Coxa Profunda
What is coxa profunda ?
Coxa Profunda is the name of a hip joint-related medical ailment. It is mostly used to describe an abnormal growth in the acetabulum’s depth, the hip joint’s socket where the femoral head (or “ball” element of the hip joint) articulates.
The acetabulum, which is shallow in a normal hip joint, fits the femoral head snugly. On the other hand, coxa profunda causes the acetabulum to drop deeper, which may alter how the hip joint functions. This ailment is frequently observed in conjunction with other hip disorders such as femoroacetabular impingement (FAI) or hip dysplasia.
An extended acetabular extent, also known as a cavernous acetabular socket, is referred to as “coxa profunda”.
The study of epidemiology:
In females, coxa profunda is far more common.
Reasons for coxa profunda:
A pincer-type lesion eventually appears as a result of acetabular overcoverage, which is then followed by a lesion of the acetabular cartilage or labrum. As a result, hip osteoarthritis (OA) in young adults is one of the causes, resulting in significant hip joint pain and limited mobility.
Symptoms of Coxa profunda:
Coxa profunda symptoms that can result in,
- hip pain
- restricted range of motion,
- hip cartilage injury or hip labral tears as a result of changed joint mechanics.
Radiographic characteristics:
Standard radiograph
The lateral edge of the acetabular teardrop is seen on anteroposterior (AP) view pelvic X-rays as being medial to or in line with the ischial ilial line 4.
Differential diagnosis:
It is important to distinguish between the coxa profunda and the protrusion acetabuli, where the femoral head is positioned medial to the ischial ilial line 4.
Associated pathology
Although coxa profunda is a non-specific finding that has been linked to femoroacetabular impingement of the pincer type, it is also a finding that should be investigated in individuals who do not exhibit any symptoms.
Treatment
Conservative methods of treating coxa profunda may include physical therapy and pain medication; however, in more severe cases or when coxa profunda is linked to other hip problems, surgery may be required.
Hip arthroscopy can be used as an alternative method of medical care for mild cases to improve joint biomechanical as well as minimize acetabular over-coverage, hence delaying the progression of hip osteoarthritis.
Intra-articular injections of blood platelet growth factors (PRPs), stem cells derived from fat, collagen, or hyaluronic acid, are a satisfactory treatment to control the symptoms, especially the pain, in intermediate forms where arthroscopic hip surgery does not benefit the patient. However, the hip’s arch of mobility will not be improved.
The preferred course of treatment for severe cases with pre-existing degenerative alterations is the implantation of a complete hip prosthesis (PTC), which relieves discomfort and restores normal mobility.
A successful surgical procedure to treat some hip pathologies involving the coxa profunda is surgical hip dislocation. It is possible to treat concurrent pathology such as labral tears, degeneration, or ossification, as well as Femoroacetabular impingement syndrome (FAIS).
As with any medical issue, seeking the advice of a trained healthcare provider is crucial for an accurate diagnosis and a treatment plan that is customized to the patient’s unique circumstances.
Physical therapy Interventions
Physical therapy is necessary. Exercises that strengthen the muscles surrounding the hip joint, increase hip joint mobility, and correct potential important movement patterns can all be created by therapists. A physical therapist can offer advice on appropriate movement methods and modifications to activities.
Hip Mobility Exercises: To increase the hip joint’s flexibility and mobility, physiotherapists will create a range of motion routines. These workouts may include controlled movements and mild stretching.
Exercises for Strengthening: Increasing the strength of the muscles surrounding the hip joint, such as the rotators, abductors, and flexors, can assist in stabilizing the joint and enhance function. Resistance bands, bodyweight exercises, or the use of workout equipment can all be used in strengthening activities.
Core Strengthening: By decreasing needless tension, strengthening the core muscles can aid with general stability and posture, which can indirectly benefit the hip joint.
Training for Proprioception and Balance: This type of exercise helps the body become more aware of where it is in space and improves balance, both of which are critical for the stability of the hip joints during a variety of activities.
Functional Training: To assist people regain the capacity to conduct daily duties without aggravating their symptoms, physiotherapists frequently create workouts that replicate real-life movements and activities.
Manual therapy: Techniques like joint mobilization and soft tissue massage can help reduce tense muscles, improve joint mobility, and relieve pain.
Correcting bad posture can help lessen the load on the hip joint and keep symptoms from getting worse.
Activity Modification: To lessen hip joint stress while enabling people to continue being active, physiotherapists offer advice on how to change certain activities and movement patterns.
Pain Management Techniques: Physiotherapists can offer guidance on pain alleviation tactics as well as instruction on pain management techniques including applying heat or ice.
Education: An important part of physical therapy is teaching patients about their disease, how to move their bodies properly, and how to avoid problems in the future.
Assistive aids: Reducing weight-bearing on the injured hip with crutches or other aids can help the hip heal and rest.
Exercise
Hip Flexor Stretch: Stretch your hip flexors by bending down on one knee and placing your other foot on the front side while maintaining a 90-degree angle in both knees. Move your weight forward gradually to extend the back leg’s hip flexors.
Exercise for Hip Abduction: Lie on your side with the injured leg elevated. Maintaining a straight posture, elevate the upper leg and then lower it back down. The hip abductor muscles are strengthened as a result.
Exercise Clamshell: While resting on your back, bend the two knees together. Open your knees like a clamshell while keeping your feet touching, then close them again.

Seated Hip Stretch: Sit on the edge of a chair and cross the injured ankle over the other knee. When extending the hip, gently apply pressure on the crossed knee.
Piriformis Stretch: Stretching the piriformis involves lying on your back and crossing the affected leg over the other knee. Pull the patient’s lower knee towards their chest to extend the piriformis muscle.

Wall Squats: Place your feet hip-width apart and approximately two feet away from the wall as you stand against it. As you down the wall, keep your knees parallel to the patient’s toes.

Leg Lifting Sideways: While lying on your unaffected side, stretch your legs in a sideways motion. Straighten the affected leg and raise it upward. Return it to its lower position.
Internal and External Rotation: Rotate both inside and outside while sitting on a chair and wrap a resistance band over your thighs. For external rotation, gently press your knees outward against the band; for internal rotation, press them inward.
Standing Hip Abduction: Take a stance and grasp a firm surface. Maintaining its upright posture, raise the affected leg out to the side. Return it to its lower position.

Hip External Rotation Stretch: While resting on the back of your body, bend both of your knees to extend your hips externally. To extend the outer hip, cross the affected ankle over the other knee and gently press the crossed knee away from your body.
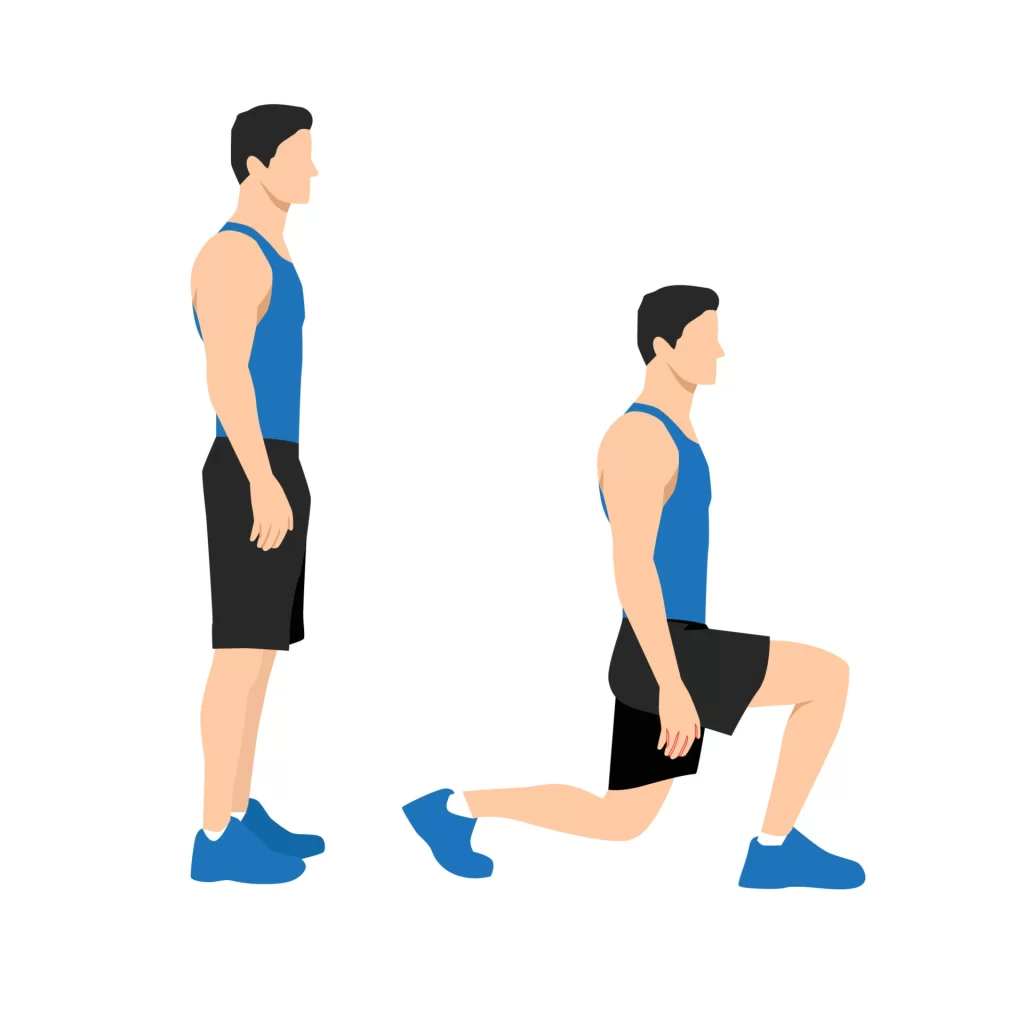
Lunges: Lower your body into a lunge position by taking a stride forward with your unaffected leg. Verify that the patient’s knee does not extend past your toes. Return to the beginning posture by pushing yourself through the exercise again.
Single-Leg Balance: Elevate the affected leg off the ground while standing on the unaffected limb. Hold this posture for a predetermined amount of time while keeping your balance. If necessary, you can utilize a steady surface as support.
Step-ups: Raise the affected knee towards your chest while stepping up with the unaffected leg on a stable step or platform. Retrace your steps and carry on.
Prone Leg Raises: Raise the affected leg off the ground by straightening it as you lie on your stomach. Lower it one more, then do it again.

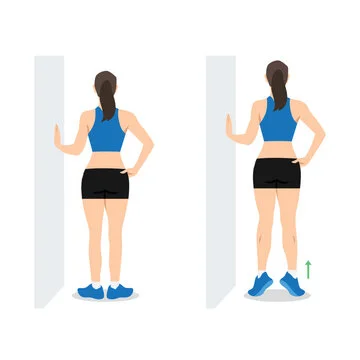
The calf raises The patient should be standing with their heels hanging over the edge of a step or platform. Ascend to the patient’s toes and then descend your heels below the step.
Prevention:
- Keep a Healthy Weight: Carrying too much weight might strain the hip joint. One can lower stress while maintaining a healthy weight by eating an appropriate diet and exercising frequently.
- Remain Active: Maintaining a regular exercise regimen helps maintain the strength and flexibility of the muscles surrounding the hip joint. Exercises that improve hip mobility and stability should be your main focus.
- Warm Up and Cool Down: It’s possible to avoid strains and injuries to the hip and surrounding muscles by warming up properly before exercise and cooling down afterward.
- Technique: Whether you’re playing sports, working out, or going about your everyday business, employing good technique and body mechanics will help lower the chance of putting too much strain on your hip joint.
- Avoid abuse: While it’s crucial to keep active, avoid engaging in excessive or repetitive activities since these may result in abuse of the hip joints and possible harm.
- Pay Attention to Your Body: It’s critical to take quick action if you feel hip pain or discomfort when engaging in certain activities. Ignoring pain could make any underlying problems worse.
- Appropriate Footwear: During a variety of activities, wearing footwear that is supportive and cushioned can assist lessen the strain on the hip joint.
- Cross-Training: To avoid overusing particular muscles or joints, try a range of workouts and activities.
- Sustain Good Posture: Maintaining proper posture will help with the equal distribution of body weight and reduce stress on the hip joint.
- Remain Hydrated: Remaining hydrated aids in cartilage integrity preservation and promotes overall joint health.
- Limit Extended Sitting: To avoid hip joint stiffness if your lifestyle entails a lot of sitting, take periodic breaks to stand, stretch, and walk about.
- Speak with a Professional: See a healthcare provider if you are experiencing any discomfort or have questions regarding your hip joint. Potential problems can be avoided with the help of suitable supervision and early intervention.
At-Home Counselling:
Rest and Adjust Your Activities: Keep clear of activities that exacerbate your hip pain, particularly those that call for high-impact workouts or repetitive hip motions. Make changes to your everyday routine to lessen the strain on your hip joint.
Ice and Heat Therapy: Several times a day, applying ice packs for 15 to 20 minutes will help lessen discomfort and inflammation. If heat therapy relieves your muscles’ tension, try switching between ice and heat.
Pain management: Ibuprofen and paracetamol, two over-the-counter pain medications, can help reduce discomfort and inflammation. However, before using them frequently, speak with a physician.
Control Your Weight: Excessive weight may put stress on your hip joints.
Proper Footwear: Hip discomfort can be reduced by donning supportive, cushioned shoes. Steer clear of shoes that exacerbate bad posture or high heels.
Avoid Extended Sitting: If you work a desk job, take breaks. Stretch occasionally and take short walks to avoid becoming stiff.
Sleeping Position: Try sleeping on your back with a cushion between your knees for support if your hip pain interferes with your ability to fall asleep.
FAQs
A coxa Profunda: what is it?
An acetabular socket that is deeply recessed is referred to as coxa profunda. The intrapelvic displacement of the femoral head and acetabulum resulting in the femoral head projecting medially towards the ischial ilial line is known as acetabular protrusion.
What is the coxa profunda treatment?
Finally, surgical hip dislocation is a useful surgical procedure for treating coxa profunda-related hip pathologies.
How frequent is profunda coxa?
Along with femoroacetabular collision, coxa profunda was seen in 75% of the thirty-three (33) asymptomatic hips and identified in 65% of the fifty (50) hips. In females, coxa profunda was more common than in males (70% vs 24%; p < 0.001).
Why does coxa profunda occur?
As a result of acetabular overcoverage, a pincer-type lesion eventually forms, followed by a lesion of the acetabular labrum and acetabular cartilage.
Does coxa profunda hurt?
Dramatic pain from the inflamed, cystic, and contused labrum may be seen in the clinical picture. In contrast, the labrum is not involved in the early phases of impingement in patients with cam-type Femoroacetabular Impingement Syndrome (FAIS).
References
- Patel, D. (2023, August 19). Femoroacetabular Impingement – Cause, Symptoms, Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/femoroacetabular-impingement/#Physiotherapy_Treatment
- Serasiya, A. (2023, July 25). Coxa Profunda – Cause, Symptoms, Radiology, Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/coxa-profunda/