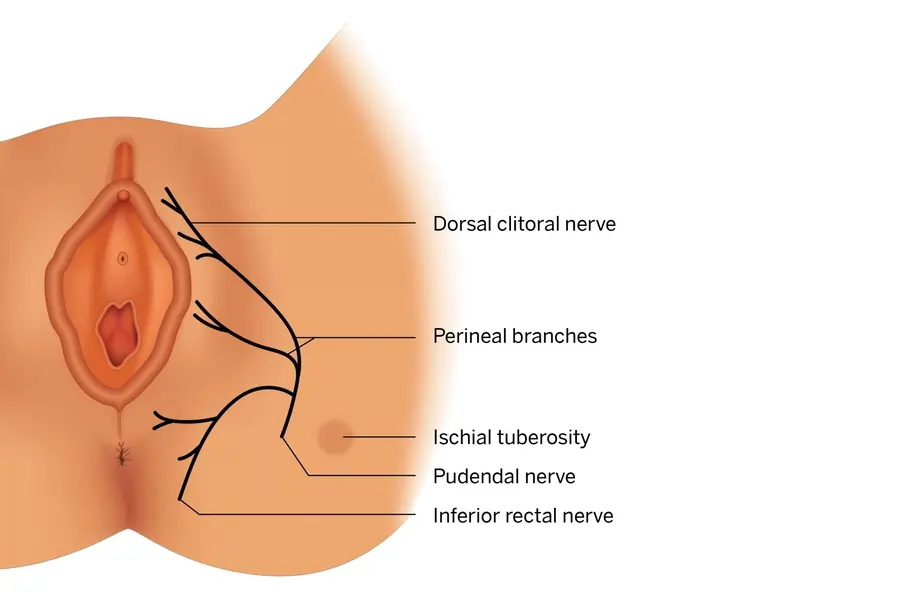
Pudendal Nerve
Introduction
The pudendal nerve is a major nerve in the pelvis, originating from the sacral plexus (S2-S4). It provides motor and sensory innervation to the perineum, including the external genitalia, anus, and pelvic floor muscles. It plays a key role in controlling bladder and bowel function, as well as sexual function. Injury or irritation of the pudendal nerve can lead to conditions like pudendal neuralgia, causing pelvic pain and dysfunction.
The pudendal nerve’s primary work is to give sensory information to the skin around the anus, anal canal, and perineum as well as the external genitalia in both sexes. Additionally, it supplies motor power to the external urethral sphincter, external anal sphincter, and other pelvic muscles.
Course
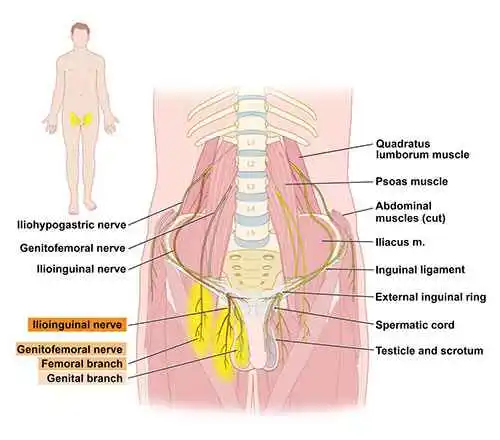
Along with the sciatic nerve, the pudendal nerve is one of the two primary branches that emerge from the sacral plexus. It appears in the pelvis along the upper border of the ischiococcygeus muscle and sacrotuberous ligament. The larger sciatic foramen is where the nerve exits the pelvis after traveling inferiorly. The nerve travels dorsal to the sacrospinous ligament and medial to the internal pudendal veins after exiting the foramen and entering the gluteal area.
The pudendal nerve enters the pudendal canal (Alcock’s canal) through the smaller sciatic foramen, accompanied by the internal pudendal artery and vein as well as the nerve to the obturator internus. The pudendal neurovascular bundle is the collective term for the pudendal artery, vein, and nerve.
When the pudendal nerve enters the canal, it gives rise to the inferior anal nerve, also known as the inferior rectal nerve, which innervates the perianal skin and the external anal sphincter. The perineal nerve and the dorsal nerve of the penis/clitoris are the two additional branches that emerge when the nerve reaches the distal part of the canal.
Function
Both sensory and motor (muscle) activities are performed by the pudendal nerve. Additionally, sympathetic autonomic fibers—but not parasympathetic ones—are carried by it.
Sensory
The pudendal nerve, which passes via the branches of the dorsal nerves of the clitoris and penis, provides feeling to the clitoris in females and the penis in males. The posterior scrotal nerves in men and the posterior labial nerves in females supply the posterior scrotum in males and the labia majora in females, respectively.
These regions get sensations from several nerves, including the pudendal nerve. Branches also provide the anal canal with feeling. The afferent component of penile erection and clitoral erection is caused by the pudendal nerve, which supplies feeling to the penis and the clitoris.
Motor
Muscles of the pelvic floor and perineum are innervated by branches, including the levator ani muscle (which includes the puborectalis, pubococcygeus, iliococcygeus, and either pubovaginalis in females or puboprostaticus in males), the external anal sphincter (through the inferior anal branch), the male or female external urethral sphincter, and the bulbospongiosus and ischiocavernosus muscles, respectively.
Because it innervates the external urethral sphincter, it controls the sphincter’s tone through the release of acetylcholine. This indicates that urine retention results from the skeletal muscle in the external urethral sphincter contracting during times of elevated acetylcholine release.
On the other hand, the skeletal muscle of the external urethral sphincter relaxes during times of reduced acetylcholine release, enabling bladder voiding. (The somatic nervous system controls the external sphincter voluntarily since it is composed of skeletal muscle, in contrast to the internal sphincter muscle.)
Branches
Three branches emerge from the pudendal nerve:
- Inferior anal nerve
- Perineal nerve
- Dorsal nerve of the penis/clitoris
Inferior anal nerve
The first of the pudendal nerve’s three branches is often the inferior anal nerve, commonly referred to as the inferior rectal nerve or inferior haemorrhoidal nerve. In the pudendal canal, it usually branches from the pudendal nerve, however in certain people, it may originate straight from the sacral plexus.
When it rises, it leaves the canal and passes through the ischioanal fossa’s fat to arrive at the anal canal’s lateral aspect. The inferior anal nerve is a mixed nerve that supplies motor function to the external anal sphincter and sensory function to the inferior part of the anal canal (to the pectinate line) and the circumanal skin. In addition, the inferior anal nerve may offer sensory innervation to the lower region of the vagina in females.
Perineal nerve
The second and biggest of the pudendal nerve’s three branches is the perineal nerve. It usually appears right before the pudendal nerve leaves the canal or in the last section of the canal. The deep (muscular) and superficial (cutaneous) perineal nerves are the two branches of the perineal nerve.
The external urethral sphincter, the front portions of the external anal sphincter, the levator ani, and the urogenital triangle’s muscles (bulbospongiosus, ischiocavernosus, and superficial transverse perineal muscle) are all supplied by the deep branch.
The posterior scrotal region in men, the labia minora, the vaginal vestibule, the bottom fifth of the vaginal canal, and the rear portion of the labia majora in females are all sensory-supplied by the superficial branch.
Dorsal nerve of the penis/clitoris
The pudendal nerve’s terminal branch is thought to be the dorsal nerve of the penis/clitoris. As the only sensory origin for the external genitalia, the dorsal nerve of the penis/clitoris is essential to preserving healthy sexual function. More precisely, this nerve innervates the skin over the prepuce, glans, and shaft of the penis in men. The glans and clitoral bodies in females are innervated by the dorsal nerve of the clitoris.
Anatomical Importance
The pudendal nerve and its branches exhibit significant anatomical diversity, as is the case with many other nerves. There are irregularities in the number of branches, size, particular routes, and innervated structures. There are frequently many variances found, even in research with a limited number of cadavers.
The ventral rami of S1 or S5 are among the extra contributions that contribute to the pudendal nerve in certain individuals. Furthermore, the routes and tissues innervated by the pudendal nerve’s primary branches vary. Frequently, even more branches are discovered, giving structures redundant innervations. These variances may cause individuals with pudendal nerve diseases to present differently.
Examination
Although it is challenging to see the pudendal nerve on standard CT or MR imaging, a needle may be positioned next to the pudendal neurovascular bundle with CT guidance. The injection site is the ischial spine, which is a readily recognized feature in CT. Within a few millimeters of the ischial spine, a spinal needle is advanced into the gluteal muscles. After that, an injection of contrast (X-ray dye) is given to highlight the nerve in the canal and verify that the needle was inserted correctly.
Cortisone and a local anesthetic may then be injected into the nerve to confirm and treat persistent discomfort in the external genitalia, pelvis, and anorectum (known as vulvodynia in females).
Pain Assessment
- The patient experiencing pelvic discomfort, particularly in the vaginal and perineal areas, with or without accompanying symptoms related to the bowel, bladder, or sex
- the gradual development of pain, excluding severe injuries
- Morning pain is less severe, and as the day goes on, it gets worse
- The most common type of pain is burning pain, although it can also be tingly, aching, stabbing, or shock-like.
- Sitting exacerbates pain, but standing, lying down, or sitting on a toilet relieves it.
- The vulva, vagina, clitoris, perineum, and rectum in females, and the glans penis, scrotum, perineum, and rectum in men, can all be affected by pain, which can be localized or widespread.
- Urinary urgency, frequency, and symptoms that resemble interstitial cystitis are also linked to PN.
- Other symptoms include dyspareunia, painful nocturnal orgasms, painful ejaculation, and prolonged sexual excitement
- Foreign body sensation
Clinical Importance
It is possible to identify patients with pudendal nerve injury by looking at their medical history and current symptoms. Neuropathy is usually observed in the pudendal nerve distribution. These injuries may result from pelvic trauma, problems during delivery, persistent discomfort, or even iatrogenic injuries after pelvic surgery or radiation therapy. Fecal/urinary incontinence, numbness, sexual dysfunction, and persistent discomfort are other symptoms. Pudendal nerve injuries can happen during delivery.
The pudendal nerve’s route makes it susceptible to strain damage during childbirth. These injuries are more likely to occur in mothers who give birth to children who weigh more than usual. After giving birth, patients may have urine and/or fecal incontinence. In these birth-related pudendal nerve injuries, the nerve usually recovers its normal function on its own.
The uncommon syndrome known as pudendal nerve entrapment or pudendal neuralgia can be caused by any type of chronic pressure near the ischial spine, and it has been observed to occur in professional cyclists as a result of repeated irritation from the bicycle seat pressing the pudendal nerve against the ischial spine or the sacrospinous ligament.
Patients with pudendal neuralgia typically experience bilateral perineal pain that is worse when they sit, and the pain may be progressive and result in discomfort that is relatively resistant to treatment, but in some patients, it can be incapacitating and severe. After seeing several doctors, people with pudendal neuralgia sometimes endure months or years of futile therapies before receiving a diagnosis. Sitting with perineal discomfort should be regarded as a common symptom of this illness.
To do a pudendal nerve block, a local anesthetic is injected close to the pudendal nerve. Pudendal nerve entrapment can be diagnosed with the use of this method. For women who cannot get spinal anesthesia, it can be used to relieve discomfort during obstetric operations, particularly after labor.
To temporarily stop nerve conduction, a single injection is given next to the pudendal nerve to complete the block. The ischial spine serves as a reference during these surgeries to help ensure that the anesthetic is administered in the proper spot. This is because the pudendal nerve wraps around the sacrospinous ligament, which brings it close to the ischial spine.
Surgical Importance
It is crucial to take into account the possibility of iatrogenic injury to the pudendal nerve before performing pelvic surgery. During obstetrical, perineal, and proctological operations, the risk of pudendal nerve damage is very significant.
Numerous operations, including radical prostatectomy, exploratory surgery, tumor removal, and cesarean sections, have been known to cause injury. To avoid iatrogenic harm, it is essential to comprehend the pudendal nerve’s overall structure and any potential deviations before performing surgery in the area.
FAQs
What are the symptoms of pudendal nerve problems?
Sharp, shooting, burning, or tingling pain (nerve pain) or numbness in your genitals (your vagina, vulva, and clitoris, or penis and scrotum), bottom, and anus are the primary symptoms of pudendal neuralgia. The space between your genitalia and anus is called the perineum.
Can sitting too much cause nerve damage?
Sitting too much can cause nerve damage, including pinched nerves, sciatica, and peripheral neuropathy.
Causes
Pinched nerves
Also known as radiculopathy, this can occur when sitting puts pressure on nerves in your lower back, neck, legs, or wrists.
Sciatica
A general term for pain that radiates down the leg, often caused by chronic sitting.
Peripheral neuropathy
A general term for nerve damage that can cause weakness, numbness, and pain, usually in the hands and feet.
Symptoms
Tingling, burning, or numbness in the limbs or extremities
Paralysis, lack of muscular strength, or unexplained weakness
Persistent headaches, come on suddenly, or are “different”
Problems with coordination
Tips to prevent nerve damage Maintain good posture, Take breaks to stand or stretch, Use an ergonomic chair, Consider a standing desk, and Take short walks every 30 minutes.
Treatment Resting the affected area until it’s healed, Regular checkups with a healthcare professional, and Applying cold and heat therapy.
How to test for pudendal nerve damage?
Among the assessments that providers employ are:
During a vaginal or rectal exam, medical professionals apply pressure on your pudendal nerve by inserting a gloved finger into your rectum or vagina.
A potent imaging technique that can examine your pudendal nerve and the surrounding tissues to find problems is magnetic resonance imaging (MRI).
Can a gynecologist treat the pudendal nerve?
Given the limited expertise most gynecologists will have with these surgical techniques, it may be prudent to send a patient to a specialist, especially for pudendal nerve release operations.
Is massage good for the pudendal nerve?
As the pudendal nerve passes via pelvic soft tissue structures including the piriformis and coccygeus muscles, compression may be relieved by deep tissue massage and soft tissue mobilization.
How long does the pudendal nerve last?
What is the duration of a pudendal nerve block? For people with persistent pelvic discomfort, a pudendal nerve block can provide varying degrees of pain relief. It might go on for a few days, weeks, months, or even years.
References
- Pudendal nerve. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/pudendal-nerve
- Wikipedia contributors. (2025, February 9). Pudendal nerve. Wikipedia. https://en.wikipedia.org/wiki/Pudendal_nerve
- Pudendal nerve. (2023, February 10).StatPearls.https://www.ncbi.nlm.nih.gov/books/NBK554736/

One Comment