Cervical Spondylosis and Myelopathy
Cervical Spondylosis with Myelopathy is a condition where age-related degeneration of the cervical spine leads to compression of the spinal cord. This can cause symptoms like neck stiffness, numbness or weakness in the arms and legs, coordination difficulties, and even balance issues.
It is a progressive disorder and requires early diagnosis and appropriate treatment to prevent long-term neurological damage.
Introduction
Age-related wear and tear narrows the spinal canal in the neck (cervical spine), compressing the spinal cord and resulting in cervical spondylotic myelopathy (CSM). Numbness, clumsiness, hand and arm weakness, and trouble balancing are just a few of the symptoms that can result from this compression. According to the Journal of the American Board of Family Medicine, it is the most frequent reason for spinal cord dysfunction in elderly individuals.
- Cervical osteophytes, or bone spurs, at the vertebral borders are the most prevalent manifestation of normal age-dependent alterations of the intervertebral discs.
- Facet hypertrophy, or expansion of the facet joints, is caused by arthritis in the neck.
- Reduction in disc height accompanied by thickening of the ligaments surrounding the spinal canal, particularly the ligamentum flavum.
- Partial dislocation or subluxation of the vertebral bodies as a result of translational mechanical instability.
- Cervical spondylosis is the basis for cervical spondylotic myelopathy.
- CSM does not develop in all cases of cervical spondylosis. Only when the spinal cord is crushed does CSM happen.
Cervical spondylosis

A condition known as cervical spondylosis is the general term for age-related wear and tear on the spinal disks in your neck. Osteoarthritis symptoms, such as bony protuberances along the margins of bones (bone spurs), appear as the disks dry up and shrink.
A degenerative disorder of the neck (cervical spine), cervical spondylosis is mostly caused by aging-related wear and tear. The spinal discs and vertebrae may degenerate, causing pain, stiffness, and nerve compression. The symptoms of this disease range from little pain to more serious problems like nerve pain, numbness, or even weakness in the arms or legs. It is particularly frequent in elderly persons.
A frequent condition that becomes worse with age is cervical spondylosis. More than 85 percent of adults over 60 have cervical spondylosis. Cervical spondylosis rarely manifests any symptoms. Nonsurgical treatments are frequently effective when symptoms do show up.
Symptoms
The majority of people don’t have any symptoms. When symptoms do appear, neck pain and stiffness are usually among them.
The spinal canal, which travels through the vertebrae, may narrow as a result of cervical spondylosis on occasion. A cavity inside the vertebrae called the spinal canal is where the spinal cord and nerve roots pass to reach the rest of the body. If the nerve roots or spinal cord are compressed, the following symptoms may appear:
- A common symptom is neck pain and stiffness, which can range from mild to severe and get worse when you move or do particular things.
- Headaches: Headaches are another common condition, particularly those that start at the back of the head.
- Shoulders, Arms, and Sometimes Even Fingers: Pain can radiate from the neck to the shoulders, arms, and occasionally even the fingers.
- Sensations of numbness, tingling, or “pins and needles” in the hands and arms might result from spondylosis-induced nerve compression.
- Muscle Weakness: Hand and arm weakness may be caused by nerve compression.
- Restricted Mobility: Difficulty rotating or bending the neck is another common symptom.
- Dizziness and Balance Issues: Cervical spondylosis can occasionally impair coordination and balance, resulting in vertigo or dizziness.
- Grinding or Popping Sensations: When rotating their neck, some people may hear or feel popping, clicking, or grinding sounds.
Causes
This comprises the cervical spine’s joints between the bones as well as the cushions or disks that lie between the neck’s vertebrae. Spurs or abnormal growths may be present in the vertebrae (bones of the spine).
One or more of the nerve roots may eventually be compressed by these alterations. The spinal cord is affected in more severe cases. Your arms, legs, and equilibrium may be impacted by this. These alterations may be caused by normal wear and tear. They might be more common among people who are highly engaged in sports or at work.
Aging is the main risk factor. X-rays show cervical spondylosis in most adults by the age of 60. The following additional variables may increase a person’s risk of developing spondylosis:
- Being overweight and not exercising.
- Working in an occupation that involves a lot of bending and twisting or heavy lifting.
- Past neck injury (often several years before)
- Past spine surgery
- Ruptured or slipped disk
- Severe arthritis
- Previous surgery on the neck
Risk Factors
Age is the main cause of cervical osteoarthritis, commonly referred to as cervical spondylosis. The disks between the vertebrae in the majority of adults over 50 lose their sponginess and cushioning ability. The space of the spinal canal is affected by the thickening of bones and ligaments.
Among them are:
- History of cervical spondylosis in the family. It may be a genetic issue.
- A neck injury or trauma. Your cervical disks and ligaments may potentially be impacted if you have previously suffered neck injuries.
- Employment, way of life, or pastime. You must repeatedly move your neck in the same way for certain jobs, pastimes, or sports. Or they might make you glance up a lot or for extended periods. This may put strain on the ligaments and disks in the neck.
- Smoking. Smoking is associated with neck pain.
- Depression. Researchers have discovered that those who suffer from depression are more likely to develop cervical spondylosis.
- Bad posture. Your cervical disks and ligaments’ long-term health is impacted by the way you hold your head when you stand or sit.
Cervical Myelopathy
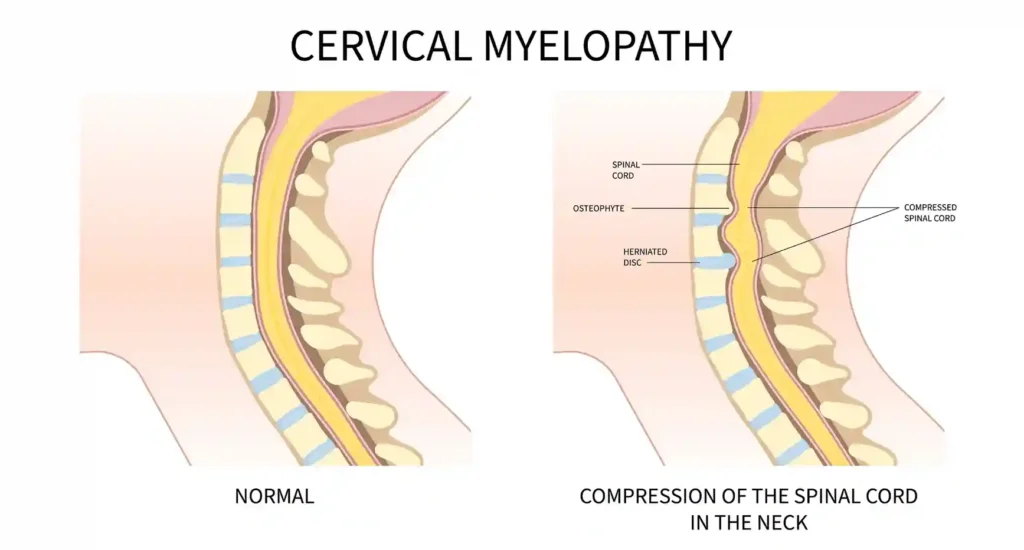
The most prevalent kind, cervical spondylotic myelopathy, results from aging-related physiological changes. It can cause several symptoms, including neck pain, muscle weakness, and numbness. Cervical myelopathy is treated with surgery.
A disorder called cervical myelopathy occurs when the spinal cord in the neck becomes compressed, frequently as a result of other spinal problems or aging-related wear and tear. A variety of symptoms, such as stiffness, numbness or tingling in the hands and arms, neck pain, clumsiness, and abnormalities in gait, can result from this compression. Untreated cervical myelopathy can worsen and result in paralysis and other serious neurological issues.
Cervical myelopathy: what is it?
Functional deficits and a variety of neurological symptoms may result from this compression. It may occur if that area of your spinal cord is compressed by an accident, a tumor, or a herniated disk.
Everybody has mornings when they wake up with neck pain or stiffness. Pain from cervical myelopathy is persistent. It might cause your hands to become numb or weak.
To avoid complications, a medical professional may recommend treatments such as spinal cord decompression surgery.
Symptoms
Signs of cervical spondylotic myelopathy and cervical myelopathy include the following:
- Neck stiffness or pain.
- Your arms and hands may feel tingly or numb.
- Weakness in your arms and hands.
- Walking difficulties and loss of balance.
Causes
Compression or pressure on the spinal cord in the neck area results in cervical myelopathy. Typical reasons for compression include:
- Bone spurs.
- Herniated disk.
- Narrow cervical canal (birth defect).
- Rheumatoid arthritis.
- Spondylolisthesis.
- Spinal degeneration.
- Spinal stenosis.
- Traumatic injury.
- Tumor.
Age-related changes that impact the structure and function of certain neck spine segments (spinal degeneration) might result in cervical spondylotic myelopathy. Your spinal cord is compressed as a result of these alterations because they restrict the spinal canal, which is the opening where it rests. Degenerative alterations are a normal aspect of aging.
Risk factors for cervical myelopathy
Any age can be affected by cervical myelopathy. Studies show that it is more common in Asian Americans over thirty. Although anyone can get cervical spondylotic myelopathy, men and individuals over 40 are more likely to get it.
Complications of cervical myelopathy
Cervical myelopathy symptoms could worsen if treatment is not provided. This might cause:
- Severe pain.
- Bowel and bladder dysfunction.
- Nerve damage.
- Difficulty walking (instability, high risk of falls).
- Restricted use of your arms, hands, and fingers.
- Paralysis.
Diagnosis and Tests
Cervical myelopathy will be diagnosed by a medical professional following a neurological examination, physical examination, and other tests. During the evaluation, your physician will review your symptoms and medical history. To learn more about how symptoms impact you, they might also evaluate your reflexes, balance, and dexterity and, if feasible, watch you walk.
To examine your spine, your doctor could prescribe imaging tests. Imaging examinations could consist of:
- X-ray.
- MRI.
- CT scan.
- Myelogram.
Treatment
Every day chores and even sleeping might be challenging when you have neck pain. However, there are a few things you may take to improve your sleep quality and continue with your everyday activities.
Exercises to treat cervical spondylosis
Certain exercises can help you utilize your neck more effectively and reduce the pain associated with cervical spondylosis. Before beginning any new exercises, consult your physician unless your physical therapist has prescribed them. Listen to your body as well.
Unless your doctor has warned you not to, you can try these kinds of workouts. Don’t do more than one or two repeats at first. Repeat the exercises throughout the day, progressively increasing the number of repetitions, if they don’t worsen your pain and you feel comfortable doing so.
Head turn
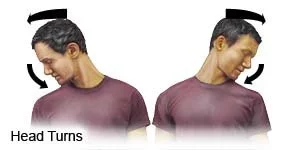
- Look directly forward. Turn your head slowly to one side until you feel the opposite side extend. Avoid pushing your head any further.
- For two seconds, maintain this posture.
- Return to the center slowly, then do the opposite turn. Return to the center after holding the posture once more.
Head tilt
- Look directly forward. As much as you can, slowly tilt your head to one side and toward your shoulder until it is no longer comfortable. The other side of your neck ought to feel stretched.
- Hold for two seconds.
- Bring your head back to the erect posture slowly.
- Continue on the opposite side.
- Go back to the middle.
Forward head tilt

- Look directly forward.
- Bring your chin down to your chest slowly, as if you were nodding.
- Raise your head back to the front.
Wide shoulder stretch
- Look directly forward.
- After letting your arms hang on each side, bend your elbows to a straight angle.
- Keep your hands facing the ceiling with your palms facing up.
- Move your hands and lower arms outward while keeping your elbows by your sides, without moving your upper arms. Align your right hand with the right and your left with the left.
- Hold for a short while.
Prevention for Cervical Spondylosis
Many people suffer from a disorder called cervical spondylosis, which is caused by wear and strain on the neck. Cervical spondylosis can be prevented or lessened by taking care of your neck due to certain risk factors, such as previous neck traumas. Here are some pointers:
- Keep your neck safe. Use the appropriate safety gear if you engage in neck-harming activities. Regardless of how minor the collision, make sure the headrest is at the right height while you’re driving to protect your neck.
- This implies that you should avoid jerking your head back and forth or straining your neck.
- Avoid repetitive gestures like reaching up and glancing up.
- Get moving and continue to be active.
Treatment for cervical myelopathy
A cervical collar brace and physical therapy are two nonsurgical alternatives for reducing the symptoms of cervical myelopathy. To remove the spinal cord compression and stop the problem from getting worse, surgery is frequently required.
To treat cervical myelopathy, your doctor could suggest a few surgical techniques. For certain patients, laminoplasty, or spinal canal widening, may be a beneficial motion-preserving procedure. To stabilize the spine following the whole or partial removal of herniated discs, bone spurs, or ossified ligaments, others may benefit from spine decompression surgery combined with spinal fusion.
These procedures can be carried out anteriorly (from the front of the neck) or posteriorly (from the back of the neck). Depending on your circumstances, your doctor will suggest a certain surgical strategy.
Cervical myelopathy can be treated in two ways, including:
- Nonsurgical management.
- Surgical treatment.
Depending on how severe the symptoms are and what’s causing them, your doctor may begin with nonsurgical methods before considering surgery.
Nonsurgical cervical myelopathy management
They could consist of:
- Wearing a neck brace.
- Participating in physical therapy.
- Taking medications.
If you must take medicine, you can manage certain symptoms with the following options:
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Corticosteroids.
- Pain relievers.
Though it doesn’t widen a narrow spinal canal or offer long-term comfort, nonsurgical treatment manages symptoms right away.
Surgical cervical myelopathy treatment
- Severe pain.
- Muscle weakness.
- Numbness.
- Balance and walking challenges.
- Difficulty with fine motor skills.
A surgeon’s recommended procedure may change depending on your age, general health, and symptoms. It could consist of one or more of the following:
- Diskectomy.
- Disk replacement.
- Spinal fusion.
Laminectomy. To make more room for the spinal cord, a laminectomy entails removing a portion of the lamina, or the back portion of the vertebra. A laminectomy is a surgical technique used to relieve pressure on the spinal cord or nerves. It includes removing all or part of the lamina, a bony structure that forms the rear of the spinal canal. Treatment for spinal stenosis, herniated discs, or bone spurs that compress the spinal cord or nerve roots frequently involves this operation.
Laminoplasty. The purpose of laminoplasty is to enlarge the spinal canal by making a hinge on one side of the lamina and holding it open with a plate or bone. To decompress the spinal cord and nerves, laminoplasty aims to expand the space inside the spinal canal. Laminoplasty can prevent fusion (which can result in neighboring segment disease), maintain neck motion, and possibly lower the risk of problems following laminectomy.
Posterior Cervical Fusion. This technique stabilizes the spine by joining vertebrae from the rear of the neck, frequently utilizing screws and rods.
Corpectomy. A corpectomy occurs when a vertebral body and disc are removed, and the remaining vertebrae are fused.
Anterior Cervical Discectomy and Fusion (ACDF): This procedure stabilizes the spine by removing a diseased disc and joining the vertebrae.
Before the treatment, your surgeon will go over the potential hazards with you so you can make an informed decision regarding your health. Following surgery, you will need to rest and recuperate. Until your provider gives the all-clear, stay away from intense activities and heavy lifting. You will receive detailed instructions from your surgeon regarding self-care and when to schedule a follow-up appointment.
Prognosis for cervical myelopathy
The cause will determine your cervical myelopathy prognosis. The results of surgical treatment are often favorable in mild cases of cervical myelopathy that improve with nonsurgical treatments.
Ignoring cervical myelopathy can make it worse. Severe cases may result in irreparable, permanent nerve damage, which can cause problems including excruciating pain and trouble moving. The source, intensity, and duration of symptoms, as well as the treatment strategy used, all affect the prognosis for myelopathy, which causes spinal cord dysfunction. In general, better results come from early diagnosis and treatment because prolonged compression can cause irreversible nerve damage.
If you experience any cervical myelopathy symptoms, notify a healthcare professional immediately. They can assist you in determining the best course of action for your life.
Conclusion
Although it is a degenerative disorder, cervical spondylosis is not lethal. You can avoid cervical spondylosis or delay its progression by being aware of your risk factors. With an early diagnosis, you and your physician can monitor its progression and manage it.
A patient’s quality of life can be greatly impacted by myelopathy, a disorder caused by spinal cord compression or damage that frequently results in increasing neurological impairments. Many myelopathy patients need surgery, such as decompression surgery, to relieve spinal cord compression and stop more neurological damage; however, some cases may be successfully treated with conservative measures like physical therapy. To maximize results and reduce the chance of irreversible damage, early diagnosis and timely treatment are essential.
FAQs
How quickly does cervical myelopathy develop?
The cause of your symptoms will determine this. It could occur suddenly following an injury, for instance, or develop gradually as you become older. Based on your symptoms and any recommended imaging tests, your healthcare provider is going to determine how quickly things will progress and how likely it is that you will experience consequences.
What are the worst symptoms of cervical spondylosis?
Severe muscle weakness, trouble walking or keeping balance, and loss of bladder or bowel control are some of the most severe symptoms of cervical spondylosis. These signs point to spinal cord compression and the need for emergency care. Numbness and tingling that spreads to the arms and legs, as well as pain that travels from the neck to the arms or shoulders, are additional severe symptoms.
What is the most recent spinal stenosis treatment?
Endoscopic spine surgery, a minimally invasive method that uses a high-definition camera and specialized tools to access the spine through a small incision, is the most recent treatment for spinal stenosis. Compared to open surgery, this method seeks to minimize postoperative pain, limit tissue damage, and hasten healing. Acupotomy, stem cell therapy, and lumbar interspinous distraction devices are other cutting-edge therapies.
Can the brain be affected by cervical spondylosis?
Although cervical spondylosis mostly affects the neck and spine, there are a few ways in which it can also have an indirect impact on the brain. Changes in brain structure and function, such as decreased gray matter volume in certain regions, altered activity in sensorimotor and default mode networks, and possible effects on cognitive and affective functioning, can result from cervical spondylosis.
Can someone with cervical spondylosis live a long life?
The majority of cervical spondylosis patients experience some chronic symptoms. Surgery is not necessary for the majority of these problems, which improve with non-surgical treatment. A lot of people who have this issue manage to lead active lives. Some people will have to endure chronic pain for the rest of their lives.
Which exercises are ideal for those with cervical spondylosis?
Gentle neck stretches and strengthening exercises like shoulder blade squeezes, neck tilts, and retractions, along with cardiovascular workouts like walking, are the ideal exercises for cervical spondylosis. The goals of these exercises are to strengthen the muscles around the neck, decrease pain, and increase neck mobility.
Which cervical spondylosis symptoms are the worst?
Severe muscle weakness, trouble walking or keeping balance, and loss of bladder or bowel control are some of the most severe symptoms of cervical spondylosis. These signs point to spinal cord compression and the need for emergency care. Numbness and tingling that spreads to the arms and legs, as well as pain that travels from the neck to the arms or shoulders, are additional severe symptoms.
Reference
- Cervical myelopathy (Cervical spondylotic myelopathy). (2025, June 2). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/cervical-myelopathy
- Cervical spondylosis – Symptoms & causes – Mayo Clinic. (2023b, December 20). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/cervical-spondylosis/symptoms-causes/syc-20370787
- Facs, T. W. M. (2012, November 29). Cervical Spondylosis with Myelopathy. Spine-health. https://www.spine-health.com/conditions/neck-pain/cervical-spondylosis-myelopathy
- Cervical spondylosis: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/000436.htm