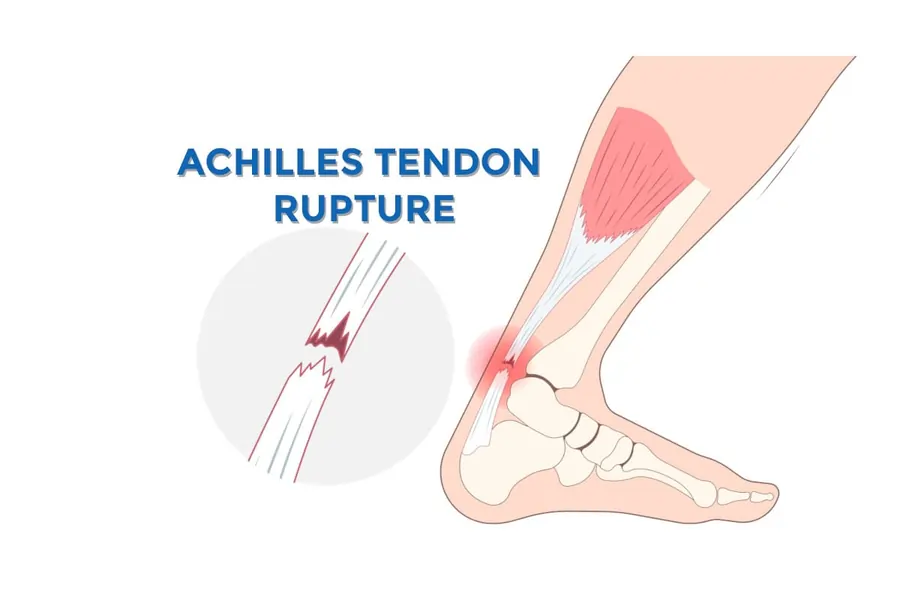
Achillis Tendon Rupture
What is a Achillis Tendon Rupture?
An Achilles tendon rupture is a complete or partial tear of the Achilles tendon, which connects the calf muscles to the heel bone. It often occurs during activities that involve sudden acceleration, jumping, or pivoting.
The most frequent tendon rupture in the lower limb is the Achilles tendon. Adults in their third or fifth decade of life are most likely to sustain the damage. Acute ruptures frequently manifest as an abrupt start of pain accompanied by a “pop” or “snapping” sound at the location of the lesion. The feeling of being kicked in the lower leg might be described by patients. Significant pain and incapacity result from the damage.
Achilles tendon injuries are most common in those who are intermittently active (sometimes known as “weekend warrior” athletes) and are most commonly sustained when playing basketball, soccer, or racket sports. According to reports, 20% to 25% of people have these injuries misdiagnosed as ankle sprains.
The third to fifth decade of life is the age range most frequently impacted by Achilles tendon injury. Ten percent or so of patients say they had prodromal symptoms prior to the accident. Inflammatory arthritis, fluoroquinolone usage, steroid injections, and previous intratendinous degeneration (such as tendinosis) are other known risk factors.
Anatomy of Achillis Tendon
Two tendinous segments make up the Achilles tendon. A single, homogeneous tendon is generated by the gradual merger of two tendon sites, one proximally and the other distally. It is made up of three muscle heads: the soleus is monoarticular, while the gastrocnemius and plantaris are biarticular. The mechanical load on the tendon is concentrated in two places. These are the medial or center region of the paratenon and the middle length of the tendon, which is the most often damaged location.
As it descends from its origin, the Achilles tendon twists 90 degrees, clockwise on the left and counterclockwise on the right. Consequently, smaller soleus fibers enter anteromedially, whereas larger gastrocnemius fibers insert posterolaterally.
This configuration is thought to affect the pathophysiologic mechanisms of Achilles tendinopathies and alter the biomechanics of the tendon.
In insertional Achilles tendinopathy, the hallmarks of tendon degeneration include capillary development, fatty infiltration, and the loss of strong parallel collagen I fibers. This will be discussed in more depth in the next sections, and it will show up as a thickening of the tendon in advanced imaging.
Epidemiology
According to current research, there can be up to 40 Achilles tendon ruptures per 100,000 individuals per year, however the prevalence varies throughout the literature. It is believed that the substantial rise in ruptures during the last ten years is related to the rise in the number of people participating in sports, especially those over thirty. Men between the ages of three and four account for seventy-five percent of ruptures during recreational activities.
Over 20% of ruptures are misdiagnosed, however the actual prevalence of Achilles tendinosis is unclear. The incidence rates among athletes are reported to be less than 1% for American football players, 7% to 18% for runners, 9% for dancers, 5% for gymnasts, and 2% for tennis players. An estimated 1 million sportsmen suffer from Achilles issues each year.
Pathophysiology of Achilles tendon rupture
Achilles tendon ruptures are caused by a combination of biomechanical, structural, and mechanical variables.
Mechanical factors: Because of its structure, the Achilles tendon is the strongest tendon in the body. It twists clockwise on the left and counterclockwise on the right as it descends from its starting point, completing a full round.
The Achilles tendon is mostly made up of thick, parallel type 1 collagen fibers arranged in fascicles. Parallel collagen fibers become less ordered and more prone to degradation as people age. Furthermore, several illnesses can weaken the tendon’s structural integrity and raise the risk of rupture, including diabetes and chronic renal disease.
Biomechanical considerations: High foot arches reduce the likelihood of Achilles injuries, but stiffness is linked to possible risk factors for Achilles injuries. Tendon fiber degradation and possible rupture can result from biomechanical factors and a limited blood supply when the tendon is subjected to repetitive microtrauma or chronic stress.
Usually, 2 to 6 cm above the calcaneal insertion, the Achilles tendon ruptures. Its tendon fibers twist in this location, and the blood flow is reduced. Research has shown that microperfusion and capillary oxygenation are lower at 5 cm above the calcaneal tubercle than at 1 cm above the tendon insertion.
Causes of Achillis tendon rupture
Achilles tendon rupture can be caused by direct trauma, prolonged tendinopathy, or intratendinous degenerative diseases, as well as abrupt forceful plantar flexion of the foot. Racquetball, basketball, and soccer are among the sports that are frequently linked to Achilles tendon rupture. Poor pre-exercise conditioning, long-term corticosteroid usage, overexertion, fluoroquinolone antibiotics, oral bisphosphonates, prior Achilles tendinopathy, diabetes, hyperparathyroidism, and hereditary variables are risk factors for Achilles tendon rupture.
Due to a number of reasons, end-stage renal disease (ESRD) is also strongly linked to a risk of Achilles tendon rupture. Before or after a kidney transplant, this demographic group is frequently administered corticosteroids and fluoroquinolones. Weekly dialysis done by ESRD also causes a number of metabolic problems, including hyperparathyroidism, which further raises the risk of tendon ruptures.
Systemic factors:
Achilles tendon injury may be related to the following systemic diseases:
- Chronic kidney failure
- Insufficient collagen
- Diabetes Mellitus
- Gout Infections
- Lupus
- Parathyroid Disorders
- Rheumatoid Arthritis
- Thyroid Disorders
Achilles tendon injuries can result from foot issues such as the following:
- Cavus Foot
- Inadequate strength and flexibility of the gastrocsoleus inhibited ankle dorsiflexion
- Tibia Vara
- Using functional hyperpronation in Varus alignment
Sign and symptoms of Achillis tendon rupture
Most persons who have an Achilles tendon rupture experience the following symptoms, while it’s possible to have none at all:
- Feeling like you were hit in the calf
- Possible significant pain and swelling in the vicinity of the heel
- An inability to “push off” or bend the foot downward when walking due to an injury
- The wounded leg’s incapacity to stand on its toes
- A sound that pops or snaps when the damage happens
Risk Factors of Achillis tendon rupture
- Age: People between the ages of 30 and 40 are most likely to rupture their Achilles tendon. Tendon deterioration and ongoing engagement in high-risk activities are probably the causes of this.
- Sex: Achilles tendon ruptures are far more common in males than women.
- Recreational games: Playing games like basketball, tennis, or soccer that require quick starts, stops, and leaping
- Past Achilles Tendon Problems: Achilles tendinopathy, also known as tendinitis, can weaken the tendon and increase its susceptibility to rupture.
- Specific Drugs: Antibiotics classified as fluoroquinolones, such as ciprofloxacin and levofloxacin, have a well-established link to an increased risk of tendon rupture.
- Injections of corticosteroids: Corticosteroid injections into or near the Achilles tendon have the potential to weaken it.
- Abrupt Increase in Activity: One of the most prevalent causes of rupture is a rapid, strong contraction of the calf muscle, which frequently occurs during a sporting activity.
- Pre-existing illnesses: Rheumatoid arthritis and other inflammatory diseases are among the medical conditions that might damage tendons.
Diagnosis
History and Physical examination
After playing sports, patients frequently complain of sudden, intense discomfort in the Achilles tendon area. The doctor will ask about the patient’s symptoms, including when they started and how they have changed over time. It’s also critical to inquire about past injuries, social background, and medical history. For instance, because of their lifestyle and risk of re-rupture, patients who are athletes may receive different treatment than those who are not.
Upon physical examination, patients with Achilles tendon ruptures may have considerable weakness in ankle plantar flexion or be unable to stand on their toes. A tendon discontinuity or indications of bruising around the posterior ankle may be palpable.
In the event of a suspected rupture, the examiner should do the Thompson test to determine whether the Achilles tendon is continuous. The patient is put in the prone position with the ipsilateral knee flexed to about 90 degrees and the foot and ankle resting.
The examiner determines if plantarflexion is present and to what extent at the foot and ankle by applying pressure to the calf. The contralateral side should be contrasted with this. A positive (abnormal) test is frequently associated with Achilles rupture.
Diagnostic evaluation
In cases where a positive Thompson test is 96% to 100% sensitive and 93% to 100% specific, the doctor should ascertain if the patient suffered an Achilles rupture after conducting a comprehensive history and physical examination. However, as was already indicated, more than 20% of ruptures of the Achilles tendon are misdiagnosed.
To confirm the diagnosis of Achilles tendon rupture and rule out other injuries, imaging procedures such plain radiographs, MRIs, or ultrasounds may be prescribed. Radiographs are taken in cases of lower leg injuries in order to rule out the possibility of a fracture. Clinical suspicion of Achilles tendon ruptures can be verified by MRI and ultrasonography.
MRI investigations are less sensitive than the clinical diagnostic criteria used to assess Achilles tendon ruptures. MRI examinations can also be costly, time-consuming, and cause delays in surgical treatment. For these reasons, MRIs should only be acquired for preoperative planning in cases of subacute or chronic injuries and confusing presentations.
Treatment of Achillis tendon rupture
The possible advantages and disadvantages of surgical treatment for Achilles tendon ruptures are still up for debate. Studies have demonstrated both surgical and nonoperative methods can produce good functional results and patient satisfaction.
When compared to surgical procedures, conservative therapy has historically demonstrated a greater risk of re-rupture. However, as rehabilitation programs have advanced, the risk difference between these groups has decreased significantly (to 1.6%), but operational therapy leads to increased consequences such as infection and wound dehiscence.
Conservative Treatment
Rest, elevation, pain management, and functional bracing are the first lines of treatment for Achilles tendon rupture. Serial casting and functional bracing had the same healing rates as surgical tendon anastomosis; however, individuals receiving medicinal treatment may have a slightly longer recovery time. All patients require orthotic and physical therapy to help strengthen the muscles and improve the ankle range of motion.
Non-operative treatment is frequently advised for patients with substantial medical comorbidities or comparatively inactive lifestyles. The injury’s chronicity and the integrity of the skin or soft tissues are also taken into account. A non-surgical technique has the advantages of minimal anesthetic risk, no wound problems, and no hospitalization expenses. The danger of re-rupture is the biggest drawback.
Surgical Treatment
The re-approximation of torn ends is a common component of all Achilles tendon repair techniques.
Open repair: These methods entail making incisions that may be inverted L, lazy S, or straight lines. Until only healthy tendon fibers are visible, the Achilles tendon is debrided. A Kessler, Bunnel, Krakow, or Giftbox approach might directly heal the tendon. The Krakow and Giftbox methods (a modified Krakow) are interlocking stitches that offer the strongest finish.
- Mini open repair: To debride the proximal section of the tendon and interlock stitches, often in a Krakow fashion, a tiny incision is made proximally. In addition, two tiny calcaneal incisions are created for bone anchors. The proximal and distal ends are joined by a suture passer into a bone anchor on either side of the calcaneus.
- The PARS system (Arthrex) was the first to use minimally invasive repair. On the back of the leg, a little transverse incision is created. To enable suture passage via small puncture incisions, a gig gadget is utilized.
Even though minimally invasive surgery became more popular when it first came out, when the nerve is not exposed during surgery, there is an 18% chance of sural nerve damage. Furthermore, it is important to note that the majority of research publications on percutaneous Achilles tendon procedures are written by people who work as paid consultants for the sales business that owns the equipment.
Sometimes the repair is reinforced by the flexor hallucis tendon, gastroc-soleus aponeurosis, or plantaris tendon. The muscle exhibits a 52% hypertrophy in cases of chronic flexor hallucis tendon ruptures, indicating a great ability for adaption upon transfer.
In general, the healing rates of surgical repair and casting are comparable. An early return to activity and a lower chance of re-rupture are the primary advantages of a surgical repair; surgical complications such as wound dehiscence, infection, and deep vein thrombosis pose the most risk. There is general agreement that athletes should choose this care because of the improved strength and results after a surgical repair.
Physiotherapy Treatment
Exercise is essential for tendon rupture, regardless of the exact therapy approach used. Exercises that improve muscular strength and range of motion include swimming, cycling, running, and walking.
Depending on the referring physician’s protocol and whether a surgical or nonsurgical method is chosen, rehabilitation will differ. This emphasizes how crucial it is for the therapist and the referring doctor to work closely together in order to maximize care. Given that these factors frequently show the biggest differences in therapeutic management for this disease, this is especially crucial for controlling the usage of braces and assessing weight-bearing status.
Depending on whether an operational or non-operative method is used, the length of immobilization may change. According to the referring orthopedic protocol, immobilization in the operational approach usually lasts between two and four weeks, however in the conservative operative care phase, it can last anywhere from three to nine weeks with the use of orthotics.
During this period, several levels of plantarflexion to neutral placement are used; nonetheless, there is ongoing discussion over the best positioning. It has been shown that preventing hyper dorsiflexion during this period is crucial for preventing Achilles tendon elongation and long-term functional impairments.
When conservative approaches are employed, therapy starts while the patient is immobilized by wearing a cast and focuses on exercises and weight-bearing mobilization training to maintain strength in the remaining parts of the injured limb.
More recent research has demonstrated the advantages of starting functional casts and early weight bearing as part of conservative therapy, which leads to better ankle dorsiflexion and a quicker return to activity. These advantages have historically been linked to surgical treatment, which made it possible to begin weight-bearing and exercise earlier. However, this varies and will be decided by the referring physician.
Glazebrook & Rubinger’s functional rehabilitation approach for nonsurgical individuals after an acute Achilles tendon rupture:
- 0 to 2 weeks: Crutches and non-weight bearing.
- 2 to 4 weeks: Walking boots with maximum heel lifts, controlled weight bearing with crutches in 25% weekly increments, active plantar and dorsiflexion range of motion exercises to neutral, inversion and eversion below neutral, swelling control techniques, physical therapy twice or three times a week, and non-weight bearing aerobic exercises like cycling are all recommended.
- 4–6 weeks: Continue exercises from the preceding weeks while advancing electrical muscle stimulation, bear weight as tolerated in the boot, and get physical therapy two or three times per week.
- 6 to 8 weeks: After 6 to 8 weeks, progressively eliminate the heel lifts (one lift per day as tolerated), put all of your weight in your boot, and do physical therapy twice a week.
- 8 and 12 weeks: Wean off the boot between 8 and 12 weeks.
Rehabilitation activities usually start two to four weeks after surgery. Over the last ten years, there has been a tendency toward faster weight-bearing, less rigorous immobilization, and quicker functional rehabilitation after surgery. Ankle range of motion exercises, resistive and progressive strengthening activities, isometric workouts, cardiovascular exercises, and balancing exercises as needed are all part of post-immobilization treatment.
There is currently no published standardized expedited procedure for recovering from Achilles tendon surgery, and more thorough evidence-based research is required to weigh the risks and benefits.
Low-impact activities are usually the main focus for the first six months, followed by high-impact exercises, with an emphasis on returning to sports when suitable. According to data, there should be a strong emphasis on calf strengthening within the first year following an injury because there is a decrease in strength increase potential after that time.
Differential Diagnosis
The following are examples of differential diagnosis for Achilles tendon rupture:
- Osteoarthritis
- Ankle sprain
- Calf injuries
- Calcaneofibular ligament injury
- Calcaneus fractures
- Deep venous thrombosis (DVT)
- Exertional compartment syndrome
- Fascial tears
- Gastrocnemius or soleus muscle strain or rupture
- Haglund deformity
Prognosis
The majority of people with ruptured Achilles tendon have a very good prognosis. However, some non-athletes could still have some residual deficiencies, such as a decreased range of motion. The majority of athletes are free to return to their prior level of athletic engagement. However, the re-rupture rate for non-surgical therapy is around 40%, while the rate for surgical treatment is barely 0.5%.
Complications
Re-rupture
Prior research has indicated a 10% to 40% re-rupture rate with non-operative care as opposed to 1% to 2% following surgery, while more recent level 1 evidence has found no difference in rerupture rates.
In a randomized controlled experiment with 60 patients from 2009 to 2013 at an 18-month follow-up, Lantto et al. recently proved the following:Similar performance ratings for the Achilles tendon
At the 18-month follow-up, there were somewhat greater calf muscle strength Differences that favored the surgical cohort (10% to 18% strength difference).
The operating cohort had somewhat higher health-related quality of life scores in the areas of bodily discomfort and physical functioning.
Complications with Wound Healing:
Overall, the risk after surgery is between 5% and 10%.
The following are risk factors for wound problems following surgery:
- The most prevalent and important risk factor is smoking.
- Use of steroids in female sex
- Open method (as opposed to percutaneous methods)
Damage to the Sural Nerve:
The percutaneous procedure-related injury rate is higher than that of the open method.
FAQs
Is it possible for an Achilles tendon rupture to mend itself?
One severe injury that needs medical treatment is a torn Achilles tendon. An Achilles tendon rupture may not heal adequately if left untreated. Your chances of rupturing it again may rise as a result.
How may an Achilles rupture be prevented?
Calf muscles should be stretched and strengthened. Your calf should be stretched until it pulls noticeably but not painfully.
Change up your workouts. Switch between low-impact activities like walking, riding, or swimming and high-impact ones like running.
Pick your running surfaces wisely.
Gradually increase the level of workout intensity.
With an Achilles tendon rupture, is it still possible to walk?
Yes, even though it might hurt, you can usually walk with a damaged Achilles tendon. But it’s not a good idea to keep using an Achilles tendon that has been ripped. If you suspect that you may have torn your Achilles tendon, see your physician right away.
Does tendon repair need extensive surgery?
Depending on the tendon and the extent of the injury, tendon repair surgery can be simple or substantial. While some repairs can be completed as outpatient operations, others necessitate a hospital stay and prolonged rehabilitation.
Before an Achilles tendon rupture, are there any warning indicators?
Stiffness: Tightness or stiffness in the Achilles is another indication that a tendon problem can be present. These symptoms are frequently caused by inflammation that impairs normal tendon mobility or micro tears in the Achilles, which, as we discussed above, might be a sign of a tendon tear.
Is a tear less severe than a rupture?
Remarkably, there is no distinction between a rupture and a full tear. On the other hand, a tear may be partial or total.
References:
- Shamrock, A. G., Dreyer, M. A., & Varacallo, M. A. (2023, August 17). Achilles tendon rupture. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK430844/
- Achillis tendon rupture , Physiopedia , https://www.physio-pedia.com/Achilles_Rupture