Neurapraxia
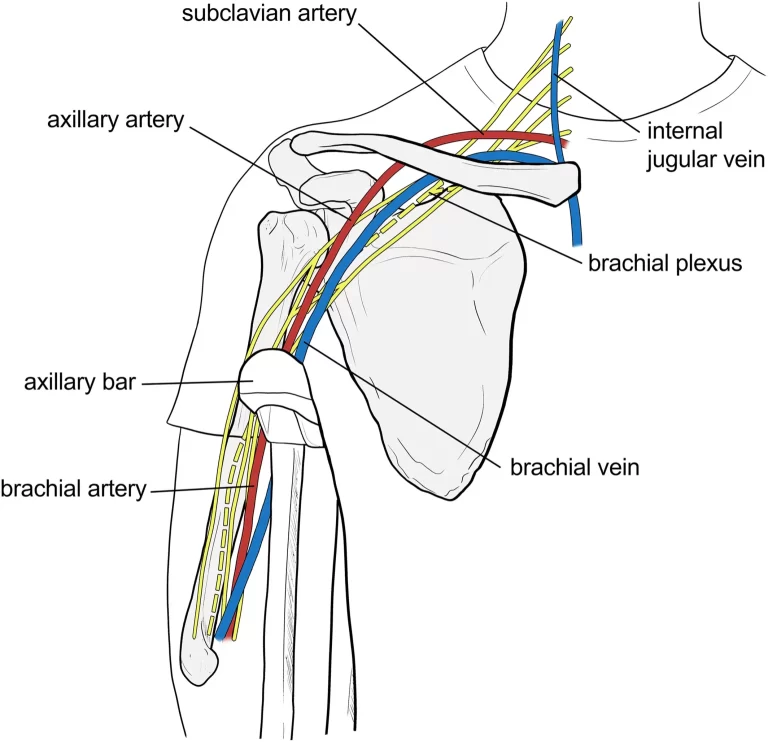
The mildest type of peripheral nerve injury, known as neurapraxia, is frequently caused by focal demyelination or ischemia. Neurapraxia makes nerve impulse conduction harder in the damaged location.
There is either whole or partial loss of motor and sensory conduction. When you have neurapraxia, you experience burning, stinging, and pain due to damage to your peripheral nerve or nerves.
These little nerve damage normally heal on their own with time and rest. Your risk of neuropraxia can be decreased by donning protective gear when participating in contact sports and physical activities like cycling.
What is the Neurapraxia?
- Neurapraxia is a modest type of nerve injury that can cause temporary loss of motor and sensory loss.
- The mildest form of peripheral nerve injury (PNI) is neurapraxia. Grades I through V make up PNIs, which are divided into five levels. Growing amounts of nerve injury are the basis for the differences between these levels.
- Neurapraxia refers to grade 1 PNIs. Under certain circumstances, neither the surrounding connective tissue nor the nerve axon the long segment of the cell that transmits electrical signals are harmed.
- The symptoms of neurapraxia are caused by a block that forms along the nerve, preventing electrical signals from traveling through. The injured area of the nervous system cannot communicate with other areas of the nervous system until this block is removed.
- Nerve injury most commonly occurs as a result of neuropathy. Although PNIs are underreported, the approximate annual incidence is 13–23 cases per 100,000 persons.
What are the causes of the Neurapraxia?
Neurapraxia typically arises by compression and ischemia, or a lack of blood supply to a tissue or area. Generally, inflammation is a common reason.
Although the actual mechanism of nerve blockage is unknown, neurapraxia is more common in nerves that travel via small bodily apertures.
One frequent consequence of surgery is neurapraxia. During surgery, it is usually caused by:
- Incorrect body positioning throughout the procedure.
- Inadequate body support cushioning.
- The application of tourniquets and several more surgical tools.
- Side effects of anesthesia can include nerve damage from chemicals or blood vessel narrowing that stops your blood supply.
Neurapraxia is more common after certain procedures than others. For instance, all anterior cruciate ligament (ACL) reconstruction surgeries include a 75% risk of neurapraxia, yet hip replacement surgeries carry a less than 1% risk.
Neurapraxia also affects particularly specific nerves in and around the mouth in certain dental scenarios, such as:
- Some molar extraction procedures
- oral illnesses
- Anesthesia injections
Outside of a medical context, additional potential causes of neurapraxia include:
- Car crashes
- Falling
- sports injuries
- injuries from gunshots
If the neurapraxia occurs outside of a medical facility, you must inform your physician of the precise moment the event occurred about the onset of your symptoms. This will assist them in determining the extent of the injury and whether compression or blood loss is most likely to be the cause.
If the neurapraxia occurs outside of a medical facility, you must inform your physician of the precise moment the event occurred concerning the onset of your symptoms. This will assist them in determining the extent of the injury and whether compression or blood loss is most likely to be the cause.
What are the symptoms of the Neurapraxia?
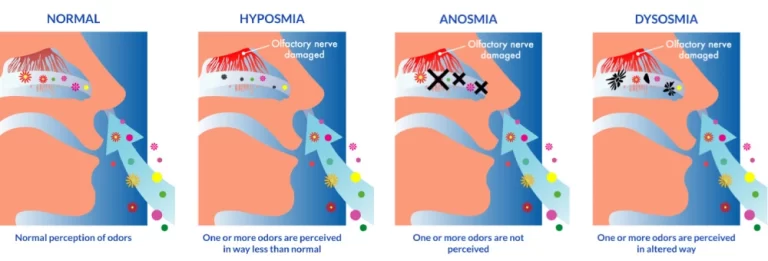
Neurapraxia symptoms vary depending on which nerve and at which location is blocked. They may consist of:
- Muscle Weakness.
- Pain.
- Sensitivity to touch.
- lack of sensation.
- loss of motor skills.
- tingling.
- Numbness.
Neurapraxia symptoms may not show up right away following the injury. It could take weeks for symptoms to manifest. In this instance, inflammation is typically the root cause, squeezing the nerve and resulting in injury.
Generally speaking, compression-induced neurapraxia creates the neural blockage more slowly and has longer-lasting symptoms than blood-loss-induced neurapraxia. Blood loss is the cause when the blockage and symptoms appear and go more quickly.
How is Neurapraxia diagnosed?
Diagnosing neuropraxia and other forms of acute peripheral nerve damage can be challenging. This indicates that cases are frequently not reported enough. Additionally, they could need blood tests to determine your
- Complete blood count (CBC).
- Renal function.
- Liver function.
- Thyroid function.
However, your doctor can use nerve conduction testing to pinpoint the precise position of the block along a specific nerve. The tests gradually focus on an area of your nerve where the electrical signal is unable to travel any farther.
It may be necessary to use some imaging tests, such as magnetic resonance imaging (MRI), to confirm that your symptoms aren’t being caused by even more serious nerve or tissue damage.
Your doctor may prescribe tests for nerve and muscle function as well as imaging exams. These tests evaluate the extent of nerve injury. They could employ:
- CT scan.
- EMG.
- MRI.
- ultrasound of the muscles and peripheral nerves.
- X-ray.
What Neurapraxia Treatment Is There?
For neurapraxia, you often won’t require any extra care. If you leave the nerve injury alone for a few days or weeks, it will recover on its own.
Additional potential therapies consist of:
- Analgesics
- Putting the afflicted area to rest
- Stay away from aggravating activity
- Replacing outdated equipment with newer models or fortifying current models. Athletes might
- Have to wear braces or alter their training equipment, for instance.
- Your doctor may suggest range-of-motion exercises as part of a neuropraxia physiotherapy treatment plan. Acupuncture and massage may also be beneficial, but only if prescribed by your physician.
Prognosis
For neurapraxia, recovery rates are excellent. In one to four weeks, the nerves should be able to mend on their own. You will have fully restored all of your senses and abilities by this point.
Tell your doctor how the healing of your neurapraxia is going. They will want to ensure that you restore all of your sensory and motor skills as soon as possible.
Are there any complications that result from Neuropraxia?
The majority of neurapraxia sufferers fully recover. However, some people experience issues like:
- Inflammation.
- Persistent numbness, weakness, or discomfort in the nerves.
- Tissue scars close to the site of damage.
- If scar tissue develops, surgery can be required. For your nerve to heal, surgeons must remove scar tissue to remove nerve compression.
What are the physical therapies for the Neurapraxia?
Physical therapy’s most important goals are to:
- Modalities: Pain and inflammation-relieving therapies using heat, ice, or ultrasound.
- Reduce pain. Massage, heat therapy, and ultrasound are some of the techniques that can help with this.
- Improving range of motion: Light exercise and stretches can prevent stiffness and contractures.
- Muscle strengthening: Exercises aim to strengthen the weakening muscles and enhance their functionality.
- Balance and coordination: The goal of the exercises is to retrain the damaged area to move smoothly.
- Functional training: To help you restore your independence, exercises center on commonplace tasks.
- Neuromuscular re-education: Activities aimed at retraining the brain and nerves to function in concert are known as neuromuscular re-education.
Summary
A little injury to the peripheral nerves, known as neurapraxia, normally recovers on its own with time and relaxation. For advice on how to effectively manage pain and other symptoms, consult your healthcare professional.
Depending on the extent of their injuries, patients may benefit from neuropraxia to fully recover in a few days to several months. During your recuperation, you can have a decreased range of motion and weakness. The best indicators that you’ve healed include not experiencing any symptoms and possessing the same level of strength and flexibility as before the accident.
A nerve should not relapse to neurapraxia if it heals completely. But any physical damage, whether from sports or another source, can result in a fresh instance of neurapraxia.
FAQs
Neurapraxia: What is it?
Peripheral nerve injury is known as neurapraxia. Your brain and spinal cord send electrical impulses to these nerves, which then distribute those signals to the rest of your body.
Who is affected by neurapraxia?
Neurapraxia can affect anyone. The illness may develop following a trauma, such as a fall, auto accident, or sports-related injury.
How can one experience neurapraxia?
When you have neurapraxia, you experience burning, stinging, and pain as a result of damage to your peripheral nerve or nerves. Minor nerve injuries normally heal on their own over time and with rest. Your risk of neurapraxia can be decreased by wearing protective gear when participating in contact sports and physical activities like cycling.
How can I reduce the possibility of neurapraxia complications?
To stop more nerve damage, ensure the wounded area is protected while it heals. Sports and other physical activities may need to be put on hold while you recover.
How much time does neurapraxia take to recover?
Depending on the severity of your injury, neurapraxia may last for a few days or several months. The majority of neurapraxia sufferers fully recover. However, some people particularly older adults may require more time to heal.
Does neuropraxia always exist?
Most people fully recover as soon as the myelin in their nerves heals itself. However, neurapraxia can recur in the event of another accident.
References
- Professional, C. C. M. (n.d.-b). Neurapraxia. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22608-neuropraxia
- Anderson, A. (2024, March 7). What Is Neurapraxia? WebMD. https://www.webmd.com/brain/what-is-neurapraxia
- Neurapraxia. (2024, April 19). Wikipedia. https://en.wikipedia.org/wiki/Neurapraxia
- Roland, J. (2017, August 10). What Is Neurapraxia? Healthline. https://www.healthline.com/health/neurapraxia#outlook
- Neurapraxia – What You Need to Know. (n.d.). Drugs.com. https://www.drugs.com/cg/neurapraxia.html