Common Peroneal Nerve
Introduction
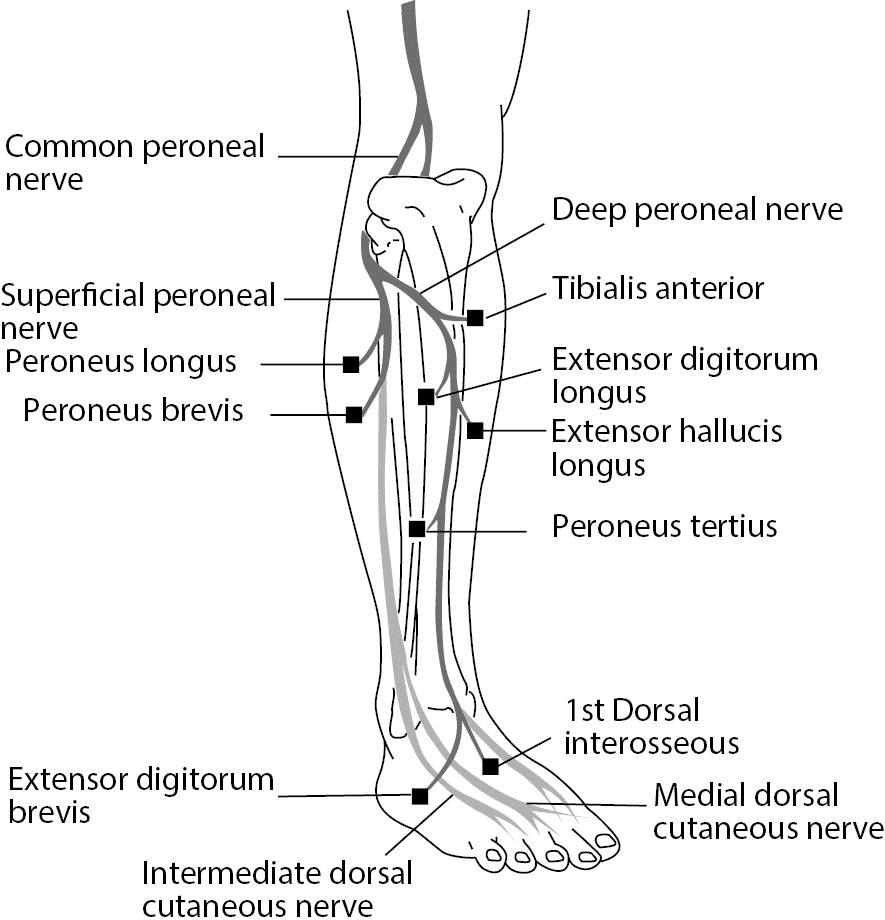
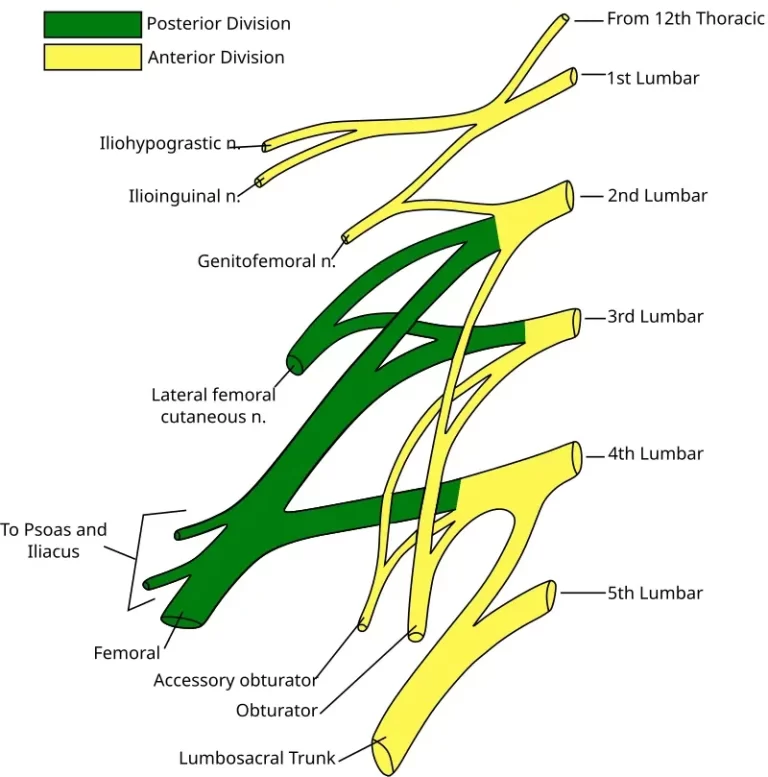
The common peroneal nerve (also known as the common fibular nerve) is a branch of the sciatic nerve, originating in the lumbosacral plexus (L4-S2). It wraps around the head of the fibula, making it vulnerable to injury. The nerve then divides into the superficial and deep peroneal nerves, innervating the lateral and anterior compartments of the leg, respectively.
It provides motor function to muscles involved in foot eversion and dorsiflexion and sensory function to the anterolateral leg and dorsum of the foot. Injury can cause foot drop and sensory deficits.
In particular, it starts from the sciatic nerve, splits off from it proximal to the popliteal fossa, and travels via the popliteal fossa and down the posterolateral side of the leg, passing behind the proximal fibular head and deep to the long head of the biceps femoris. It splits into the superficial and deep fibular nerves at the fibular neck, just inferior and lateral to the fibular head. Within the lateral compartment, the superficial fibular nerve runs anterolaterally between the extensor digitorum longus and fibularis longus muscles.
Before it reaches the ankle and foot, it ends its distal journey inside the lateral compartment. Between the tibialis anterior muscle and the extensor digitorum longus muscle, the deep fibular nerve flows anteriorly and parallels the anterior tibial artery. The deep fibular nerve passes between two muscles in the anterior leg compartment as it moves distally. These muscles include the tibialis anterior and extensor hallucis longus.
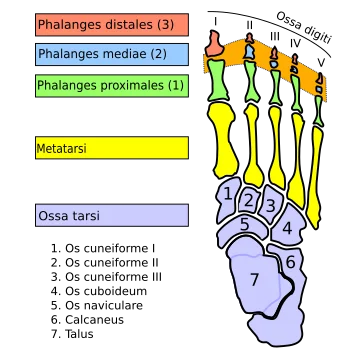
The nerve splits into medial and lateral branches as it gets closer to the foot anterior to the talus. The medial branch ends between the first two metatarsals after following the dorsalis pedis artery. The lateral branch ends close to the fifth metatarsal after following the lateral tarsal artery.
Structure
The sciatic nerve’s smaller terminal branch is known as the common fibular nerve. Root values for the common fibular nerve are L4, L5, S1, and S2. It begins from the superior angle of the popliteal fossa and runs along the medial edge of the biceps femoris to the lateral angle of the popliteal fossa.
It then splits into terminal branches of the superficial and deep fibular nerves after winding around the fibula’s neck to puncture the fibularis longus. The popliteal fossa is where the common fibular nerve produces several branches before division.
Cutaneous branches
The skin of the top two-thirds of the lateral side of the leg is supplied by the lateral sural cutaneous nerve, also known as the lateral cutaneous nerve of the calf.
It connects to the sural nerve after running along the posterolateral side of the calf.
Articular branches
- Superior lateral genicular nerve – sits above the lateral femoral condyle and is associated with the artery of the same name.
- The Inferior lateral genicular nerve – is located right above the fibula’s head and runs alongside the artery of the same name.
- Recurrent genicular nerve – It originates at the site where the common fibular nerve divides, and it subsequently ascends anterior to the knee joint along with the anterior recurrent tibial artery to supply the tibialis anterior muscle and the knee joint.
Motor branches
The nerve to the short head of the biceps femoris muscle is the sole motor branch that emerges directly from the common fibular nerve.
Function
Nerve roots: L4 – S2
Motor: directly innervates the biceps femoris’ short head. further feeds the muscles in the leg’s anterior and lateral compartments (via branches).
Sensory: innervates the lower posterolateral and upper lateral leg skin. furthermore provides cutaneous innervation to the dorsum of the foot and the skin of the anterolateral leg (via branches).
Motor Functions
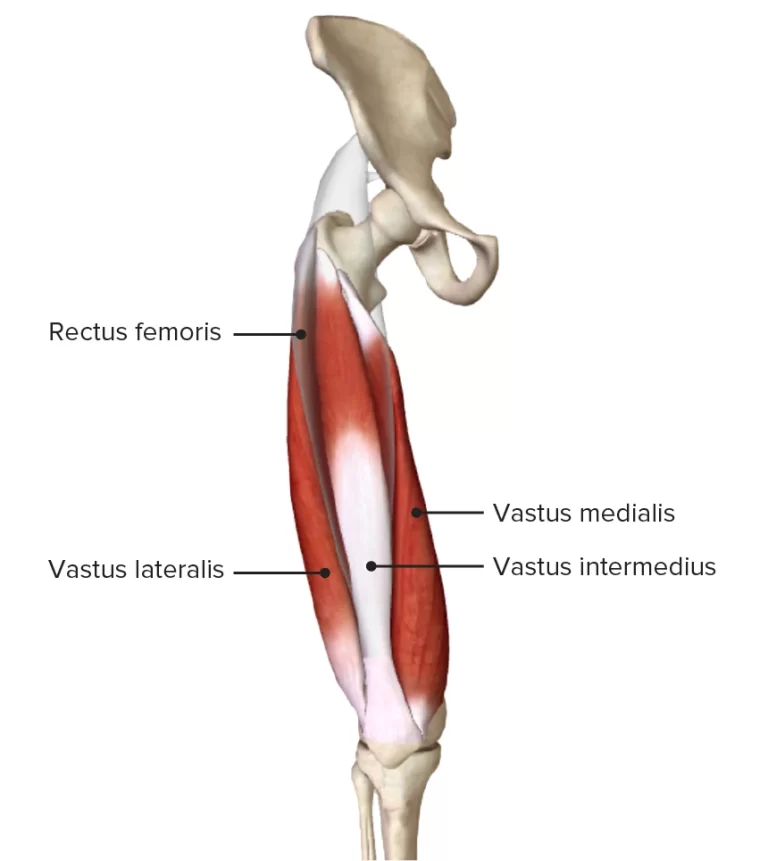
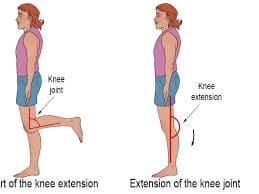
The short head of the biceps femoris muscle, which is a component of the hamstring muscles that flex at the knee, is innervated by the common fibular nerve.
Furthermore, muscles are innervated by its terminal branches:
Superficial fibular nerve: innervates the fibularis longus and brevis muscles, which are located in the leg’s lateral compartment. The foot is everted by these muscles.
Deep fibular nerve: innervates the tibialis anterior, extensor digitorum longus, and extensor hallucis longus muscles, which are located in the anterior compartment of the leg. These muscles aid in dorsiflexion of the foot and finger lengthening. Additionally, it innervates a few of the foot’s intrinsic muscles.
The patient may lose the capacity to dorsiflex, evert the foot, and stretch the digits if there is injury to the common fibular nerve.
Sensory Functions
As the common fibular nerve passes across the lateral head of the gastrocnemius, it immediately gives rise to two cutaneous branches.
- Sural communicating nerve: The sural nerve is created when this nerve joins a branch of the tibial nerve. The skin on the lower posterolateral leg is innervated by the sural nerve. Lateral sural
- cutaneous nerve: innervates the upper lateral leg’s skin. Along with these nerves, the common fibular nerve’s terminal branches also have a cutaneous purpose:
Superficial fibular nerve: innervates the dorsum of the foot and the skin of the anterolateral leg, except the area between the first and second toes. The skin between the first and second toes is innervated by the deep fibular nerve.
Course
The smaller of the sciatic nerve’s two terminal branches—the other being the tibial nerve—is the common fibular (peroneal) nerve (root value L4-S2). The majority of the fibers of the common fibular (peroneal) nerve come from the sacral plexus’s posterior division.
At the distal portion of the thigh, close to the top of the popliteal fossa, the nerve emerges from the sciatic nerve. After that, it moves inferolaterally via the popliteal fossa in the direction of the fibular head. It is situated lateral to the gastrocnemius muscle and medially to the tendon of the biceps femoris muscle in the fossa.
The nerve subsequently enters the leg’s anterior compartment by puncturing the leg’s fascia. The fibular neck is surrounded by the common fibular nerve. Under the fibularis longus muscle, the nerve then splits into two terminal branches, the superficial and deep fibular (peroneal) nerves.
Branches
The common peroneal nerve emits the following when it is still in the popliteal fossa:
The knee joint is reached via the genicular branches.
The calf’s lateral cutaneous nerve
A sural communicative branch.
The two terminal branches consist of
- Superficial peroneal nerve L5, S1, 2
- Deep peroneal nerve L4,5, S1,2
Superficial fibular (peroneal) nerve
Between the fibula and the proximal portion of the fibularis longus muscle, the common peroneal nerve bifurcates to form the superficial branch, commonly referred to as the superficial fibular (peroneal) nerve.
The fibularis longus muscle is reached by this nerve when it dips deeply. It splits into the medial dorsal cutaneous nerve and the intermediate dorsal cutaneous nerve after penetrating the deep fascia in the distal part of the leg. The superficial fibular (peroneal) nerve supplies the lower anterolateral leg’s skin with sensory information and motor control to the muscles of the fibularis longus and fibularis brevis.
Deep fibular (peroneal) nerve
The bifurcation of the common fibular nerve also gives birth to the deep branch of the fibular nerve, which is also referred to as the deep fibular (peroneal) nerve. This nerve gives innervation to the leg’s extensor (anterior) compartment after passing through the interosseous membrane.
Together with the anterior tibial artery, the nerve then descends on the crural interosseous membrane between the tibialis anterior and extensor hallucis longus. The lateral and medial terminal branches of the deep fibular nerve split off near its termination.
Anatomical Variations
Similar to most human anatomy, the common fibular nerve’s route and surrounding anatomy have several variations that surgeons should be aware of, particularly if they plan to decompress the nerve. The chance of compressed nerves may also rise or fall as a result of these variations.
Research comparing the anatomy of surgically decompressed nerves and cadavers revealed some significant differences. The first one has fibrous tissue behind the superficial head of the peroneus longus, forming a structure resembling a band. The next variation likewise has fibrous tissue that forms a band-like structure, however, this tissue is found on the superficial surface of the peroneus longus muscle’s deep head. The last variation mentioned involves two muscles along with their unusual origin and junction.
Though some persons begin together at the fibular head and split apart as they progress distally, the soleus and fibularis longus muscles often begin independently on the fibular head.
Examination
Common Peroneal Tension Test
The patient’s symptoms were replicated by a standard peroneal nerve stress test (SLUMP test while biassing the foot and ankle in PF/IN). The three requirements for positive neural tension were satisfied by the symptoms:
The patient’s symptoms are reproduced differently from side to side, with a remote component.
Symptoms may be replicated by the peroneal nerve tension test, a variant of the SLR in which the ankle is plantarflexed and inverted at the site of initial resistance.
Symptoms may also be reproduced by Tinel’s sign, which is the palpation or tapping of the nerve around the fibular head.
The deep peroneal nerve is quickly and grossly screened by heel walking (dorsiflexon, L4, L5).
The superficial peroneal nerve (L5, S1) and tibial nerve (S1-2) are quickly and grossly screened during toe walking.
Weakness of the tibialis anterior, extensor digitorum longus and brevis, extensor hallucis longus and brevis, peroneus longus, peroneus brevis, and peroneus tertius may also be detected by manual muscle testing. The physical therapist may see toe drag during the swing phase, foot drop, or a “slapping” gait during the gait analysis.
Clinical Importance
Compared to other neuromuscular problems, the common fibular nerve is a topic that is explored a lot because of its characteristic clinical appearance and frequent damage. It is fairly susceptible to harm due to its placement. It passes across the fibula’s neck on the lateral part of the knee, where skin, subcutaneous fat, and fascia provide their only defense. Thus, the common fibular nerve is frequently harmed by a variety of lateral knee injuries. For instance, a football player may sustain a common fibular nerve damage and a fibular neck fracture if they are tackled from the side.
The patient would probably arrive with knee discomfort, ankle eversion, loss of foot dorsiflexion, and loss of feeling in the dorsum of the foot and along the lateral leg. Patients who are unable to dorsiflex their feet are also prone to exhibit a “foot drop.”
The swinging phase of the gait cycle is when this phenomenon happens. Instead of clearing the ground as in a normal stride, the toes drag on it due to a lack of dorsiflexion. Exaggerating hip abduction to provide more foot space is a common way for the patient to make up for foot-dragging.
Nerve compression when it passes over or distal to the fibular head and neck is another typical source of damage to the common fibular nerve. This can happen when a cast or splint is applied too tightly or improperly, or it can happen when someone has compartment syndrome following a burn or trauma.
In both cases, the compressed nerve would first induce paresthesias, then weakening and loss of feeling, and finally, if treatment is not received, loss of ankle eversion and dorsiflexion of the foot. It should be mentioned that distal pulses should be checked in these situations since there may be a vascular compromise.
Proximal injuries at the sciatic nerve level can also cause clinical manifestations that resemble damage to the common fibular nerve. Piriformis syndrome is a typical case. The sciatic nerve, which supplies fibers to the common fibular nerve, may become trapped inside the piriformis muscle in certain situations or anatomical variations.
Loss of dorsiflexion, loss of foot eversion, and loss of sensation to the anterolateral part of the leg and dorsum of the foot are symptoms of a tight piriformis that might be comparable to those of a traditional common fibular nerve injury. Nevertheless, in addition to these symptoms, the patient may also have pains that are close to the knee, which is how sciatica often manifests. To create an appropriate treatment strategy, it is crucial to distinguish between sciatica, piriformis syndrome, or just typical fibular nerve damage.
Surgical Importance
Nerve-related surgical procedures include:
Decompression of the fibular (peroneal) nerve
An incision is created across the fibula’s neck to surgically decompress the common fibular nerve. The fascia that envelops the nerves on the leg’s lateral side is freed.
Decompression of the deep fibular (peroneal) nerve
A ligament from the extensor digitorum brevis muscle that crosses over the deep fibular nerve, applying pressure and producing discomfort, is freed during surgery to treat deep fibular nerve entrapment in the foot.
FAQs
What is the common peroneal nerve’s primary purpose?
The sciatic nerve gives rise to the common peroneal nerve. It gives the foot, toes, and lower leg mobility and feeling. Peripheral neuropathy, or injury to the nerves outside the brain or spinal cord, includes common dysfunction of the peroneal nerve. Any age can be affected by this disease.
Which workout is best for the peroneal nerve?
Exercise Program for Peroneal Tendonitis
Place your hands on the wall as you face it. Bend your front knee and shift your weight forward while maintaining both heels on the ground and your toes pointed forward. If you can, hold the stretch for at least 15 to 30 seconds. Do this three times.
What is the route of the common peroneal nerve?
From the knee to the lower leg, the common peroneal nerve passes below the fibula’s head. After that, it divides into the deep and superficial fibular nerves.
Where is the peroneal nerve most frequently injured?
Both the knee (common peroneal nerve) and the spine (lumbar nerve roots) are frequently affected. In particular, the deep branch of the peroneal nerve is in charge of the loss of function when it is affected.
References
Common fibular (peroneal) nerve. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/common-fibular-nerve
TeachMeAnatomy. (2024a, March 30). The common fibular nerve – course – motor – sensory – TeachMeAnatomy. https://teachmeanatomy.info/lower-limb/nerves/common-fibular-nerve/
Wikipedia contributors. (2024a, August 4). Common fibular nerve. Wikipedia. https://en.wikipedia.org/wiki/Common_fibular_nerve
Common fibular (peroneal) nerve. (2022,October 17).StatPearlshttps://www.ncbi.nlm.nih.gov/books/NBK532968/