Calf Muscle Pain
Calf muscle pain is a common issue that can affect individuals of all ages and activity levels. Located at the back of the lower leg, the calf muscles play a vital role in supporting movements like walking, running, and jumping. Pain in this area can result from various factors, such as overuse, injuries, muscle strain, or underlying medical conditions.
Understanding the causes and symptoms of calf muscle pain is the first step toward effective treatment and recovery, ensuring you can maintain an active and pain-free lifestyle.
What is calf muscle pain?
A dull aching or a sharp pain behind your shinbone in the back of your leg is frequently a sign of calf muscle pain. For each person, it may feel somewhat different. if engaging in physical activities like walking and jogging causes you to feel pain.
Usually, the reason is muscular. However, if the pain is abrupt and has no apparent source, it may be a blood vessel issue.
However, persistent or severe calf pain is frequently an indication that your lower leg muscles aren’t receiving enough blood.
What does calf pain feel like?
A strong, dull, and painful pain at the back of the lower leg, often accompanied by tightness, is how some individuals describe their calf pain.
Causes of calf muscle pain
Numerous factors can contribute to calf pain, which can also be linked to other medical disorders. Calf pain may usually be treated on your own, but in some cases, you might need to see a doctor right away. Purchase supplements and vitamins. These are a few frequent conditions that are linked to calf pain.
Muscle cramps
- Exercise, injury, dehydration, and mineral shortages are common causes of cramps. Additionally, they will be linked to more severe illnesses like:
- Hypothyroidism
- Diabetes,
- alcoholism,
- pregnancy, and
- kidney failure
- Muscle cramps can occur in up to 50% of pregnant women, particularly during the final three months before zonal leg cramps. These cramps, which mostly affect the calf muscle, might be caused by various medical disorders or by taking certain drugs, like as beta-blockers, diuretics, and stains.
Muscle strain
- Your calf muscle may be strained, for instance, when you begin a new workout program or enhance leg activities. This might involve activities like cycling and running.
- Lifting weights
- A muscular strain typically manifests as an abrupt onset of pain, soreness, and restricted range of motion.
- Compression, ice, rest, and over-the-counter (OTC) pain relievers are effective at-home treatments for mild to severe strains.
- Medical attention may be required for more serious tears or strains.
Sciatica pain
- Problems with the sciatic nerve cause sciatica.
- Packs that are hot or chilly
- OTC painkillers
- Physical treatment
- Steer clear of extended standing or sitting
- Overuse, strain, and tension on the Achilles tendon—which joins the soleus, plantaris, and gastrocnemius muscles at the rear of the ankle—cause Achilles tendonitis. Typical signs and symptoms may include:
- Tendon inflammation
- Pain
- The rear of the leg is stiff.
- Easy remedies at home might be beneficial. These might consist of:
- Extending
- Lowering the degree of activity
- Using over-the-counter painkillers
- It’s crucial to consult a doctor if your pain is becoming worse or if home remedies don’t help.
Deep vein thrombosis(DVT)
- DVT can be caused by a variety of disorders and circumstances. These might consist of:
- DVT in one’s family or personally
- Smoking
- Being obese or overweight
- Other disorders that might cause pregnancy complications
- Among the signs and symptoms of DVT are:
- Inflammation of the leg, ankle, or foot
- The act of cramping
- Tenderness or pain in the legs
- Discoloration of the skin
- The vein thickens or becomes solid.
- When touched, the affected skin feels hotter than the surrounding region.
- Depending on the skin tone, the affected region becomes blue, pale, or reddish.
- If you experience any DVT symptoms, you should see a doctor right once.
Compartment syndrome
- When excessive pressure accumulates inside the muscles, a potentially dangerous condition known as acute compartment syndrome can develop.
- This usually occurs following significant damage to the region, such as a fracture or fractured bone. The condition may also be caused by the usage of steroid hormones or crape bandages. Acute compartment syndrome can cause pain that is worse than the actual injury.
- Among the signs of compartment syndrome are:
- Trouble moving the affected area
- Severe stiffness or fullness inside the muscle
- Even if paralysis or numbness are later signs of irreversible damage,
- When exercising, this results in leg pain. When the action is halted, the pain stops. It may also result in:
- Feeling numb
- Having trouble moving the foot
- Muscle bulging that is visible
- People with chronic compartment syndrome may find that physical therapy helps them feel less pain. If this doesn’t help, surgery can be a possibility as well.
Contusions
- A kick to the calf, for example, might cause injury to muscular tissue without rupturing the skin.
- Bruising and pain are common symptoms of calf contusions.
- Compartment syndrome, a serious illness that prevents blood from reaching your leg muscles, can be caused by severe contusions.
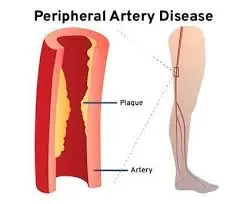
Claudication
- Walking or exercising might cause muscular soreness if you have intermittent claudication.
Sing and symptoms of calf muscle pain
The following symptoms might point to a more severe condition:
- Swelling
- The calf’s unusually pale color or numbness
- Leg and calf tingling and numbness
- Unexpected onset of weakness in the leg
- Retention of fluids
- Calf redness
- The calf’s warmth and tenderness
- If you experience any of these symptoms in addition to calf pain, you should see a doctor.
Differential Diagnosis
- Muscle strain:
- Calf Strain
- gastrocnemius, soleus, plantaris.
- Calf Strain
- contusion: gastrocnemius.
- Compartment syndrome:
- syndrome of the deep posterior compartment.
- Referred Pain:
- Myofascial structures, superior tibiofibular joint, baker’s cyst, knee posterior cruciate ligament, knee posterior capsular sprain, lumbar spine pain (also known as lumbar radiating pain or somatic pain), Ankle (Tibiotalar) or Knee Osteoarthritis Achilles tendinopathy.
- Tendon injuries: Plantaris tendinopathy are example of tendon injury caused by osteoarthritis.
- Nerve entrapment: tibial, sural, and common peroneal nerves and branches.
- Fractures: (fibula, posterior cortex of the tibia) or fractures (including malunion).
- Vascular anomalies: include aneurysm, arterial insufficiency, endo-fibrosis of the external arteria iliaca, and entrapment of the arteria poplitea. Varicose veins, such as superficial thrombosis, deep vein thrombosis, and venous insufficiency.
Diagnosis
Subjective assessment
- History, current symptoms, and sing.
- Note Calf strain injuries can manifest as a noticeable abnormality that resembles a bulge or a flaw in the muscular belly.
- Palpation
- Tenderness
- Swelling.
Treatment of Calf muscle pain
Medical treatment
- Over-the-counter (OTC) drugs like:
- ibuprofen (Advil) and
- paracetamol (Tylenol)
- Aleve (naproxen)
Physical Therapy Treatment
The purpose of exercise therapy is
- Reduce calf muscle pain
- Reduce the edema of the muscles
- Strengthens the calf muscles
- regain the patient’s trust
- Restore patients’ whole range of motion
Immediate treatment
- Rest. Additionally, you will require a piece of protective equipment, such as a sling or crutches.
- Ice.
- Compression. Apply a gentle bandage or ace wrap to the affected region.
- Elevation. Raise the damaged region to an A level above the heart.
Electric modalities
Ultrasound
- helps lessen pain and swelling
- Using cold water baths and ice packs as part of cryotherapy can help reduce edema and inflammation in the affected region.
- It is advised to apply colds continuously for 25 to 30 minutes at a time, many times throughout the day.
TENS
- Muscle spasms and pain may be lessened using transcutaneous electrical nerve stimulation (TENS).
IFT (interferential treatment)
- The following are the primary clinical uses for which IFT (interferential treatment) seems to be employed:
- Pain relief
- Stimulation of muscles
- Increased blood flow in the area
- decrease in edema.
Massage
- Look for any contraindications.
- To ensure that sports massage is safe, always check for contraindications, particularly deep vein thrombosis.
- Placement
- Rest your feet comfortably in a prone posture, either by letting them hang over the edge of the massage table or by supporting them with a rolled towel.
- Effleurage that is light
- Start by using the “effleurage” technique. In order to prepare the tissues for deeper techniques, these mild stroking techniques start to warm them up.
- Deep effleurage
- As before, but gradually penetrating the tissues more deeply. Avoid going so deep that the patient becomes tense from pain since it will negate the benefit.
- Petrissage
- There are a variety of kneading techniques. Work down as far as it feels comfortable. As the ailment improves over time, massage pressure can be raised. Use effleurage and petrissage procedures alternately.
- Tapotement
- These percussion-style techniques are optional. They could be preferred by certain therapists, but most likely only in the later phases of rehabilitation.
- Completing
- To complete the massage, switch back to gentle effleurage techniques.
Calf Muscle exercise
Towel stretch

- Wrap the face cloth around one foot’s ball. Hold the towel by both ends.
- After that, unwind for 30 seconds.
Inner calf ball massage
- With one knee bent to the side and the other in front of your torso, begin in the side-sit posture. As if performing cardiopulmonary resuscitation, press your weight onto the ball. Before proceeding to the next location, hold the ball in that spot and flex and point your foot thrice when you locate a sore spot.
ATM

- Make your knee straight.
- Point your foot back in front of your nose while simply moving your ankle. Continue until it becomes uncomfortable or you are unable to tilt it back any further.
- For ten seconds, maintain this posture.
- Get back to where you were before.
Heel raise
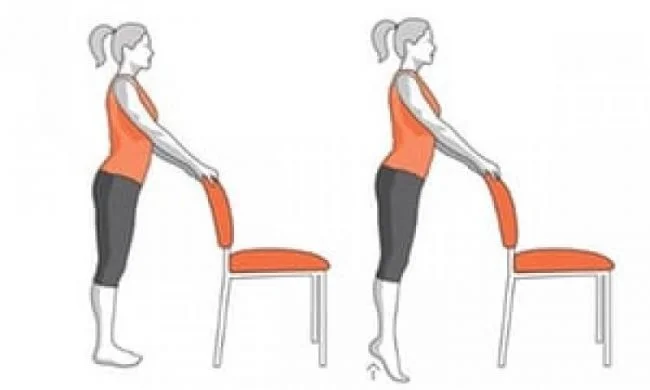
- Use your hand to steady yourself on a table if you require assistance keeping your equilibrium.
- To stand on your toes, lift both of your heels.
- Hold for ten seconds. Return to the starting position gradually.
- Do this fifteen times. Perform three sets each day.
- Keep your knees from locking.
- Keep your back straight.
Lunges

- Lower your body till the back knee is only a few inches above the ground while bending your knees.
- Maintain your weight on the front foot’s heel as you continue to the beginning position.
SLR
- This is known as a pelvic tilt.
- One leg should be straightened out along the floor and then gently raised 6 to 8 inches above the
- ground before being put back down.
- finish ten repetitions.
Solus stretch
- Keep the sore leg in the back as you stagger your feet while facing a wall.
- Without raising your affected heel off the floor, shift your weight in the direction of the wall.
- Hold for 20 seconds, then let go.
- Three repeats in a row
- Two times a day, do this.
Can calf pain be prevented?
- To strengthen and mend the calf, always stretch both before and after working out. If you’re starting anything new, build up gradually and avoid overdoing it.
- Increase your water intake to prevent cramping. Although the research is inconclusive, some people, particularly pregnant women, have reported that taking magnesium supplements helps them avoid cramping.
Conclusion
Calf muscle pain can disrupt daily activities and overall mobility, but with proper care and attention, it is manageable. Identifying the cause, following appropriate treatment, and adopting preventive measures can help alleviate pain and reduce the risk of recurrence, ensuring a healthy and active lifestyle.
FAQs
Is pain in the calf a sign of anything?
Excessive stretching of the calf muscle can result in calf strain, which can cause pain, stiffness, or weakness. Stretching both before and after exercise might help you avoid calf soreness and injuries. Additionally, calf pain may indicate more serious conditions such as sciatica, deep vein thrombosis (DVT), or Achilles tendinitis.
Can calf muscle pain be caused by low B12?
Impaired coordination: A B12 deficiency may result in ataxia, a neurological condition that impairs balance and coordination.
Can calf pain be associated with the heart?
However, it could indicate peripheral artery disease, which raises the chance of a major cardiovascular event such as a heart attack or stroke. Everybody occasionally has aches and pains in their legs.
Does pain in the calves indicate diabetes?
Leg pain and numbness or tingling from neuropathy can be signs of undiagnosed or uncontrolled diabetes, but diabetes itself is seldom the cause of leg pain. The feet and legs are the primary areas affected by peripheral neuropathy. Usually, focal neuropathy affects a single, targeted artery.
What is the source of calf pain?
Leg cramps may be caused by deficiencies in specific vitamins (such as vitamin B or vitamin D insufficiency) or minerals (such as calcium, magnesium, potassium, and phosphorous). Vitamin K may be able to help reduce leg cramps, according to a new study.
How can calf nerve pain be resolved?
Speaking of heat, ice and heat packs can frequently help with some types of leg nerve pain. Try using ice initially if the pain is new or could be related to an injury. Heat can improve blood flow and provide rapid alleviation for diabetic nerve pain in the legs as well as chronic nerve pain in the legs.
When is calf pain a cause for concern?
Get in touch with your doctor right away if you have: signs of an infection, such as redness, warmth, or soreness, or a temperature that is higher than 100 degrees Fahrenheit (37.8 degrees Celsius). a leg that is unusually bloated, pallid, or cold. calf soreness, particularly after extended periods of sitting, such as after a lengthy flight or vehicle travel.
If I have calf soreness, should I walk?
You should still be able to walk and bear weight on your calf if the pain is not too severe. Avoid jogging or walking if you have significant calf muscle pain. Avoid pushing through pain as this may exacerbate the issue.
How can calf pain be relieved?
Ice: Avoid putting ice on your skin directly. Compression: Cover your calf with a compression bandage or wrap. Compression minimizes swelling and lowers blood flow to the sore spot.
Is calf pain a sign of a blood clot?
In the affected location, a grume in a leg vein may result in pain, warmth, and soreness. There may not always be any obvious signs.
Which medication works best for calf pain?
Over-the-counter drugs: Over-the-counter painkillers like ibuprofen (Advil), acetaminophen (Tylenol), or naproxen (Aleve) can also be used to treat calf pain.
moderate motion: Calf soreness may be relieved by gentle stretching.
Calf raises are one example of a common workout.
How can tense calf muscles be relaxed?
Techniques for releasing tense calves
Place one foot in front of the other and bend your front knee slightly while you stand close to a wall.
For 15 to 20 seconds, hold this stretch.
When is calf pain a cause for concern?
Consult your physician right away if you have: symptoms of an illness, such as redness, warmth, or soreness; if not, you have a fever that is higher than 100 degrees Fahrenheit (37.8 degrees Celsius). a bloated, pallid, or abnormally cold leg. calf soreness, especially following extended periods of sitting, such as during a lengthy flight or vehicle travel.
Can calf pain result from dehydration?
Leg cramps may be especially familiar to you if you have calf and thigh muscles. Additionally, dehydration reduces blood volume. resulting in cramps and spasms as your muscles and organs receive less blood supply.
References
- Patel, D. (2023, December 13). Calf muscle pain – Cause, Symptoms, Treatment, Exercise. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/calf-muscle-pain/
- Professional, C. C. M. (2024, May 1). Calf Muscle Pain. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/22274-calf-muscle-pain






One Comment