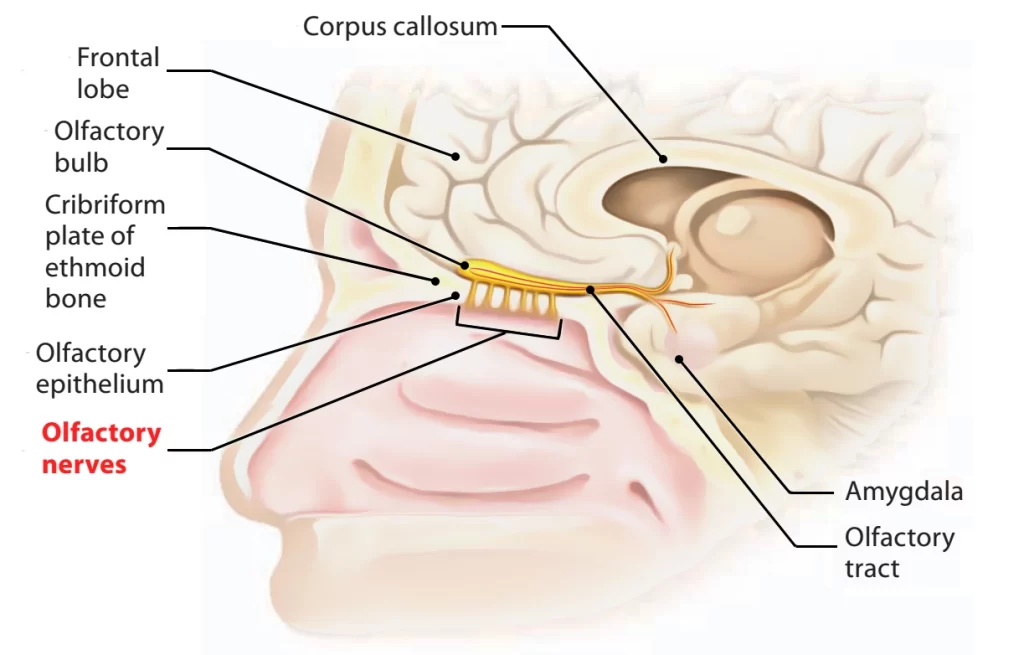
The olfactory nerve (sometimes called the vision nerve or cranial nerve 2) is one of the two nerves that originate directly from the cerebrum. This is the upper portion of your brain. Among the lower areas of your brain where other cranial nerves start to originate are the midbrain, pons, and medulla oblongata, which are referred to as your brainstem.
The olfactory nerve fibers and the olfactory bulb, which is situated in the upper part of your nose, are separated by short lengths. Your cribriform plate serves as a path for the nerve fibers that go to your olfactory bulb. This pale, porous bone in your skull divides your brain from your nasal cavity.
Function of the Olfactory Nerve
CN It enables the detection of fragrances, odors, perfumes, and more. Smelly substances release microscopic molecules. These chemicals enter your nose when you inhale. These compounds are detected thereby unique cells called olfactory receptors. Your olfactory nerve transmits this information to your brain via the receptors, enabling you to detect scent.
Your olfactory system enables the perception of smell in two ways:
- Nostrils: Odor-producing substances release small molecules that can activate olfactory receptors. Certain combinations of receptors allow you to differentiate between various odors.
- Back of your throat: Chewing food or sipping liquids causes chemicals to be released that aid in smell. These molecules ascend your throat and reach the rear of your nose’s olfactory receptors.
Your sense of smell is greatly influenced by your olfactory mucosa. This membrane, which is located in the upper nasal cavity, is made up of several cell types.
- Olfactory receptor cells: The dendritic process and central process are supported by olfactory receptor cells. In your olfactory mucosa, dendritic processes direct cells toward microscopic hairs where they activate olfactory cells. Cells are directed in the opposite direction by central systems.
- Sustentacular cells: these give neighboring tissue support.
- Basal cells: Olfactory receptor cells and sustentacular cells originate from basal cells.
What is Olfactory Nerve Disorders?
Olfactory nerve disorders may impact your sense of smell. They happen when there’s a problem with the olfactory nerve, which sends signals connected to smell from your nose to your brain.
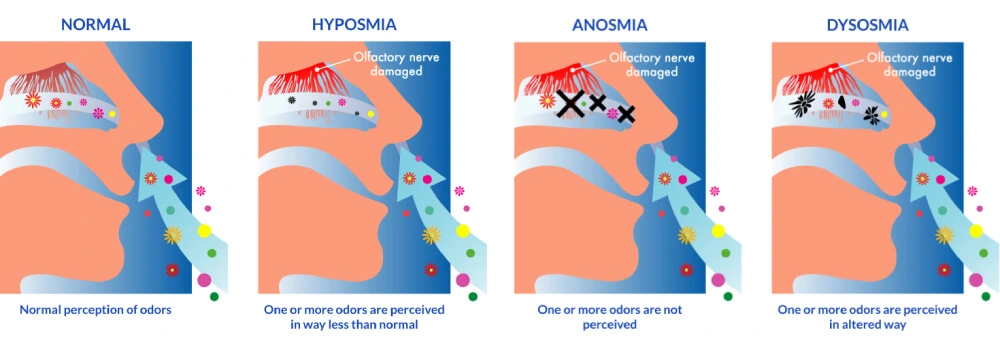
Olfactory nerve diseases fall into a few primary categories:
- Anosmia: The total absence of scent.
- Hyposmia: A reduction in your sense of smell.
- The term dysosmia refers to a deceived sense of smell.
- Congenital anosmia, or malfunctioning of the olfactory nerve, occurs in certain individuals at birth.
It’s crucial to visit a doctor if you’re having issues with your sense of smell so they can identify the underlying issue. The cause of olfactory nerve problems will determine the course of treatment. While there may not always be a cure, there are coping mechanisms you can try to deal with your loss of scent.
Diseases and Conditions that impact the Olfactory Nerve
The following illnesses and other circumstances may have an impact on olfactory nerve function:
- Sinus infection and Nasal polyps
- Tobacco use.
- Inadequate dental care.
- Substances such as pesticides and environmental pollutants.
- Severe brain trauma, such as concussions.
- Drugs such as antibiotics.
- The virus responsible for coronavirus (COVID-19) sickness is SARS-CoV-2.
- Carcinoma of the head and neck.
- Diabetes.
- Alzheimer’s Disease.
- Brain tumor.
- Parkinson’s Disease.
- Seizures.
Causes and Symptoms Olfactory Nerve Disorders
Your sense of smell can be affected by several illnesses and injuries. These may result in phantom scents, a weaker or absent sense of smell, or even an enhanced sense of smell. Some symptoms linked to faulty odor perception are referred to as the following:
- Dysosmia: Dysosmia can produce phantom smells, or smells that aren’t there, or it may alter how you perceive real smells. This is called an olfactory hallucination. The olfactory epithelium’s deterioration is typically to blame for this.
- Anosmia: A complete absence of smell is known as anosmia. A head injury, obstruction, or infection could be the cause.
- Hyposmia: Hyposmia is a diminished sense of smell. Allergies, nasal polyps, viral infections, and head trauma are among the possible causes.
- Hyperosmia: Having an acute sense of smell, hyperosmia is a rather uncommon disorder. It can arise as a result of pregnancy, Lyme illness, autoimmune diseases, or other conditions. It can also happen on its own occasionally. Some smells can make you extremely uncomfortable and increase your risk of headaches, migraines, nausea, and vomiting. Scents from candles, cleaning supplies, perfumes, and chemicals are the ones most likely to cause symptoms.
Your perception of taste is also greatly affected by changes to your sense of smell.
Olfactory Loss Following Virus
- Although other viral infections can also affect the olfactory nerve, the common cold is the most common cause.
- You are probably aware that when sinus congestion in your nose fills up, it can cause a reduction in your sense of smell, which returns when the congestion goes away.
- On occasion, though, it takes some time to return completely. Everyone has probably encountered post-viral olfactory loss (PVOL) at some point. Although the exact reason for this is unknown, researchers believe that some viruses, such as those that cause the common cold and influenza, harm the olfactory epithelium and mucous membrane in some way.
- Some people’s sensitivity to smells will abruptly and noticeably decrease. In others, which most people experience a few times a year, it’s a progressive loss over several acute diseases.
Post-Traumatic Olfactory Loss
- A brain injury can cause post-traumatic olfactory loss (PTOL), which is anosmia or hyposmia. The extent of the damage and the area of the skull that is injured are related to the loss. The most common injuries that result in a loss of smell are those to the back of the head.
- Given that the olfactory nerves are located near the front of the brain, that may appear strange. The brain may thrust forward and strike the inside front of the skull the location of the olfactory nerve in the event of a blow to the back of the head.
- The delicate nerve fibers are then pulled when the brain rebounds, and they may snag on the jagged edges of the tiny openings in the skull through which they emerge.
- This can cause a severe injury to the olfactory nerves, but more frequently, olfactory bulb bruises cause a loss of smell. A blow to the nose or other facial injuries might potentially result in PTOL.
Additional Reasons for Olfactory Loss
- Reduced sense of smell can also be a prelude to some neurological disorders like Parkinson’s, Alzheimer’s, and Lewy body dementia, as well as tumors like meningiomas of the olfactory groove.
What effects does COVID-19 have on the sense of smell?
Loss of smell affects up to 50% of COVID-19 patients. Researchers continue to investigate why. However, olfactory receptors may be harmed by viral infections such as SARS-CoV-2, the virus that causes COVID-19. Many people have olfactory recovery. However, it can take several months.
Diagnosis Of the Olfactory Nerve Disorders
Olfactory abnormalities are frequently diagnosed after a thorough history and physical examination. During a physical examination, nasal polyps and signs of a viral infection may be found. A thorough medical history can identify potentially hazardous exposures.
Psychophysical examination (olfactory test)
- To determine the extent of olfactory dysfunction by a qualified professional, a psychophysical examination is required. It is also beneficial to monitor the development or reversal of olfactory dysfunction.
- A test called the University of Pennsylvania Smell Identification Test may be administered to determine whether hyperosmia or anosmia is present. Further testing will depend on several circumstances because there are numerous potential explanations, including nutritional issues, brain abnormalities, and more.
Electrophysiological examination
- Three electrophysiologic tests, including the olfactory event-related potential (OERP), electroencephalogram (EEG), and electro-olfactory (EOG), have been conducted. EOG is an invasive process that lacks reliability, while EEG only captures the olfactory stimuli’s indirect influence. Consequently, it is uncommon to find these two tests applied in clinical practice or research environments.
- Similar to the auditory brainstem response (ABR), the OERP can distinguish between false impressions and detect residual olfactory functioning. OERP was detectable in certain groups of hyposmia patients but not in any anosmic patients. More research will be required, but the prognosis may be reflected in the absence of OERP in hyposmia. Electrophysiologic examinations are currently largely utilized in research stages.
- Both the psychophysiologic and electrophysiologic examinations have certain drawbacks. They offer little information regarding the lesions’ location and cannot accurately differentiate between central and peripheral loss.
Imaging examination
- Imaging studies should be utilized carefully for diagnosing olfactory impairment because they are usually negative. As such, they are not recommended consistently. Imaging tests like CT and MRI are not able to provide additional information, even in the case that thorough histories (risk factors and past incidents) and physical examinations (nasal endoscopy) are negative.
- Nevertheless, imaging might be beneficial in certain instances of tumorous, inflammatory, traumatic, neurodegenerative, and structural disorders. Kallmann syndrome (congenital agenesis of olfactory bulbs) can be confirmed by MRI. Since olfactory impairment is not often linked to brain cancers, imaging screening for brain tumors is not required.
- Functional magnetic resonance imaging (fMRI) will be useful in the screening and early diagnosis of neurodegenerative disorders such as multiple sclerosis, Parkinson’s disease, Alzheimer’s disease, and others. It has recently been utilized to evaluate active areas in the brain by olfactory stimulation. Nevertheless, research is currently the main purpose for it.
Treatment Of the Olfactory Nerve Disorders
Treatment and Managing With the Loss of a Sense of Smell
- There are no particular therapies that can undo changes in one’s ability to smell. Dysomia can occasionally go away on its own with time. High-dose supplements of zinc and vitamin A have been studied, however, the results are not encouraging at this time.
- Olfactory training is being tested now, and preliminary research suggests that it may be useful. Numerous research indicates that certain individuals might benefit from scent training. According to researchers, this might be because identifying or even imagining a certain scent frequently stimulates different parts of the brain. The majority of investigations have utilized widely used essential oils.
- That makes coping the main objective of treatment. Safety precautions, such as making sure you have a fire alarm, are crucial for people who are olfactory deficient. Given that some foods and spices are more likely to activate the receptors (trigeminal and olfactory chemoreceptors), nutritional counseling may be beneficial.
- Your sense of smell may gradually return if the source of your loss is known and curable, such as surgically removing nasal polyps, realigning the septum, or treating sinus congestion.
- In many cases of post-viral olfactory loss, that is what occurs; nonetheless, the sensation may never entirely recover. More than 80% of participants in a 2014 study stated that their olfactory abilities had improved a year after receiving a diagnosis of loss.
- If Parkinson’s syndrome or Alzheimer’s disease is the cause of your decreased sense of smell, your treatment options will typically focus on treating the illness rather than the reduced sense of smell.
- In general, those with post-traumatic olfactory loss have a worse prognosis. While some people may never fully recover their sense of smell, others might have gradual improvements. The degree of restoration is typically based on how serious the damage was.
- Scar tissue may make it impossible for olfactory nerve cells to ever reattach to the olfactory bulb, even though they are capable of growing new nerve fibers. It’s also possible that the new fibers won’t be able to pass through the microscopic openings in the bone beneath the nose.
- For certain individuals with Parkinson’s disease and PTOL, smell training may be helpful.
When should contact a medical professional if having olfactory nerve issues?
If you observe any of the following, you should speak with a doctor:
- A change in the overall scent.
- Quick loss of scent perception.
- Smells bad without any reason.
It’s critical to get medical help if you experience these symptoms. They could put you at risk for the following health and safety problems:
- If you can’t smell the meal, you’re either eating too much or not enough.
- Ignoring warning indicators of danger, such as a gas leak, fire smoke, or spoiled food.
Precaution Of the Olfactory Nerve Disorders
There are some situations where you might not be able to stop your sense of smell from being affected. It might not be possible to prevent complications from brain tumors or neurological diseases.
- Avoiding risky activities that could cause brain damage is one preventive action that you can take.
- Obtaining a COVID-19 vaccination.
- wearing a mask to shield your nose from chemical exposure.
- If you smoke, vape, or use other tobacco products, stop using them.
- Regularly brushing and flossing your teeth.
- keeping up with medical interventions for ailments that may impact your sense of smell.
- using helmets and other safety gear when playing sports to prevent concussions.
Summary
The first cranial nerve in your body is your olfactory nerve (CN I). Your sense of smell is functioned by this nerve. Cranial nerve 1 is susceptible to several illnesses such as COVID-19, diabetes, and Alzheimer’s disease. If you experience problems with your sense of smell, it’s crucial to consult your healthcare professional. They can inform you if it will reappear or go back to normal. They might also talk about how to avoid it and yet be safe and healthy.
FAQs
Why does olfactory damage occur?
Head injuries, viral infections, neurodegenerative disorders, and sinonasal diseases are the main causes of olfactory impairment.
What condition affects the nerve that senses smell?
Nasal and paranasal diseases account for 23% of common causes of olfactory loss and dysfunction; these are followed by upper respiratory infections (19%), head trauma (15%), idiopathic exposure or drugs (10–25%), and other conditions include aging, neurological disease, congenital abnormalities, and drug exposure.
What signs and symptoms are present in olfactory disorder?
The range of symptoms is from complete loss of smell and taste to diminished perception of certain tastes and smells, such as sweet, sour, bitter, or salty foods. Occasionally, tastes or odors that are usually pleasurable can turn unpleasant.
What can I do to enhance my sense of smell?
The majority of experts advise scent training, which involves inhaling essential oils like lemon, eucalyptus, cloves, rose, and others daily to revive the olfactory nerves.
Can olfactory nerves be capable of healing?
Even though the olfactory system is remarkably capable of neuronal regeneration and recovery after injury, the olfactory function does not recover in many cases of serious head injury. What elements are most important in predicting olfactory function recovery after a head injury is unknown.
References
- Professional, C. C. M. (n.d.-g). Olfactory nerve. Cleveland Clinic. https://my.clevelandclinic.org/health/body/23081-olfactory-nerve
- Peter Pressman, MD. (2022, November 4). Overview and causes of olfactory disorders. Verywell Health. https://www.verywellhealth.com/disorders-of-olfaction-2488765
- Olfactory nerve | anatomy. (n.d.). Encyclopedia Britannica. https://www.britannica.com/science/olfactory-nerve
- Smell disorders. (2023, July 31). NIDCD. https://www.nidcd.nih.gov/health/smell-disorders
- Holbrook, E. H., MD. (n.d.). Disorders of Taste and Smell: Introduction and background, Anatomy and physiology, Etiology of smell and taste Disorders. https://emedicine.medscape.com/article/861242-overview?form=fpf