Ataxic Gait
Introduction
Ataxic gait refers to a type of abnormal walking pattern characterized by a lack of coordination and balance. It typically results from damage or dysfunction in the cerebellum, the part of the brain responsible for motor control.
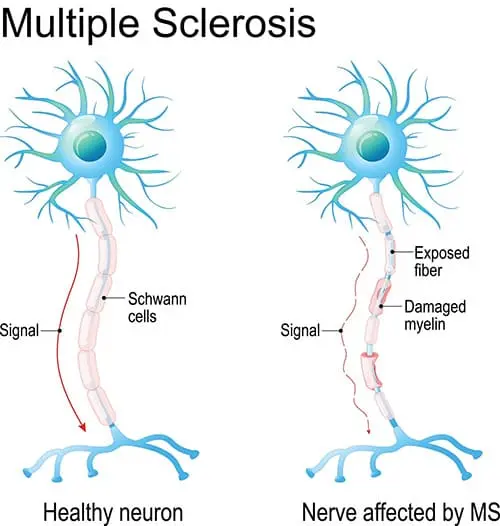
People with ataxic gait often present with a wide-based stance, irregular foot placement, and difficulty walking in a straight line, appearing unsteady or as if they are staggering. This condition can be caused by various underlying factors, such as neurological disorders, stroke, multiple sclerosis, or alcohol abuse, and it requires medical evaluation for proper diagnosis and treatment.
When walking, deficiencies in managing interaction forces (such as stepping over barriers) lead to some aspects of intralimb leg coordination issues.
On the other hand, most of the walking problems that have been documented are closely linked to deficits in dynamic balance, or inefficiencies in the trunk-two-leg coordination necessary to maintain the body’s center of gravity over the feet. Cerebellar persons with relatively minor balance abnormalities do not exhibit many gait ataxia symptoms; instead, they have substantial difficulties in leg coordination, as per studies. However, nearly all of the symptoms of gait ataxia are present in cerebellar persons who have significant balance abnormalities but only mildly impaired leg coordination.
What is the Ataxia?
Ataxia is characterized by clumsy, ungainly, or thoughtless motions due to difficulties in muscular coordination. It might manifest as a single illness or as a sign of several different conditions or circumstances. Depending on what causes ataxia, the condition may be able to be treated in addition to its symptoms being eradicated.
Types of Ataxia
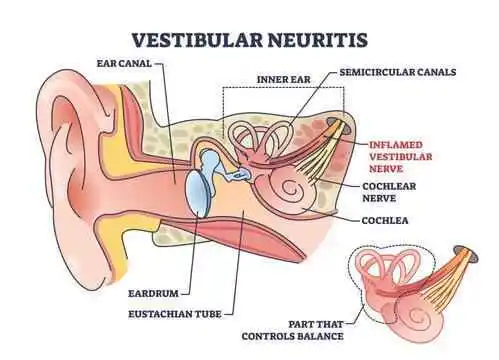
- Vestibular Ataxia: A problem affecting your inner ears, which are involved in your equilibrium, results in this type of dizziness. When your equilibrium is off, it’s hard to coordinate your movements.
- Cerebellar Ataxia: An anomaly in the cerebellar, a portion of the brain that coordinates how other brain regions interact with one another, causes this particular sort of ataxia.
- Sensory Ataxia: Your body has a sense known as “self-positioning,” which your brain may utilize to determine each body part’s location. For example, how do you locate your hands and feet when you are unable to see them, such as in a dark environment or when your eyes are closed. Your place’s perception is distorted by sensory ataxia.
What Causes Ataxic Gait?
- Ataxic gait may be attributed to conditions relevant to the brain, spinal cord, or peripheral nervous system. Distinctive features characterize ataxic gait impairments caused by cerebellar disorders.
- Cerebellar ataxia seems to be related to a number of disorders, including dysmetria, dyssynergia, dysdiadochokinesia, dysrhythmia, and intention tremor.
- The cerebellum handles fine motor movement through interactions with multiple brain areas. The cerebellum has trouble integrating data from the brain and the body as together when there is damage to the cerebellar neurons.
- Consequently, balance, posture, and smooth muscle action become difficult to coordinate, which negatively impacts gait function.
Sings and symptoms of the Ataxic Gait
- Gait ataxia affects about half of the patients. The additional signs include alternating hemiparesis, vertigo, tinnitus, and paresthesias of the fingers, toes, and corners of the mouth. Sudden unconsciousness is a possibility and usually passes in a few minutes.
- Stroke of the brainstem and cardiac arrhythmia are uncommon but potentially lethal outcomes. Usually, a severe throbbing occipital headache follows the neurological abnormalities. In little more than one-third of cases, nausea and vomiting are present.
- A common description of ataxia is a loss of balance or an inability to coordinate movements of the body that is not caused by the weakening of the muscles. A variety of voluntary motor actions, such as using the hands or fingers, speaking, moving the eyes, eating, putting on clothes, and pacing (ataxic gait), can exhibit symptoms of ataxia.
- Ataxia is a symptom of one or more underlying neurological illnesses rather than a separate sickness in and of its own. When it comes to a repetitive motor task like locomotion, ataxia symptoms can be very noticeable. The walking symptoms of ataxia are markedly different from those of orthopedic problems, leg spasticity, or Parkinson’s disease.
- Although youngsters may suffer from recurrent occurrences of basilar migraine, these attacks eventually turn into a pattern of typical headaches. Even when the patient has a classic headache, they may still feel dizziness and ataxia.
Types of Ataxic Gait
- Sensory Gait:
Atherosclerosis affects the cerebellum’s afferent fibers, or sensory inputs, but does not harm the cerebellum itself.
Signs and Symptoms
- In most cases, the patient’s lower leg no longer receives sensory or proprioceptive sensations.
- They do not know where their limbs are at all. They walk, paying close attention to the ground and taking more steps than are necessary. For additional stimulation of the sensory system, persons with sensory ataxia use their to tap the base.
2. Cerebellar Gait:
This unsteady, stumbling gait is aimed towards the cerebellar lesion due to a cerebellar lesion.
Signs and Symptoms
- Patients usually experience this by swaying to one side or the other, thus they often search for something to lean on, like a cane, a bed rail, or even the wall.
- Struggling to walk in tandem or heel-to-toe throws it off balance.
- Additionally, the stance is widened, yet this does not completely prevent stumbling.
- Titubation (a fore-and-aft tremor of the head and trunk) worsens noticeably when patients are told to close their feet and narrow their base, causing a fall.
- Hence, your posture is affected in an adverse way depending on whether your eyes are open or closed (negative Romberg’s).
Diagnosis of Ataxic Gait
A physical examination, neurological testing, and imaging procedures like MRIs or CT scans are commonly used to diagnose ataxic gait.
Physical and Neurological Examination
- The patient’s wide-based posture, difficulties turning, and unsteadiness can all be observed in their gait.
- Coordination problems can be detected by testing fine motor abilities, such as touching your nose with your finger.
- Assessing reflexes can be useful in detecting disorders related to the nervous system.
- Involuntary eye movements, or nystagmus, are frequently linked to cerebellar ataxia.
- To evaluate cognitive performance and rule out diseases like dementia, cognitive testing is used.
- Assessing touch, warmth, and vibration perception through sensory evaluation.
Imaging studies
- MRI: Magnetic resonance imaging is a diagnostic tool used to see abnormalities in the brain, such as tumors, strokes, and degenerative changes.
- CT scan: Computed tomography, or CT scan, is an additional technique for assessing the physical structure of the brain.
Treatment for the Ataxic Gait
The treatment plan is determined by the true origin of ataxic gait.Here are a few potential strategies:
Conservative Treatment
- Medications: Medication to treat underlying disorders may be recommended, depending on the etiology of ataxic gait. For instance, supplements could be advised if a vitamin deficit is the root cause. In cases where a neurological condition is the underlying reason, medication may be recommended to treat symptoms.
- Physical therapy: It can help with strength, balance, and coordination. Stretching, walking, and balancing training are a few possible workouts.
- Occupational therapy can assist people with ataxic gait in learning how to modify their everyday routines. Occupational therapists could provide safety and independence-enhancing techniques.
- Speech treatment: Speech therapy is a useful tool if ataxic gait is impairing swallowing or speech.
Surgical Treatment
In certain instances, treating the underlying cause of ataxic gait may include surgery. Surgery, for instance, may be necessary to remove a tumor or restore damaged nerves.
Physical Therapy for the Ataxic Gait
Treatment for ataxic gait must include physical therapy. Strength, flexibility, balance, and general functional abilities can all be developed by it.
The following are a few typical therapy methods for ataxic gait:
- Balance Exercises: These exercises aim to help you stay balanced and avoid falling. These could entail utilizing a balancing board, walking on a tightrope, or standing on one leg.
- Coordination activities: These exercises help increase the capacity to coordinate movements. They could entail exercises like finger-to-nose coordination, tapping your feet to a beat, or throwing and catching a ball.
- Strengthening exercise: Increasing the strength of your legs and core muscles will help you become more balanced and stable. This could entail workouts like planks, lunges, and squats.
- Gait training: To enhance gait patterns and lower the risk of falls, this entails walking practice with a therapist.
- Assistance equipment: To increase mobility and safety for people with ataxic gait, physical therapists can teach them how to use assistive devices such as wheelchairs, walkers, and canes.
Exercises for Ataxic Gait
Lower-back-rotation
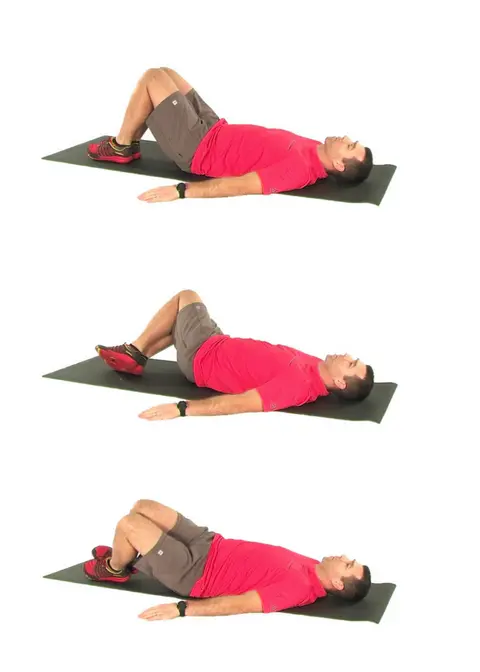
- This exercise will help with bed mobility and transfers because it concentrates on the segmental motions of the lower half of the body.
- Both knees should be bent, and the legs should be level and hip-distance apart. The arms need to be widely extended and apart from the torso.
- Allow a gradual rotation of both knees from side to side. Try to keep your upper body and back flat while your lower body pivots side to side.
- This exercise should be performed smoothly and softly ten times.
Quadriceps weight shifting

- Shifting Weight on All Four Legs The goal of this exercise is to strengthen your core stability while kneeling. It will be simpler to access and maintain insecure positions as a result.
- Kneel, placing hands under shoulders and knees under hips, starting with the spine in a neutral position. Return the opposite leg to hip height shortly after gradually elevating one arm to shoulder height.
- Hold your balance for a moment before dropping your arm and leg to the floor. On the opposite side, repeat with the arm and leg.
- Preserve your spine neutral during this exercise, and go gently and gradually. Try your best to complete ten repetitions.
Sit to stand
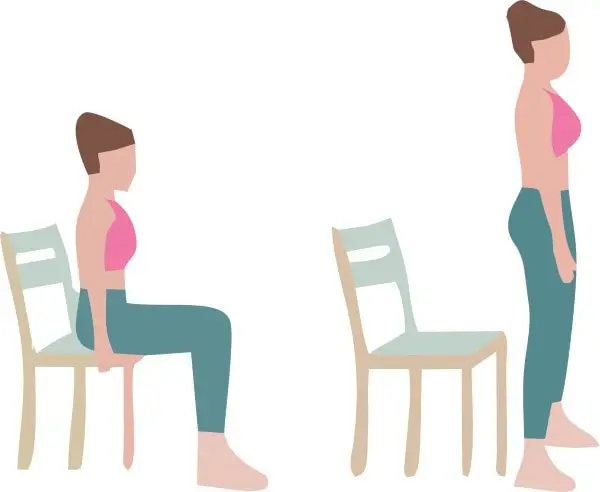
- Get Up and Sit The purpose of this exercise is to increase lower extremity strength and balance during functional sit-to-stands.
- Position your feet under your knees, hip-distance apart, while seated. Your entire body should be in front of the chair as you sitting up upright.
- Use the muscle in your legs to propel yourself up into a standing position as your weight shifts to your feet.
- After ten repetitions, return to the chair by sitting down. Steadily and slowly perform this; do not use your arms as support.

Weight shifting in sitting
- Sit upright on chair with your feet under your knees and your hips apart (on an exercise ball is more challenging).
- Get started by easily and comfortably moving your upper body to the right, subsequent to the left.
- Provide equal side-to-side weight glide for your trunk.
- Perform ten repetitions.
- The main goals of this workout are balance and core stability.
Weight shifting in standing

- This exercise improves balance and prepares the body for sidestepping and twisting. The feet should be spaced at least hip-width apart when standing.
- As you slowly begin to lateralize your weight, rotate your head, shoulders, hips, and trunk onto one foot.
- It is necessary to perform this side-to-side shifting action ten times.
Forward-backward weight shifting
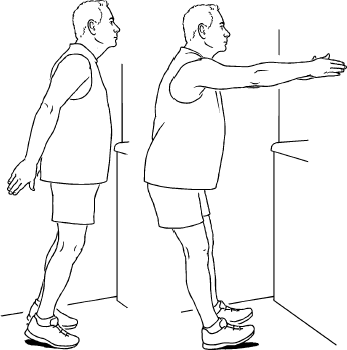
- Walking preparation is achieved by the use of balance exercises like the standing anterior-posterior weight shift.
- When standing, spread your feet hip-width apart or wider. Initialize by transferring all of your weight to your toes and then back to your heels gently.
- Repeat this shifting motion forward and backward ten times.
One-leg stand

- This exercise focuses on balancing with a tiny base of support and is functionally related to walking and transfers (e.g., getting in and out of a bathtub).
- Begin by standing up straight and distributing your weight onto one leg. Then, without letting the second leg touch the standing leg, raise it off the ground.
- Try to stay balanced for longer periods of time while standing on one leg. After dropping the lifted leg, carry on on the reverse side.
FAQs
Does physical therapy work for ataxia?
Patients with ataxia may participate more in activities thanks to physiotherapy’s reduction of activity restrictions and enhancement of gait, balance, and trunk control. Consideration must be given to fall prevention in individuals with progressing ataxia due to the frequency of falls and the high incidence of injuries resulting from them.
Is ataxia a prevalent a medical condition?
One symptom that comes up often is ataxia. Less commonly occurring and typically only occurring in connection with particular inherited ailments and diseases is ataxia.
Is it possible for someone with ataxia to walk?
A class of neurological disorders known as ataxia is typified by a chaotic appearance of motor behavior. Individuals suffering from ataxia may display irregularities in tasks necessitating precise motor control, like walking, speaking coherently, swallowing, writing, and reading.
How can an ataxic gait be fixed?
The basic treatments for ataxia include neuromotor exercises and physical therapy focused on balance and coordination, which have been demonstrated to improve or prevent the progression of functional deterioration.
References
Patel, D. (2023a, April 24). Ataxic Gait – Type, Cause, Symptoms, Treatment, Exercise. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/ataxic-gait/
Team, P. (2020, September 21). Common Gait Deviations: Ataxic Gait » ProtoKinetics. ProtoKinetics. https://protokinetics.com/common-gait-deviations-ataxic-gait/
Mohamed, O., & Appling, H. (2020). Clinical Assessment of Gait. In Elsevier eBooks (pp. 102–143). https://doi.org/10.1016/b978-0-323-60913-5.00005