Fibula Bone
Introduction
The fibula is a long bone in the lower extremities that is part of the lateral side of the tibia. The fibula is significantly thinner than the tibia when compared. It starts at the knee joint and travels down the side of the leg to the ankle joint, which is situated right behind the tibial head.
The fibula is much thinner and smaller than the tibia, and it is positioned directly below the tibial head. It moves down the side of the leg until it reaches the ankle joint. At the medial surface of the fibula, where it connects to the tibia through the interosseous membrane, a ridge represents the interosseous boundary.
The two points on the interosseous membrane where they connect are known as the fibula and tibia. This boundary is the ridge seen on the medial side of the fibula. This connection has an extremely restricted range of motion for a syndesmotic joint.
The long fibula bone is divided into three sections:
- the upper end,
- the lower end
- intervening shaft.
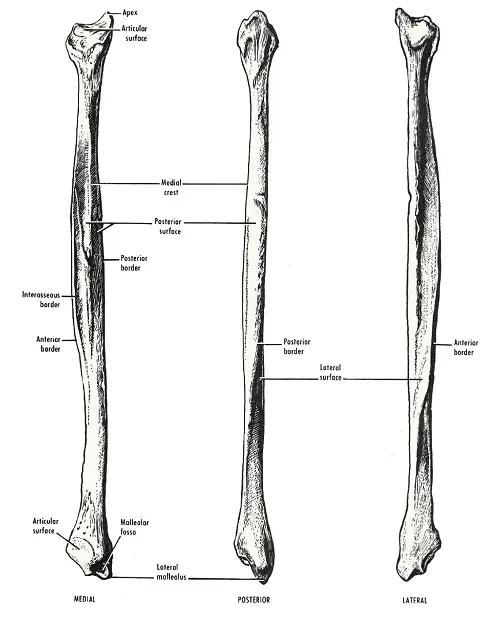
Fibular neck formation occurs as the head narrows distally. The fibular shaft has three surfaces:
- the lateral surface,
- medial surface, and
- posterior surfaces.
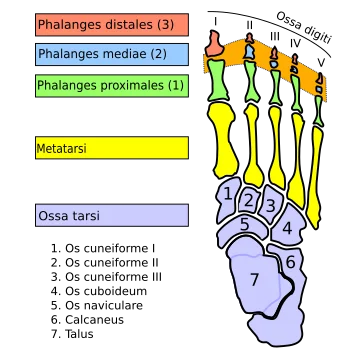
It is located distal to the neck. It has a triangle shape at first, but as it moves away, it becomes more asymmetrical. The lateral malleolus, which joins the lateral talus to form the lateral ankle, supplies the distal end of the fibula. The medial and posterior malleoli are produced by the connection between the lateral and posterior tibia.
Structure and Function
The ankle joint is supplied by support and is mostly used to connect to the tibia. Several grooves on the distal end of the fibula are intended for ligament attachments, which support and give leverage as the ankle moves.
The tibia and fibula can bear no weight. Its main function is to provide support to the ankle joint when the tibia is at work. Several grooves for ligament attachments on the distal end of the fibula provide support and leverage during ankle motions. The knee is stabilized are this ligament.
Development
The shaft and both ends form the upper fibula’s two centers. Around the eighth week of fetal life, the body swells osseously and moves toward the extremities. They have cartilaginous endings at birth.
The upper and lower epiphyses, which unite at around the age of twenty-fifth, are what make up the body. The lower epiphysis ossifies first.
Head
One part of the upper limb is the head of the fibula, which has a unique quadrate structure. It is positioned above a flattened articular surface that is pointed upward, forward, and medially for articulation with the tibia’s lateral condyle.
The prominence serves as an attachment point for the biceps femoris tendon in both its upper and lateral portions. It also provides the connection to the knee joint’s fibular collateral ligament, which separates the tendon into two sections.
There are rough spots where muscles and ligaments follow the remaining borders of the skull. It has two tubercles: one behind the attachment site of the posterior ligament of the head and the top soleus fibers, and one in front that acts as the anterior and upper peroneus longus fibers.
Body
Three main components make up the fibula’s body:
the anterior, posterior, medial, and lateral surfaces; the antero-lateral, antero-medial, postero-lateral, and postero-medial borders.
The anterolateral boundary starts above the head, descends vertically to just below the center of the bone, then curves slightly laterally before bifurcating to enclose a triangular subcutaneous surface just above the lateral malleolus. The extensor muscles on the anterior leg surface and the peronaei longus and brevis on the lateral surface are divided by an intermuscular septum, which is attached to this boundary.
The flexor muscles on the posterior surface and the peronaei on the lateral side are divided by an aponeurosis, to which it provides connection. It is directed considerably medial-ward below, rearward in the center of its length, and lateralward above.
The posteromedial border, also known as the oblique line, begins at the medial side of the skull and ends at the bottom fourth of the bone, where it joins the interosseous crest. It is prominent and can be seen in the upper and central parts of the bone. It provides a connection to an aponeurosis that divides the flexor hallucis longus and soleus from the tibialis posterior.
Joints
The three joints involved in articulating the tibia and fibula are the superior, middle, and inferior tibiofibular joints.
The particular tissue known as the interosseous membrane also called the middle tibiofibular ligament, facilitates the articulation of the tibia and fibula. It consists mainly up of aponeurotic lamina that connects to the oblique fibers. The tibial interosseous border is the fibular interosseous border at the ligament’s lateral and medial side attachment. Between the muscles in the front and back of the leg is a membrane.
It is made up of a thin layer of the aponeurotic membrane that has been continuously moving. The fibula structure is the medial, lateral, and posterior surfaces. It begins as a triangle and gradually becomes more asymmetrical. The distal end of the fibula generates the lateral ankle component through the malleolus’s articulation with the lateral talus.
Blood supply and Lymphatics
The blood vessels that provide the blood supply to the lateral compartment of the lower leg’s back are the fibular and peroneal arteries. The tibia and fibula’s trunk contain it. Located in the posterior region of the lower leg arteries is the fibular artery’s largest branch.
Blood needs passage through the fibular artery to reach the periosteum and the surrounding bones. The following minor branches make up its composition. Fibula transplantation for mandibular repair is improved by knowledge of the blood flow in the fibula.
A branch of the fibular artery can pass through the bone if the foramen connected to the posterior side of the fibula is in good shape.
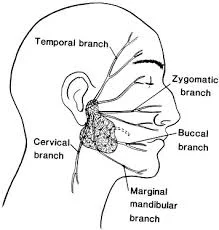
The common fibular nerve’s genicular branch supplies the knee, though the deep fibular nerve supplies the ankle. The proximal and distal ends of the fibula are innervated by these types of nerves. The nervous system of the fibular periosteum is supplied by superficial and deep fibular nerves, in a manner akin to the nervous system of the muscles located nearby.
Nerve supply
The superficial fibular (peroneal) nerve provides sensation to the anterolateral leg and supplies the muscles of the lateral compartment of the leg. However, the deep fibular (peroneal) nerve is the main nerve supply to the dorsum of the foot and the muscles of the anterior compartment of the leg.
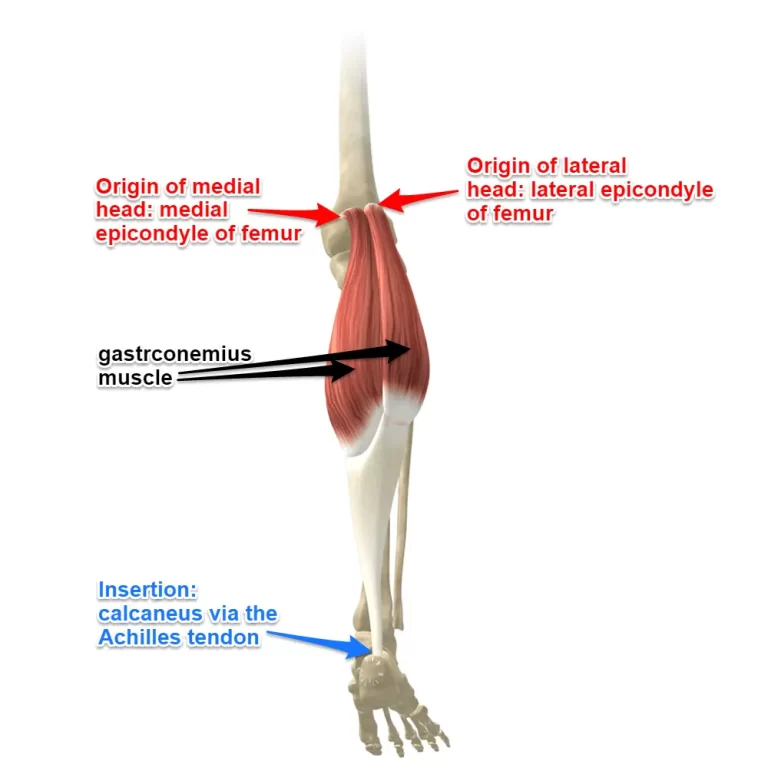
It proceeds in the opposite direction, through the medial border of the biceps femoris and then through the lateral head of the gastrocnemius. The lower limb’s lateral compartment borders comprise the fibula’s lateral surface, deep fascia, and intermuscular septum. This compartment contains the superficial fibular nerve and controls plantar flexion and eversion. The fibula’s rear surface, deep fascia, and interosseous membrane constitute the lower limb’s posterior compartment and border compartment and are used by the tibial nerve, which regulates digit and plantar flexion. The medial surface of the fibula forms a partial border with the lower limb’s anterior compartment.
The calcaneus bone’s lateral and posterior parts, the soleus muscle, and the foot’s deep tissues are all points of entry for blood.
Muscle
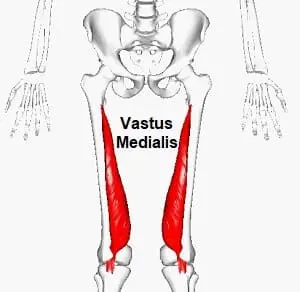
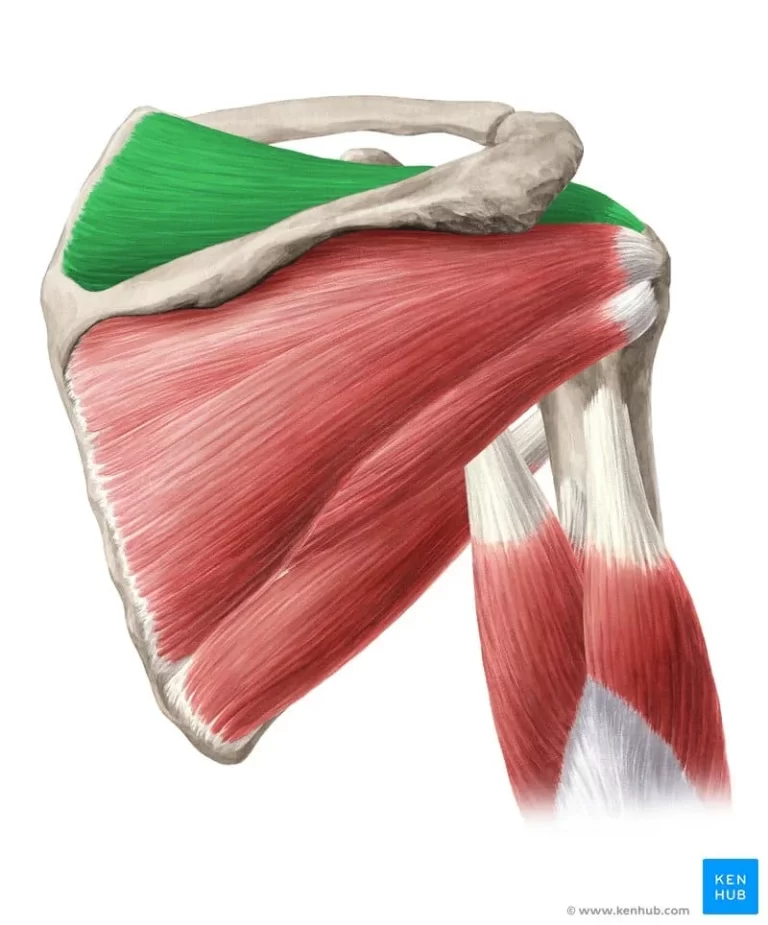
The fibular shaft gets its distinctive form from fibula attachment locations with many main muscles.
The attaches to the medial fibula are the origin of the Extensor digitorum longus (EDL) and Extensor hallucis longus (EHL) muscles.
The extensor digitorum longus ends are known as the superior medial border.
The muscle called the Fibularis Tertius will enable it to connect to the smallest areas of the front surface.
The lower two-thirds of the posterior surface is referred to as the (FHL) flexor hallucis longus.
The part of the posterior surface where the tibialis posterior gets its origin is situated between the medial crest and the interosseus boundary.
The deep transverse facial septum is given thought at the posterior border.
Surgical Importance
The best option for mandibular repair is a fibula bone transplant. The tibia is primarily responsible for supporting weight; therefore, moving the fibula out of its natural alignment will not significantly affect it.
Clinical Importance
Congenitally
Fibular shaft length is an effective measure for determining newborn bone age, and recent studies strongly support its usage. This could be a more accurate alternative to conventional ways of assessing newborn bone age, such as counting ossification centers or watching hand, wrist, or knee radiographs.
The most common pattern in the lower bones is the fibular hypoplasia-aplasia, also known as fibular bone hemimelia. This causes the fibula to be absent in part or completely. This is commonly identified at birth when a limb-length difference and a lack of digits are discovered.
Neurologically
The fibula’s proximal end has a slightly enlarged prominence with a facet articulating with the tibia’s lateral condyle. The common peroneal nerve’s contents are known by an individual name. It may become stuck when it passes near the fibular head, experiences trauma, or is directly injured. The neuropathy that affects the lower limbs most frequently is called the most common fibular nerve-entrapment neuropathy. Although lateral limb sensory deficits and foot drop are potential indicators, misdiagnosis due to the condition’s high incidence may postpone treatment.
Fractures
When the biceps femoris muscle contracts suddenly, the fibula may suffer an avulsion fracture. The biceps femoris tendon is where the fibula is connected, which means that it may become very tight.
The point of origin on the lateral malleolus is known as the distal fibula. When the ankle is forcefully twisted externally, the lateral side’s distal fibula might also break. Direct trauma, foot eversion, or outward twisting all result in a distinct sort of damage. Transverse fibula fractures and eversion injuries are the most common injuries. Use a clinical decision-making tool such as the Ottawa Ankle Rules if you suspect lateral malleolar injury.
Compartment syndrome is usually caused by fibular fractures. The risk of compartment syndrome increases in cases where there is both a tibial plain fracture and a fibular fracture.
History
Etymology
The smaller bone in the lower leg was referred to as the “fibula” in English for the first time in around 1706; it was first used to refer to a clasp or brooch (see fibula). It comes from the Latin word fībula, which also indicates a brooch and clasp. The reason the bone got its name was that it looked like a modern defense pin clasp.
FAQs
Can you walk with a broken fibula?
Since the fibula does not support weight, your doctor may decide to let you walk while your injury heals if you have an isolated fibula fracture. This is comparable, in certain circumstances, to having a major ankle sprain.
Is a broken fibula serious?
A fracture of the tibia and fibula is a dangerous injury that has to be treated very quickly. With timely medical intervention, a fractured tibia-fibula can be entirely healed.
Can you replace a fibula?
A fibula-free flap is frequently utilized in reconstructive surgery to replace lost soft tissue and bone. This treatment is frequently employed in mandibular or maxillofacial repair after trauma, cancer excision, or congenital malformations.
How do I fix a broken fibula?
Crutches, a walking boot, or a brace may be suggested in the majority of fibular fracture situations to immobilize your lower leg. Whether your injury was repaired surgically or you can heal quickly and fully at home, physical therapy, stretching, and consistent exercises to strengthen the affected area are advised.
Can a fibula heal without surgery?
The surgical reconstruction of the fibula has been demonstrated to be accelerated by returning normal ankle function as soon as feasible.
How can I make my fibula heal faster?
Fibula bone regeneration is accelerated when the injured ankle is allowed to walk normally as soon as possible.
What is the best medicine for broken bones?
Anabolic drugs facilitate the growth of new bone and speed up the healing process for nonunion and acute fractures. A synthetic type of parathyroid hormone called teriparatide is one of these medications. It may speed up the healing process by increasing blood calcium levels and stimulating the formation of new bone tissue.
Can we eat curd in a fracture?
Because it is the primary component of bone, calcium can be found in milk, among other items, yogurt, sea vegetables, and green leafy vegetables. To restore muscles, you need protein. Consumption of meals rich in clean, lean protein, such as the seafood taken in the wild and grass-fed cattle, will thus help hasten the body’s recuperation.
Can you walk without a fibula?
The fibular bone connects the knee and ankle joints on the outside of the leg. It’s a tiny, delicate bone that can be mostly removed without impairing your capacity to walk or carry weight.
References
- Gupton, M., Munjal, A., & Kang, M. (2023b, May 23). Anatomy, Bony Pelvis, and Lower Limb: Fibula. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470591/

2 Comments