Lumbar Radiculopathy
Lumbar radiculopathy refers to a condition where the spinal nerve roots in the lower back, specifically the lumbar region, are compressed or irritated. This compression can result from various factors, such as herniated discs, bone spurs, degenerative disc disease, or spinal stenosis.
Definition
The condition known as lumbar radiculopathy is an inflammation of a nerve root in the lower back, resulting in back and leg discomfort or irritation. A condition that frequently affects the sciatic nerve, hence it is also known as sciatica.
Anatomy of the lumbar spine
To comprehend this condition, it is helpful to grasp the following spine components:
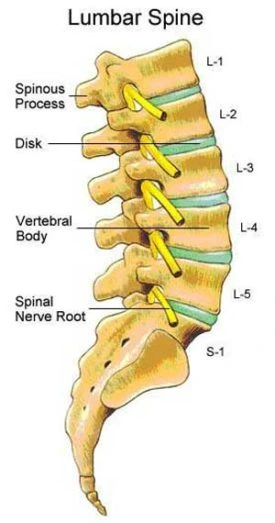
- Vertebrae. The spine is made up of these bones arranged together. The lumbar spine contains five vertebrae.
- Discs- These are soft tissue cushions that sit between the vertebrae. They act as shock absorbers in the spine.
- Spinal Canal. This is an opening developed inside the arranged vertebrae. This canal is where nerves flow in the lumbar spine.
- Nerves. These branch out and go away from the spinal canal, traveling to various body regions. Nerves get out of the spinal canal through holes between the vertebrae. The nerve root that is nearest to the spinal canal.
- Sciatic Nerve. This big nerve originates from multiple nerve roots in the lower back. This nerve travels down the back of the leg to the foot.
What causes lumbar radiculopathy?
Several causes may lead to lumbar radiculopathy:
Aging, injuries, bad posture, excess body weight, and other factors can all contribute to lower back problems. These disorders may irritate nerve roots. They include:
- A lumbar spinal disc has been damaged. The injured disc may then push on neighboring nerve roots

- Degeneration due to wear and tear, as well as aging. This can cause narrowing (stenosis) of the spaces between the vertebrae. The restricted holes press upon nerve roots as they exit the spinal canal.
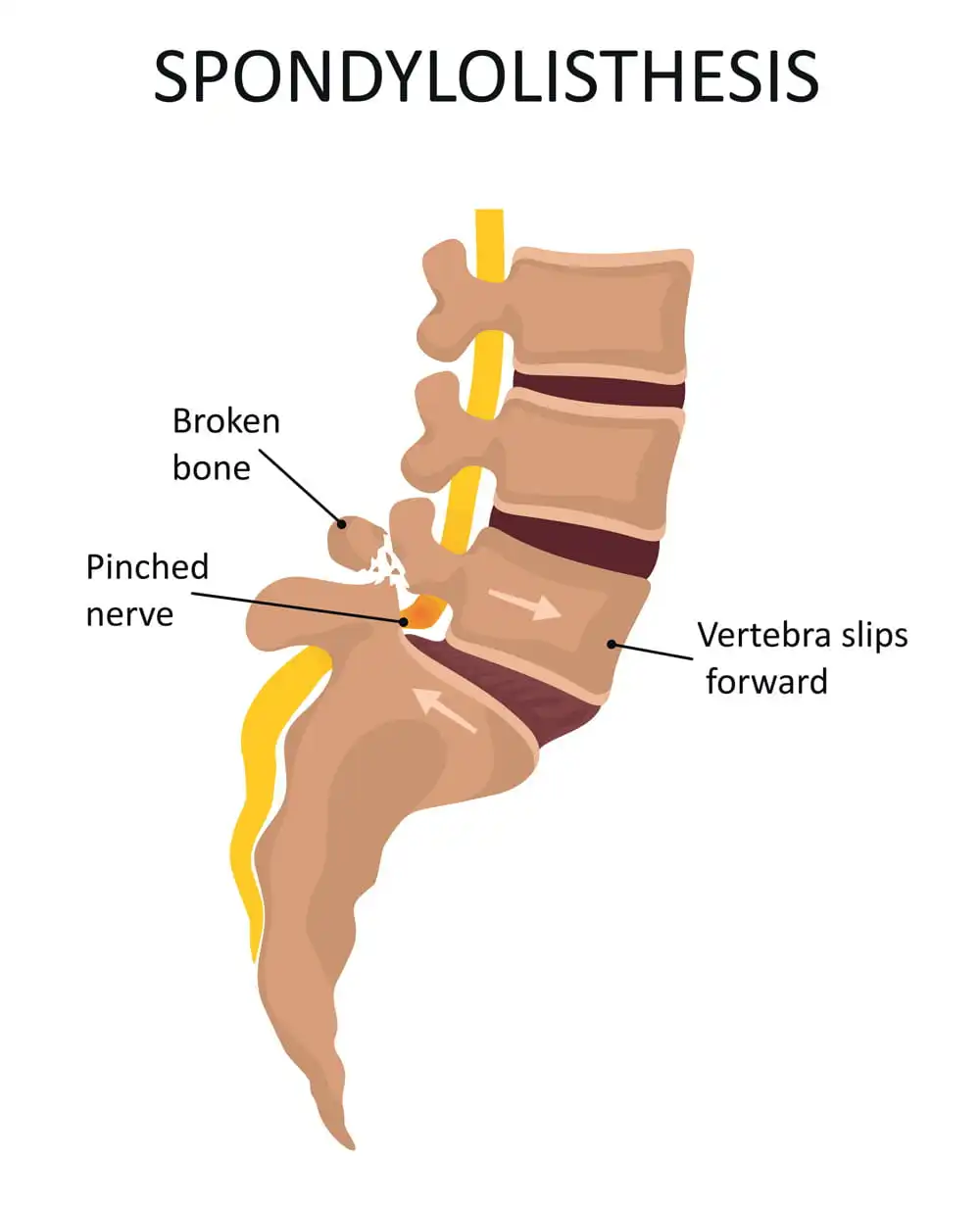
- Unstable spine (spondylolisthesis) This is when a vertebra slips forward. It might then impinge on the nerve root.
- Injuries such as falls, car accidents, or sports-related incidents can damage the spine and soft tissue around it.
- poor posture (lordosis) is excessive curvature of the lumbar spine that may further lead to damage to discs or nerves.
- Other, less common things can put pressure on nerves in the lower back. Diabetes, infection, and tumors are a few examples.
- spinal tumors or other inflammatory conditions like AS may put pressure on the spinal canal and put pressure on the nerves which results in radiculopathy.
What are the risk factors for Lumbar Radiculopathy?
- Age is the most important risk factor for lumbar radiculopathy. The highest age range is 45 to 64. Men have the greatest impact in their 40s, while women are affected in their 50s and 60s.
- Men have a higher risk than women in general, although particular subgroups of women are at a higher risk.
Other modifiable risk factors include:
- Obesity: Carrying more weight affects the mechanics of the spine, making nerve compression more likely to occur
- Occupation: Occupation: your profession involves hard lifting and twisting actions.
- Sedentary lifestyle: inactivity can result in weak core muscles, putting more strain on the spine.
Non-modifiable risks include:
- Arthritis: any degenerative joint condition can affect the lumbar vertebrae
- Previous injury: Spinal trauma can alter bone and disc tissue.
- Pregnancy: Hormones impact the strength of ligament tissue during pregnancy.
- Congenital factors: gaps in the spine through which nerves travel might be smaller owing to hereditary reasons.
What are the Symptoms and Signs of Lumbar Radiculopathy?
Lumbar radiculopathy also known as sciatica when it involves the sciatic nerve can cause a range of signs and symptoms that often affect one side of the body.
The symptoms could appear anywhere throughout the sciatic nerve’s path. This is substantial since branches of the nerve reach your feet.
the most common complaints are:
- Lower back pain can be followed by other symptoms and experiences.
- Tingling or numbness following the nerve’s route, frequently across the buttock, back of the thigh, and calf on the affected side
- Muscle weakness
- sensation or reflex changes, hypersensitivities such as hyperesthesia, or hypothesis
- symptoms worsening with movements such as Activities that involve bending, twisting, lifting, or prolonged sitting or standing can exacerbate symptoms of lumbar radiculopathy. Coughing, sneezing, or straining may also worsen pain due to increased pressure on the nerve roots.
- Pain can range from dull, aching to intense, electric-shock feelings, which are frequently triggered by unexpected movements, coughing, or sneezing. You may also feel like your lower back movement is limited.
How to diagnose Lumbar Radiculopathy?
Lumbar radiculopathy is diagnosed with a full assessment that includes a medical history, a physical examination, and, in particular situations, imaging (MRI, CT-myelogram) and nerve conduction investigations.
Physical Examination:
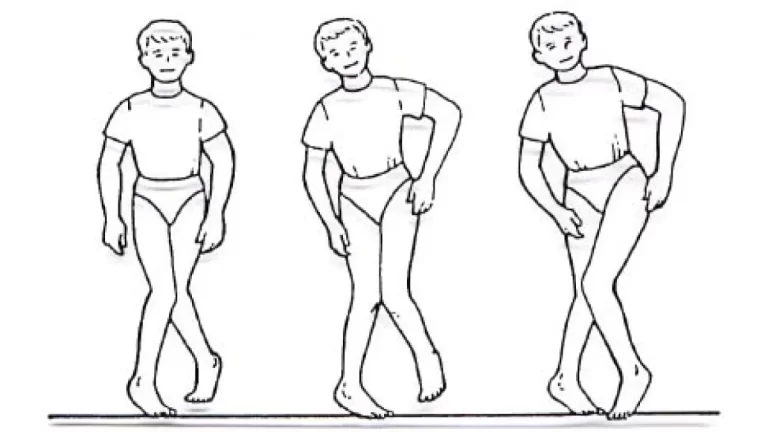
The physical examination for lumbar radiculopathy is a way to assess nerve function, muscular strength, reflexes, and signs of nerve compression in the lower back, buttocks, thighs, and legs.
Lower Back Examination:
Range of Motion: The provider will assess your ability to move your lower back in different directions, such as flexion (forward bending), extension (backward bending), lateral bending (side-to-side), and rotation. Restricted range of motion or pain during movement may indicate lumbar spine issues.
Tenderness: Palpation of the lower back area helps identify areas of tenderness, muscle spasms, or localized pain that may be associated with nerve compression or spinal abnormalities.
Imaging Studies:
X-ray: X-rays can reveal degenerative changes in the lumbar spine, such as osteoarthritis, disc space narrowing, bone spurs (osteophytes), and facet joint degeneration.
Magnetic resonance imaging (MRI) or computed tomography (CT): These imaging studies can reveal herniated discs, spinal stenosis, soft tissue injury, Bulging, Herniated discs, bone spurs, or other abnormalities that may be causing nerve compression and radiculopathy.
Nerve Conduction Studies: nerve conduction studies or electromyography (EMG) may be performed to evaluate nerve function, These tests can help determine the severity of radiculopathy and identify the specific nerve roots affected.
Special Tests:
- Straight Leg Raise Test: This test involves raising one leg while lying down with the knee straight. Pain radiating down the leg (sciatic nerve distribution) at an angle of less than 60 degrees is considered a positive test for lumbar radiculopathy.

- Lasegue’s Sign: Similar to the straight leg raise test, Lasegue’s sign is positive if raising the leg while lying down reproduces leg pain or sciatic nerve symptoms.
- Lumbar Extension Test: The provider may ask you to lean backward (extend) while standing to reproduce or exacerbate symptoms of radiculopathy, such as leg pain or tingling
Treatment of Lumbar Radiculopathy
Medications
Medications commonly used to manage the symptoms of lumbar radiculopathy (lower back pain due to nerve compression) include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): medications like ibuprofen (Advil, Motrin) and naproxen (Aleve), as well as prescription NSAIDs. They aid in decreasing pain, inflammation, and discomfort.
- Acetaminophen: Also known as paracetamol, acetaminophen (Tylenol) is an over-the-counter pain reliever that can be used to alleviate mild to moderate pain associated with radiculopathy.
- Topical Analgesics: creams, gels, or patches containing medicines such as lidocaine or capsaicin that may be administered directly to the painful area to provide localized pain relief.
Physical therapy treatment
Physical therapy is an effective and safe treatment option for relieving discomfort, strengthening your muscles, and even preventing future harm.
Physical therapy activities that may be effective in treating your lumbar radiculopathy include:
hands-on manual therapy to your spinal joints, muscles, or nerves to reduce inflammation of nerve roots by restoring normal mechanics around the nerve. Once the nerve root inflammation improves, you will begin workouts to strengthen the muscles surrounding the nerve root, which will aid in maintaining proper nerve mechanisms. Finally, you will be taught how to do activities with proper ergonomics to safely return to activities of daily life or activities that have been restricted because of this condition.
Assessment
The physical therapist begins by conducting a comprehensive assessment to understand the patient’s medical history, current symptoms, functional limitations, and specific goals for treatment.
Physical examination includes evaluating posture, range of motion, muscle strength, sensation, reflexes, and any neurological deficits related to nerve compression.
Pain management
Teach strategies for pain management, including the use of heat or cold packs, proper body mechanics, ergonomic adjustments at work or home, relaxation techniques, and contributing factors such as Poor posture, poor lifting techniques, or sedentary living habits.
Modalities:
Soft-tissue modalities are typically integrated into a back pain program. These methods use particular manual techniques, such as myofascial release therapy or massage therapy, to relieve the patient’s soft-tissue discomfort.
- Heat Therapy:
- Application of heat packs or warm compresses to the lower back to relax muscles, increase blood flow, and reduce pain.
- Cryotherapy– Cold Therapy:
- Ice packs or cold therapy for acute pain or inflammation management, are applied controlled to avoid skin damage.
- Infra-red Radiation:
- Application of IRR for improving the blood flow at the lower back area and decreasing muscle tension.
- Electrical Stimulation:
- Transcutaneous Electrical Nerve Stimulation (TENS) or Interferential current therapy (IFC) used to alleviate the pain
Traction
Traction involves applying a pulling force to the spine, which aims to create space between vertebrae, reduce pressure on spinal discs, and alleviate nerve root compression. Lumbar traction takes around 1.5 times the person’s body weight to bring about vertebral body separation. However, this treatment is complicated and time-consuming; also, most people find lumbar traction difficult to handle.
Exercise
- isometric exercise for the back and abdomen will ease the pain and strengthen the back and core muscles.
- Pelvic tilt
- Pelvic tilts activate pelvic floor muscles and strengthen your abdominal muscles. and improve lumbar stability.
- Lie back on the floor with your knees bent. Flatten your back on the floor by squeezing your abdominal muscles and slightly bending your pelvis upward. Hold for up to several seconds. and Repeat
- Back extension in standing
- performing a standing lumbar extension to quickly get pressure off the spinal nerves and rapidly reverse symptoms.

- Lumbar flexion with rotation (trunk rotation)
- The rotating feature of this stretch improves spinal mobility. It allows for greater rotation and movement between the vertebrae, which can release the compressed nerve and contribute to a healthier and more functional spine
- Lumbar flexion in sitting and standing position
- bending forward will increase the mobility of the lumbar spine
- hip flexion-extension exercise
- hip flexion in supine lying and extension in prone lying.
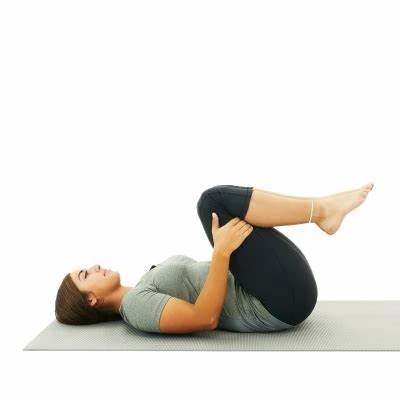
- Knee to chest
- this exercise will increase the strength of the lower back muscle and help to improve the full range of motion in both the pelvis and lower back vertebrae.
- this exercise loosens up any stiffness and improves posture
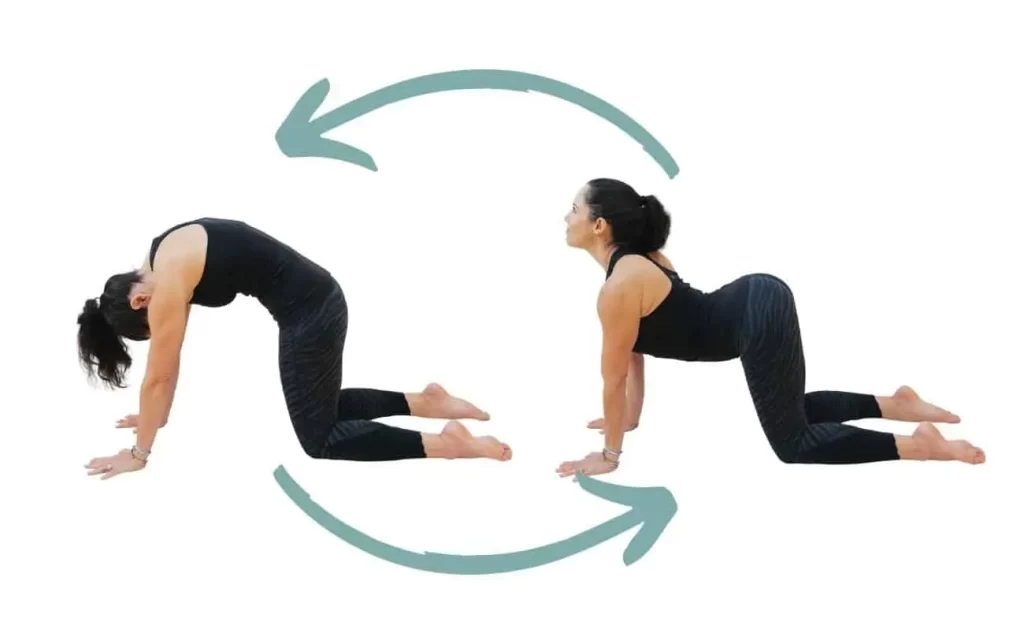
- Cat and cow
- The cat-cow is a mobilization of the lower back area, to bring proper movement into the lower back and pelvis.
Core strengthening exercise
- curl-ups
- Abdominal curl-ups or sit-ups to strengthen the rectus abdominis.

- Bridges
- Lie on your back, legs bent, feet flat on the floor, with your pelvis apart, Lift your hips off the floor.
- Hold for 10-20 seconds, then lower back down. Repeat 10-15 times

- Prone press up
- Increase the stability and strength of your erector spinal muscles. They also increase the range of motion in your lower back.

- Plank
- Plank variations (front plank, side plank) to engage abdominal and back muscles


Goals of exercise
- Reduce radicular pain rapidly (leg or arm discomfort caused by a pinched nerve in the spine).
- Restore spine mobility
- Restore body balance and improve spinal stability
- Learn to maintain a supported spinal posture
- Treat the underlying cause of pain in the spine
- Sustain activities longer
- To reduce the chance of repeated discomfort, avoid painful postures and actions.
Splints
- Lumbosacral orthosis (LSO) is a typical care for back discomfort.
- this splint will restrict the movement in the lumbar spine region and support the surrounding muscles during movement.
- which helps to reduce pain and swelling around the lower back region.
Flexibility and Stretching Exercises:
- Hamstring stretches to improve flexibility in the back of the thighs.
- Quadriceps stretches to relieve tension in the front of the thighs.
- Hip flexor stretches to reduce tightness in the hip muscles.
- Lumbar and thoracic spine stretches to promote mobility and relieve stiffness.
- Abductor stretch (Butterfly stretch) improves flexibility in the pelvic region.
- Iliotibial band stretch improves stability in the hip and knee.
Postural Correction and Ergonomic Training:
- Assess and correct posture during sitting, standing, and lifting activities to reduce strain on the spine.
- Guide ergonomic adjustments in workstations, chairs, and sleeping positions to maintain a neutral spine alignment.
Surgical Management
Surgical management for lumbar radiculopathy, also known as sciatica, is typically considered when conservative treatments like medications, physical therapy, and injections haven’t provided sufficient relief. Here are some common surgical options:
- Laminectomy: In this procedure, a portion of the bone above the nerve root and/or disc material from beneath the nerve root is removed to ease pressure on the impacted nerve.
- Artificial disc replacement: In cases where a disc is causing symptoms and needs to be removed, an artificial disc can be inserted to maintain normal motion and function of the spine.
- Microdiscectomy: This is a minimally invasive procedure where a small portion of the herniated disc that is pressing on the nerve root is removed.
- Foraminotomy: This procedure enlarges the space where the nerve exits the spinal canal, reducing pressure on the nerve root.
Do’s & Don’ts
Dos:
- Exercise Regularly: Engage in low-impact exercises like walking, swimming, or cycling to improve flexibility and strength in the lower back and core muscles.
- Maintain Good Posture: Pay attention to your posture while sitting, standing, and lifting objects to avoid putting excessive strain on your lower back.
- Use Proper Lifting Techniques: When lifting large things bend your knees while keeping your back straight, correct-sleeping-positions, weight-lifting
- Apply Heat or Cold Therapy: Use heat packs or cold packs to relieve pain and reduce inflammation in the affected area.
- Practice Relaxation Techniques: Incorporate relaxation techniques such as deep breathing, meditation, or yoga to manage stress, which can worsen pain.
- Stay Active: Avoid prolonged periods of inactivity or bed rest, as it can lead to muscle stiffness and weakness. Instead, stay active within your pain limits.
- Wear an Orthosis Belt: always wear an orthosis while driving or walking.
Don’ts:
- Avoid High-Impact Activities: Refrain from activities that involve repetitive bending, twisting, or high-impact movements that can exacerbate symptoms.
- Don’t Ignore Pain: Listen to your body and avoid pushing through severe pain or discomfort. Rest when needed and modify activities as necessary.
- Limit Prolonged Sitting: Minimize prolonged sitting or standing in one position. Take regular pauses to stretch and change postures.
- Avoid Heavy Lifting: Steer clear of lifting heavy objects or performing strenuous activities that strain your lower back muscles.
- Don’t Smoke: If you smoke, consider quitting, as smoking can impair blood flow to the spine and hinder healing.
- Don’t Self-Medicate: Avoid self-medicating with over-the-counter painkillers for prolonged periods without consulting a healthcare professional.
Summary
Lumbar radiculopathy discomfort is a common, self-limiting damage to the nerve roots of the lumbar spine. The illness affects millions of individuals and causes discomfort. Thus, a team of professionals is ideally suited to managing the disease.
Rarely, the disease can lead to serious problems such as spondylolisthesis and cauda equina syndrome. These problems frequently involve surgical intervention and modern imaging techniques.
Lumbar radiculopathy discomfort is a common, self-limiting damage to the nerve roots of the lumbar spine. The illness affects millions of individuals and causes Severe symptoms that must be treated quickly to avoid lasting damage, which can lead to a worse quality of life and higher medical expenses. As a result, it is critical to identify risk factors, conduct a complete examination of the patient with radicular pain, and monitor for the course of symptoms. A team effort is the best method to reduce the difficulties of such an accident.
The suggested initial step for patients experiencing lumbar radicular discomfort is to have their primary care doctors evaluate them for severe radiculopathy or warning signs When symptoms are minor or moderate, conservative treatment should begin, which may include slight exercise, stretches, and medication. A chemist should examine dose and undertake medication reconciliation to avoid interactions between medicines, and potential trust on particular pain drugs, and to notify the healthcare team of any issues.
- The patient should see a primary care physician one to two weeks after the first accident to assess the course of the nerve damage.
- If symptoms increase or significant radiculopathy is suspected, consider referral to neurosurgery or hospitalization for spinal decompression.
- If radicular problems remain three weeks following the accident, a physical therapy referral may be an option.
- When symptoms last more than six weeks, imaging tests such as an MRI or CT scan can help see the nerve roots.
- The patient should see a dietician and follow a healthy diet to maintain a healthy weight.
- The chemist should advise the patient to quit cigarette smoking since this might aid in the healing process. Furthermore, the chemist should educate the patient on pain treatment and easily available solutions.
- Continuous discomfort after six weeks may need a referral to interventional pain management or neurosurgery for an epidural steroid injection.
- If mild to severe symptoms persist three months after start, referral for surgical surgery should be considered.
FAQ
Why is lumbar radiculopathy worse at night?
Lying down puts a load on your sciatic nerve. This pressure might be increased if you have a soft mattress that encourages your spine to bend when sleeping.
What happens if you don’t treat lumbar radiculopathy?
The condition is caused by discomfort or injury to one of the spinal nerves going out of the spinal cord in the lower back. If ignored, untreated lumbar radiculopathy can injure the sciatic nerve.
What are the common symptoms of lumbar radiculopathy?
Common symptoms include sharp or shooting pain in the lower back, buttock, and leg, numbness or tingling sensations, weakness in the leg or foot, and difficulty with leg movements or walking.
Can lumbar radiculopathy be prevented?
While it may not be entirely preventable, maintaining a healthy weight, practicing good posture, avoiding activities that strain the back, and staying physically active can reduce the risk of developing lumbar radiculopathy.
What not to do with radiculopathy?
The following behaviors and habits may worsen lumbar radiculopathy:
Prolonged sitting.
Coughing and sneezing, place a sudden impact on the spine.
Twisting the spine (i.e. golf, gymnastics, some yoga poses)
High-impact exercise, including Running or jogging. Weightlifting
References
- Results Physiotherapy | Physical therapy for Lumbar Radiculopathy. (n.d.). https://www.resultspt.com/lumbar-radiculopathy
- Ocs, N. U. P. D. (n.d.). 7 McKenzie Method Exercises for back pain and sciatica. Spine-health. https://www.spine-health.com/wellness/exercise/7-mckenzie-method-exercises-back-pain-and-sciatica
- CMSadmin. (2023, November 24). Cat Camel Exercise | Transform Chiropractic. Transform Chiropractic. https://transformchiropractic.com/back-pain/cat-camel-exercise/
- Ben-Yishay, A., MD. (n.d.-c). Lumbar radiculopathy. Spine-health. https://www.spine-health.com/conditions/lower-back-pain/lumbar-radiculopathy
- Lumbar radiculopathy. (n.d.-d). Physiopedia. https://www.physio-pedia.com/Lumbar_Radiculopathy
- Alexander, C. E., Weisbrod, L. J., & Varacallo, M. (2024, February 27). Lumbosacral radiculopathy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK430837/
- Dydyk, A. M., Khan, M. Z., & Singh, P. (2022b, October 24). Radicular back pain. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK546593/
- Lumbar radiculopathy. (n.d.-e). www.aapmr.org. https://www.aapmr.org/about-physiatry/conditions-treatments/musculoskeletal-medicine/lumbar-radiculopathy
- School, M. M. (2022b, July 14). Lumbar Radiculopathy | UTHealth Neurosciences. Neurology, Neurosurgery, Spine Care | UTHealth Neurosciences. https://med.uth.edu/neurosciences/conditions-and-treatments/spine-disorders-and-back-pain/lumbar-radiculopathy/
- Abhishiek Sharma, MD, FAANS. (n.d.-b). 7 Treatments for lumbar radiculopathy: Atlas Neurosurgery and Spine Center: Neurosurgery. https://www.atlasneurosurgery.com/blog/7-treatments-for-lumbar-radiculopathy
- Apnp, P. V. (n.d.). Radiculopathy, radiculitis, and radicular pain. Spine-health. https://www.spine-health.com/conditions/spine-anatomy/radiculopathy-radiculitis-and-radicular-pain
- Sciatica Vancouver – Dr. Craig Best. (2023, September 22). Dr. Craig Best. https://www.drcraigbest.com/spine-neck-pain/lumbar-radiculopathy-vancouver/
- Ocs, N. U. P. D. (n.d.-b). What is the McKenzie method for back pain and neck pain? Spine-health. https://www.spine-health.com/wellness/exercise/what-mckenzie-method-back-pain-and-neck-pain