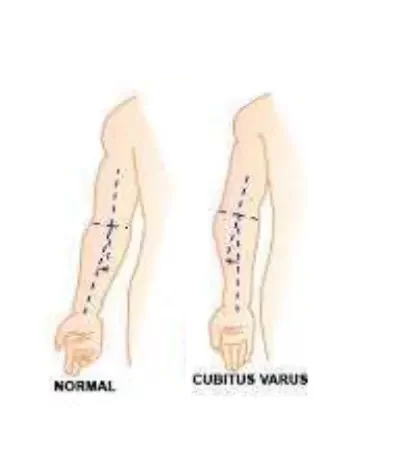
Cubitus Varus Deformity
Definition for Cubitus Varus Deformity
Cubitus varus deformity, often referred to as “gunstock deformity,” is a condition characterized by an inward angulation of the extended elbow. This deformity typically arises as a complication following supracondylar fractures of the humerus, particularly in children.
Cubitus valgus is the “opposite” condition.
This is a trilobate asymmetry of the elbow, with internal rotation in the transverse plane, sagittal plane extension, and coronal plane varus angulation.
The pediatric population lacks well-established guidelines on the timing of surgery and the indications for corrective osteotomy. Historically, pediatric cubitus varus has been viewed as a cosmetic issue with minimal to no functional impairments or pain.
While cubitus varus after a pediatric distal humerus fracture or congenital deformity is well documented in the adult orthopedic literature, it can also result in adult elbow joint asymmetry, snapping triceps, ulnar neuropathy, progressive varus of the ulna, and posterolateral rotatory instability (PLRI). While there may be some changes to the arc of motion, such as greater hyperextension and decreased elbow flexion, children with cubitus varus usually have minimal loss of mobility.
Cubitus varus deformity has been linked to an increased risk of lateral condyle fractures. The very young, skeletally immature elbow may be remodeled to regain the lost flexion. Unlike in children, adults with cubitus varus usually complain of recurring instability and lateral elbow pain as symptoms, which do not show up until decades after the cubitus varus first develops.
What is Cubitus Varus Deformity?
A disease known as cubitus varus deformity causes the hand to curve inward as the forearm is flexed toward the body. This may happen as a result of an accident, problems with bone growth, or congenital abnormalities. Physical therapy and surgery are among the available treatment options, contingent on the severity of the disease.
- The most frequent side effect after a supracondylar humerus fracture is cubitus varus.
- Cubitus varus was formerly believed to be caused by a disruption in the development of the distal humeral epiphysis.
- Cubitus varus results in a little functional disadvantage but a cosmetic abnormality.
- A tiny degree of anterior or posterior angulation or medial or lateral displacement may be allowed during reduction, but malrotation of any kind is not.
- Verification of rotation is done under fluoro using oblique, lateral, and AP views.
- Soft-tissue interposition may require open reduction if reduction is not achieved.
- The supracondylar fracture of the humerus is one of the most well-known and frequently occurring injuries in the pediatric age group. It typically results from a fall on an outstretched hand and accounts for 16% of all pediatric fractures and 60% of all pediatric elbow fractures. Men are more likely to sustain this injury than women.
- Because they affect neurovascular structures, the immediate consequences can be fatal and pose a hazard to limbs, while the late complications pose a significant risk to the patient’s functional status.
- All of these factors require stringent attention to detail and appropriate management procedures. In the pediatric age range, the majority of cases (90%) have presentations between the ages of 5-7. More injuries are of the extension kind than the flexion type. It usually occurs in the extremity that is not dominating. This form of flexion is typical in older kids. According to certain research, this patient category had an incidence of open fractures of up to 30%.
Anatomy Of Cubitus Varus Deformity
Bone
In children, the distal humerus has a weak, thin bone that makes up the supracondylar area.
The olecranon fossa borders this region from the back, the coronoid fossa borders it from the front, and the corresponding supracondylar ridges border it on both sides.
The condyles and epicondyles that result from the medial and lateral supracondylar ridges, respectively. The carrying angle of the trochlea is typically 4° valgus in males and 8° valgus in females.
Soft tissue structures
The connection of different muscles that cause the distal segment to rotate and move is derived from the supracondylar ridges, condyles, and epicondyles.
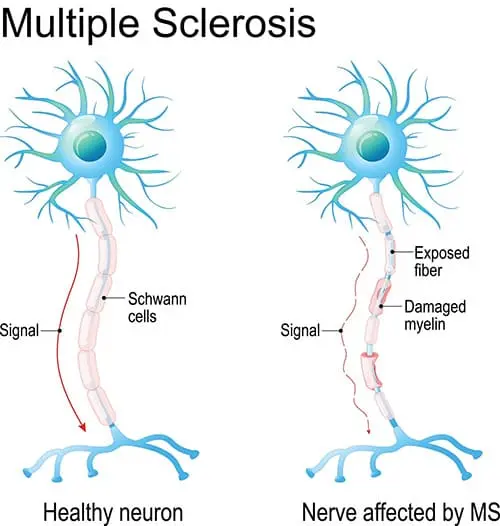
Neural structures are located close to the supracondylar area.
The brachial artery, which is frequently implicated in supracondylar humeral fractures, is located superficially to the brachialis muscle along the anteromedial portion of the distal humerus.
The supracondylar area and the major upper limb neurological structures—the median, radial, and ulnar nerves—are closely related.
Epidemiology
Although it happens seldom, congenital cubitus varus is not likely to be the origin of the malformation. The cause is humeral epiphyseal dysplasia, a condition in which the elbow joint’s carrying angle is reduced when the epiphysis angulates toward the midline. In the twelfth week of pregnancy, the distal humeral epiphysis occurs, marking the beginning of the ossification of the elbow joint. Epiphyseal dysplasia will cause congenital cubitus varus throughout this window of time.
Patho-Anatomy

The lateral ulnar collateral ligament and ulnar supination may eventually attenuate due to the medial deviation of the upper extremity mechanical axis and the medially directed triceps force vector associated with this deformity, resulting in symptomatic elbow PLRI (Posterolateral rotatory instability). Although the arc of elbow motion is changed with greater hyperextension and decreased flexion, bone remodeling in the axis of the elbow joint in immature children frequently recovers elbow flexion. On the other hand, the rotational component of the deformity shows minimal remodeling and, consequently, repair. These patients may also have limited pronation range of motion.
Radial head overgrowth, capitellar, and posterior trochlear malunion are among the pathoanatomic characteristics caused by internal rotation malunion of the distal humerus. Secondary adaptive modifications resulting from these basic defects include a lateral shift in the convexity of the trochlear notch and an enlarged anteroposterior trochlear articular arc. Moreover, the ulna increases its varus, flexion, and external rotation in response to a distal and medial placement. Additionally, internal rotation malunion of the distal humerus, concurrent fibrosis, and entrapment in the cubital tunnel can result in ulnar nerve instability and delayed ulnar nerve palsy.
The ulnar nerve neuropathy symptoms are caused by the nerve becoming caught in the fibrous bands of the flexor carpi ulnaris muscle, where it may sublux or even dislocate anterior to the medial humeral epicondyle.
Biomechanics:
The upper extremity’s mechanical axis is displaced medially as a result of varas asymmetry.
The lateral collateral ligament complex undergoes higher tensile stresses and attenuation due to recurrent varus forces on the elbow from everyday activities, such as pulling up from a sitting posture. This causes greater medial displacement of the mechanical axis.
Even in the presence of an intact LUCL, a biomechanical study showed that increasing cubitus varus deformity did in fact cause higher LUCL strain and increased ulno-humeral widening.
In the cubitus varus, the triceps is moved medially. This displacement of the triceps force vector causes the ulna to rotate externally, or supinate.
The first stage of PLRI is caused by persistent medial triceps pressures on the olecranon, which elongates the olecranon and causes the ulna to rotate externally.
With severe PLRI, both of these biomechanical alterations ultimately result in radial head subluxation and dislocation. They also result in olecranon external rotation and sustained LUCL reduction.
Morphology:
- Elbows with cubitus varus do really experience morphological alterations in the elbow joint, as confirmed by three-dimensional computed tomography scans. Elbows with cubitus varus exhibit trochlear overgrowth posteriorly as compared to the contralateral, undamaged elbow. This results in greater internal rotation of the posterior joint line of the distal humerus.
- With a longer articular surface extending from anterior to posterior and a lateral displacement of the convex portion of the trochlear notch, the proximal ulna accommodates the trochlear overgrowth.
- In comparison to the contralateral ulna, the ulna moves to a more distal and medial position and experiences more external rotation and flexion.
- Also, the diameter of the radial head increases, and the lateral side of the capitellum overgrows distally, but not to the point where this results in an increase in cubitus varus.
- These bone morphological abnormalities are thought to be caused by the medial overpull of the triceps, while it’s also plausible that this is a result of physical damage to the elbow.
- There have also been reports of cubitus varus and tardy ulnar nerve palsy with anterior displacement of the nerve. The location and stability of the nerve are hypothesized to be impacted by the internal rotation deformity of the distal humerus, distal fibrosis, and nerve entrapment; in these situations, ulnar nerve transposition is advised in addition to corrective osteotomy.
- Similar to this, internal rotation of the distal humerus and medial displacement of the triceps can both result in the medial section of the triceps breaking.
Causes of Cubitus Varus Deformity:
In the past, up to 30% of patients with supracondylar humerus fractures experienced this deformity. Nonetheless, since these injuries are now treated surgically, the incidence has significantly dropped. This can happen less often following lateral condyle humeral fractures. Other reasons include infections, osteonecrosis, physis traumas, and Rarely, malignant illnesses.
Differential Diagnosis
Malunited supracondylar fractures are the typical cause of the cubitus varus. The differential includes distal humerus physis damage, trochlear osteonecrosis, and varus deformity resulting from prior lateral condyle fractures.
Diagnosis:
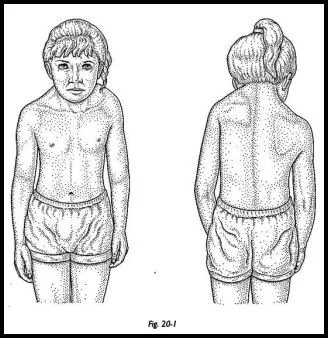
History and Physical
A patient with cubitus varus deformity requires a comprehensive history and physical examination. On the first visit, it is important to check for open wounds, stiffness, range of motion, scarring, and a thorough neurovascular examination. During a physical examination, rotational asymmetry is assessed by comparing the shoulder passive internal rotation in the extension of the implicated and uninvolved extremities. When a child’s deformity worsens, radiographs must be critically analyzed, and further axial imaging is necessary to see whether there are any anomalies in the child’s asymmetrical development.
The cubitus varus deformity is often identified six to ten weeks following the healing of the fracture and the restoration of full elbow range of motion. The elbow’s unattractive look is mostly caused by varus angulation, however, any amount of posterior angulation or flexion contracture lessens the deformity’s outward appearance. Torsional malrotation makes the deformity look more pronounced. When left untreated, varus angulation usually stays constant and seldom ever becomes worse over time. The distal humeral physis may progress with an asymmetric growth disruption. Cubitus varus can cause posterolateral rotatory instability due to attenuation of the LUCL and ulnar nerve entrapment if left untreated or if the condition is severe enough. Occasionally, following surgical repair, PLRI is revealed.
Evaluation
To determine the degree of deformity and calculate the humeral-elbow-wrist angles, full-length anterior-posterior radiographs (AP) of the damaged and contralateral upper extremities are crucial. The most precise way to figure out the right carrying angle is via the HEW angle. If the extremity position is valgus, a HEW angulation is shown with a (+) sign; otherwise, a varus angle is shown with a (-) sign. This method is preferred over Baumann’s angle as it may be applied to both adult and skeletally immature populations.
A fair approximation of the HEW angle can be obtained in the absence of lengthy radiographs by measuring the angle subtended between the center of the elbow, the center of the shaft, and the center of the transverse diameter of the radius and ulna bone. Osteotomies should aim to restore the HEW angle as near to the undamaged contralateral extremity as feasible, with the needed correction determined by the angle difference between the two extremities. The pre-operative AP radiographs of the affected extremity are also used to compute the lateral condylar prominence index.
The proportion of the distal humerus’s overall width that represents the difference between the lateral and medial widths measured from the mid-humeral axis. A true lateral elbow radiograph can be used to assess the extent of the deformity. On paper, affected and unaffected extremities radiographs are traced to calculate the wedge width required for surgical repair. For the dome osteotomy correction approach, a similar method is used to calculate the necessary rotation.
A cubitus varus deformity’s severity is ranked as follows:
- Grade I: Physiologic valgus loss
- Grade II: 0 to 10 degree varus
- Grade III: 11 to 20 degree varus
- Grade IV: Varus > 20 degrees
Physical Examination:

A patient with cubitus varus deformity requires a comprehensive history and physical examination. On the first visit, it is important to check for open wounds, stiffness, range of motion, scarring, and a thorough neurovascular examination.
During a physical examination, variations in shoulder passive internal rotation in extension between the implicated and uninvolved extremities are assessed to identify rotational asymmetry. When a child’s deformity worsens, radiographs must be critically analyzed, and further axial imaging is necessary to see whether there are any anomalies in the child’s asymmetrical development.
Six to ten weeks after the fracture heals and the full elbow range of motion is restored, cubitus varus deformity is typically identified. The elbow’s unattractive look is mostly caused by varus angulation, however, any amount of posterior angulation or flexion contracture lessens the deformity’s outward appearance. Torsional malrotation makes the deformity look more pronounced. When left untreated, varus angulation usually stays constant and seldom ever becomes worse over time.
The distal humeral physis may progress with an asymmetric growth disruption. Cubitus varus can cause posterolateral rotatory instability due to attenuation of the LUCL and ulnar nerve entrapment if left untreated or if the condition is severe enough. Occasionally, following surgical repair, PLRI is revealed.
Treatment of Cubitus Varus Deformity:
Medical Treatment
Medical treatments are primarily symptomatic; for example, doctors would typically prescribe NSAIDS if there is joint pain and swelling.
Physical Therapy Treatment:
Corrective elbow mobility exercises, strengthening of weak muscles, and stretching of tight muscles surrounding the elbows are the main goals of physical therapy treatments.
- to fully and painlessly mobilize the elbow joint.
- to speed up the healing process.
- to make affected muscles stronger.
- to enhance children’s general functioning abilities.
Cubitus varus exercises:
- Stretching exercise: Following an evaluation, the deformity can be corrected by doing appropriate stretching exercises on the tight muscles surrounding the elbow.
- Strengthening Exercise: Strengthening exercises for weak muscles also aid in preserving the elbow’s natural shape and correcting the deformity overall.
- Exercises for elbow mobilization assist to rectify deformities and reduce stiffness in the joints.
- Splints or Corrective Orthosis for Cubitus Varus:
- Electrotherapeutic methods such as TENS, ULTRASOUND, PARAFFIN WAX BATH (pain alleviation and extensibility), and faradism under pressure for deformity repair were chosen as therapy options.
The following outcome metrics can be used to compare and assess how well a therapy is working:
- Faces and the Numerical Pain Rating Scale (NPRS) Pain Measure
- Motion range: Goniometry
- Muscle testing by hand (MMT)
Cubitus varus surgery:
There are several documented methods for cubitus varus correction:
- the lateral closing wedge osteotomy.
- step-cut osteotomy.
- dome osteotomy.
- external fixation with distraction osteogenesis.
- computer-aided multi-planar osteotomy.
Cubitus varus osteotomy:
The best method for decreasing cubitus varus deformity symptoms and recurrence is a corrective osteotomy of the distal humerus. The purpose of the osteotomy is to make the elbow joint stable and realign it within the usual range of 5 to 15 degrees. Many osteotomy procedures have been documented for surgical correction: step cut, multiplanar, dome, double dome, straight and oblique lateral closure wedge, reverse V, triangle, external fixation with distraction osteogenesis, and so on.
But no method is more effective or safer than another. Furthermore, since the degree of uncorrected torsional deformity did not affect the carrying angle in one investigation, it is unclear if correcting axial rotational malunion is required to provide superior results. This finding is significant because axial derotation correction techniques frequently result in decreased cortical contact at the osteotomy site, making the site unstable. Uncorrected rotational malunion following corrective osteotomy may have uncertain long-term effects. Since hardware prominence is prevalent in this age range, pins, screws, staples, and tension band structures with wires are usually employed for internal fixation of the osteotomy in the pediatric population.
Furthermore, since the degree of uncorrected torsional deformity did not affect the carrying angle in one investigation, it is unclear if correcting axial rotational malunion is required to provide superior results. This finding is significant because axial derotation correction techniques frequently result in decreased cortical contact at the osteotomy site, making the site unstable. Uncorrected rotational malunion following corrective osteotomy may have uncertain long-term effects. Since hardware prominence is prevalent in this age range, pins, screws, staples, and tension band structures with wires are usually employed for internal fixation of the osteotomy in the pediatric population.
According to a recent pediatric study, external fixation was less expensive than internal fixation devices, made preoperative planning simpler, and made removal during the recovery phase easier. But in adults, and often in teenagers as well, medial and lateral column plates are considered essential for secure fixation and early mobility to reduce stiffness. Insecure internal fixation, particularly in the adult population, might allow the osteotomy to wander into a varus position, which can result in a poor esthetic outcome and recurrence.
While the expense of creating these templates is still an issue, several writers have recently employed 3-D printed cutting guides to expedite and simplify the process of correcting the three-dimensional malformation. Lateral ulnar collateral ligament reconstruction may be required as an adjuvant operation to address posterior locus of inhibition (PLRI) in individuals with long-standing deformities. For kids or teenagers, this is rarely essential, though.
While there is no suggestion for the type of osteotomy to be used, young patients may find the more intricate three-dimensional adjustments to be technically more difficult than adult patients. The authors of a meta-analysis comparing four distinct corrective osteotomies found no procedure to be safer or more successful. The medial side of the humeral metaphysis is lengthened by medial open wedge osteotomy, which may result in ulnar nerve stretching and an increased risk of persistent pain and delayed ulnar nerve palsy.
The most often used method is lateral closing wedge osteotomy (LCWO). In comparison to more challenging tri-planar corrective osteotomies, it is a less technically demanding treatment, and some published series have shown reduced complication rates. Yet, a typical issue with this treatment is lateral condylar prominence leading to a “pseudocubitus varus” deformity, which is correlated with the degree of the preoperative abnormality. On occasion, unsightly scarring on the elbow’s lateral side might also be an issue. According to several experts, the incidence of lateral condylar prominence may be reduced by using an oblique lateral closure wedge.
Some writers contend that when children under the age of 12 have osteotomy, remodeling of the lateral prominence and hyperextension takes place. Furthermore, keeping the medial side osteoperiosteal hinge joint intact is essential to this method since its loss during healing might result in under-correction and a return of the deformity.
The advantages of the step-cut and reverse step-cut procedures, which are also widely used, are their greater surface area and inherent stability.
The rotational component of the cubitus varus deformity can be corrected with multiplanar osteotomy. That being said, this is a technically difficult process. A CT scan may be necessary for preoperative planning in order to create a three-dimensional model of the damaged and unaffected arms.
The dome osteotomy is regarded as a difficult technique to perform. However, lateral condylar prominence is avoided with this technique. To reduce post-operative stiffness, it can also be done using a participial technique that spares muscles. Convexity is used during the osteotomy procedure with respect to the proximal shaft. After that, the distal portion is rotated to make the necessary adjustments.
Because of the osteotomy’s vast surface area, uneventful recovery is frequent. Rotating the distal component is difficult, though. Furthermore, this may result in ulnar nerve stretching. Recently, a double-dome osteotomy modification was devised, which avoids extending the neural structures and allows for simpler rotation correction from the deformity’s core. The benefit of this surgery is that, like the multiplanar osteotomy, it addresses the rotational component of the cubitus varus. Overcorrection and temporary radial nerve palsy are two risks associated with this procedure.
Distraction osteogenesis is a method that uses traction to gradually extend the osteotomy site in order to create bone. Cubitus varus was treated using this technique on the ulna. Distraction osteogenesis consistently exhibits lower rates of corrective loss than other osteotomy methods.
Advice and Exercises for the Immobilization Period:
- Since the elbow is often immobilized for three weeks, it is important to keep the nearby joints—the shoulder, wrist, and hand—actively moving or to perform active-assisted exercises often throughout the day.
- It is improper to move the elbow and appropriate to wear an arm sling.
- It is important to teach postural training, which entails sitting up straight, releasing your shoulders, and retracting your scapula.
1-2 Weeks After Removal of Cast:
- Joint stiffness can be reduced by hot fermentation.
- The musculature of the arm and forearm can be released gently using soft tissue techniques.
- Use a wand to gently guide you through active and active-assisted activities that are pain-free, often many times a day.
- Arms and forearm muscles can be strengthened using isometric exercises.
- Teach parents and kids to perform regular tasks including eating, writing, grooming, and dressing with the affected hand.
- Keep away from pushing and weightlifting activities.
Suggestions and Activities Following a 2-Week Cast Removal:
- Exercises for strengthening and range of motion should be progressive and engaging.
- such as passing a ball or putting on and taking off clothing.
Postoperative Rehabilitation
The type of corrective treatment chosen determines the postoperative care. After receiving a posterior above-elbow splint for two to three weeks, active range-of-motion exercises are administered. Depending on how well the wound is healing, the K wires are taken out after four to six weeks.
Prognosis:
The cubitus varus does not cause functional loss if left untreated. Corrective osteotomy is mostly justified for cosmetic reasons. However, surgery is necessary when there is a long-standing deformity along with concurrent clinical symptoms of instability and ulnar neuropathy.
Complications
There have been reports of up to 15% of these treatments’ complications including ulnar and radial nerve injuries, lateral condylar prominence, infection, stiffness, scarring, and under- or overcorrection. Approximately 75% of nerve injuries are considered to be temporary and have been linked to the posterior approach.
Healthcare Team:
Cubitus varus is treated collaboratively by pediatric orthopedists, radiologists, and physical therapists. Orthopedic surgeons are the primary healthcare providers, and it is expected that they have experience in corrective osteotomy procedures. The nursing staff in the orthopedics specialization is vital. Physical therapists aid in the restoration of range of motion after surgery.
FAQs:
A varus test: what is it?
The gold standard test to use for evaluating posterolateral instability of the knee is the varus stress test at 20–30° of knee flexion. The fibular collateral ligament’s function is isolated in this test.
How is cubitus varus fixed?
One typical method of cubitus varus correction is a supracondylar humeral osteotomy. We postulated that children with this deformity may benefit from a progressive correction using lateral distal humeral hemiepiphysiodesis (LDHH).
Which type of cubitus varus osteotomy is this?
The deformity known as cubitus varus needs to be surgically corrected in order to prevent more fractures, lateral instability, and nerve palsies, among other problems. One effective way to treat the deformity is with a lateral closed wedge osteotomy. Reduction of problems can be achieved by using a plate and screw for appropriate stabilization.
What is the cubitus varus pathophysiology?
Pathology. This deformity is caused by a supracondylar fracture that is not aligned properly. One cause of varus position is the collapse of the medial column due to comminution. It may also arise from the distal shattered fragment’s internal rotation and extension.
Can physical activity treat cubitus valgus?
Yes, it can be cured with exercise. To further safeguard the elbow, you should wear an elbow brace since the valgus deformity will force you to Overextend your elbows will cause your muscles to become hyperextended.
How is varus deformity treated?
A high tibial osteotomy is the most common surgical procedure used to treat varus knee without severe osteoarthritis, especially in younger patients. Through cutting into the bone and rearranging it, this technique realigns the tibia. This relieves the pressure that an incorrect tibiofemoral position has been exerting on your knee.
How are valgus and cubitus varus treated?
One of two treatments is often used to cure cubitus valgus: osteotomy or fixation. During an osteotomy, your doctor makes incisions in the bone to change its position and reshape it. Distraction osteogenesis, a specific kind of osteotomy, has been used to treat children’s cubitus valgus.
What other name would you propose for Cubitus varus?
A typical outcome of malunion of the supracondylar fracture is cubitus varus, sometimes referred to as “gunstock deformity.” This elbow asymmetry is trilobate, characterized by internal rotation in the transverse plane, sagittal plane extension, and varus angulation in the coronal plane.
What alternative name would you give Cubitus varus?
A common result of supracondylar fracture malunion is cubitus varus, sometimes known as “gunstock deformity.” This is a trilobate asymmetry of the elbow, with internal rotation in the transverse plane, sagittal plane extension, and coronal plane varus angulation.
What is the cubitus varus normal range?
The best method for decreasing cubitus varus deformity symptoms and recurrence is a corrective osteotomy of the distal humerus. The purpose of the osteotomy is to make the elbow joint stable and realign it within the usual range of 5 to 15 degrees.
Does cubitus varus harm?
Having cubitus varus might make it difficult to carry out daily duties. For example, carrying goods may cause pain and weakness in the arm that is affected. Cubitus varus can be treated with bracing, surgery, or physical therapy.
What is the cubitus varus carrying angle?
A girl’s carrying angle is greater than a boy’s, with an average of 6°–14°. Cubitus varus deformity is caused by any decrease in the elbow’s natural carrying angle. The most frequent reason for this deformity is a late consequence of a humerus supracondylar fracture.
Cubitus varus involves which nerve?
In cubitus varus, the triceps muscle actively pulls and compresses the ulnar nerve during elbow flexion, resulting in neuropathy.
What is the cubitus varus treatment?
Surgical correction of the cubitus varus deformity is necessary to prevent consequences such as lateral instability, nerve palsies, and eventual fractures. Lateral closed wedge osteotomy is a suitable alternative to correct the deformity. Appropriate stabilization—ideally with a plate and screw—will lead to fewer difficulties.
What differentiates valgus from cubitus varus?
Whereas the distal portion of the forearm deviated medially in cubitus varus deformity, it deviated laterally in cubitus valgus deformity.
Why does one develop cubitus varus?
The cubitus varus, sometimes referred to as the gunstock deformity or bow elbow, is caused by malunion, which results from a supracondylar humeral fracture. It causes only the extension type of humeral supracondylar fracture to lose or reduce its carrying angle.
What is a varus cubitus?
Cubitus varus is a consequence of a malunited supracondylar fracture. The tri-planar deformity is composed of the varus, hyperextension, and internal rotation components. In addition to ulnar nerve involvement and instability symptoms, the main reason for surgery is cosmetic.
References
- Physiotherapist, N. P. (2023d, December 13). Cubitus Varus – Cause, Treatment, Exercise. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/cubitus-varus/
- Vashisht, S., & Banerjee, S. (2023, August 14). Cubitus Varus. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560694/
- Dhameliya, N. (2023a, April 17). Cubitus Varus Deformity: Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/cubitus-varus-deformity/