Amyotrophic Lateral Sclerosis
Amyotrophic Lateral Sclerosis (ALS) is a progressive neurodegenerative disorder that affects nerve cells in the brain and spinal cord, leading to the gradual loss of muscle control. It primarily damages motor neurons, resulting in muscle weakness, atrophy, and eventually, paralysis. While the exact cause of ALS is often unknown, a small percentage of cases are inherited.
Symptoms typically include muscle twitching, stiffness, and difficulty with speaking, swallowing, and breathing. There is currently no cure for ALS, but treatments can help manage symptoms and improve quality of life.
Amyotrophic lateral sclerosis (ALS): what is it?
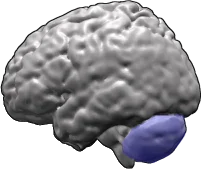
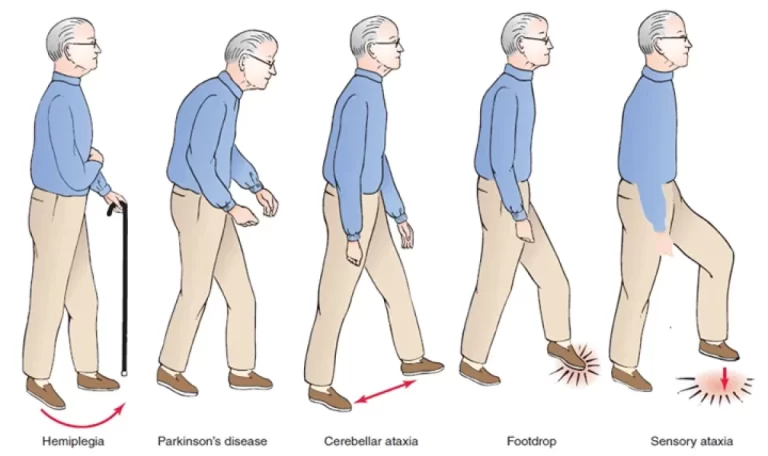
Motor neurons, the brain and spinal cord nerve cells that regulate voluntary muscle movement and breathing, are impacted by amyotrophic lateral sclerosis (ALS), formerly known as Lou Gehrig’s disease. Muscles weaken, begin to twitch (fasciculations), and atrophy due to motor neurons being degenerated and dying and losing the ability to speak with the muscles.
The brain eventually loses the capacity to initiate and regulate voluntary actions, including breathing, talking, chewing, and walking, in individuals with ALS. Since ALS is progressive, its symptoms worsen with time.
It goes after your motor neurons. These control respiration and voluntary muscle movements, such as those used for speaking, chewing, and moving your arms and legs.
Your muscles receive signals from your neurons telling them to move. Similar to bad phone coverage, ALS makes communication difficult. Since the instructions that neurons give to muscles are unclear and fragmented, the call finally terminates. Neurons are unable to receive any more calls as a result of this bad connection.
The symptoms of ALS progressively get worse over time. Muscle weakness and twitching may affect your ability to speak, chew food, reach for objects, and move independently. Your muscles progressively atrophy (waste away) as a result of ALS. Atrophy can cause breathing difficulties and potentially fatal consequences.
ALS has no known cure, but new medicines are being developed all the time. Your quality of life can be enhanced and the disease’s progression slowed with the correct combination of treatments.
Several ALS medications that could increase survival, slow the rate of decline, or aid in symptom management have been licensed by the US Food and Drug Administration. But as of right now, there isn’t a cure for ALS that can halt or reverse its course.
Types
Sporadic ALS
Almost all ALS cases are classified as sporadic, which means that there is no family history of the disease and the disease appears to strike randomly without any obvious risk factors. Family members of ALS patients are more likely to get the condition, but the overall risk is quite low, and the majority do not get ALS.
Familial ALS
Familial (also known as inherited or genetic) ALS accounts for about 10% of all cases. Familial ALS has been linked to mutations in over a dozen genes. A small percentage of persons have this hereditary form of ALS. However, several recent genetic findings indicate that ALS is more common than previously believed in inherited types.
Stages of ALS
Amyotrophic Lateral Sclerosis (ALS) progresses through several phases, each of which symbolizes a particular stage of the disease and its effects on the patient. Knowing these phases aids in predicting the care and support needed at each step and offers insight into how ALS develops. The seven stages of ALS are described below:
Early Symptoms Stage
The first encounter with ALS is often accompanied by subtle symptoms, such as stiffness, twitching, cramping, or weakness of the muscles in the arms, legs, shoulders, or tongue. Initially, these symptoms are typically modest and may go overlooked.
- Muscle weakness
- Difficulty while breathing
- Difficulty while speaking
- Trouble swallowing
- Muscle twitches
The clinical symptom most likely to remain undiagnosed for the longest period among all of these was heavy breathing. Not everyone with early-stage ALS has these obvious symptoms. Other common symptoms include:
- Muscle cramps
- Tightness or “stiff” muscles
- Slurred or pitch changes in speech
Early on, it’s important to consider where ALS starts. The majority of cases (limb-onset ALS) start with limb weakness before progressing to the “trunk,” which is the central region of the body that houses the internal organs. One will start to feel weak when breathing when the trunk is impacted.
Bulbar-onset ALS, however, doesn’t begin in the limbs. For instance, it can cause difficulties with eating and swallowing considerably earlier than limb-onset ALS and begins in the head and neck.
Progressive Weakness Stage
As the disease progresses, muscle weakness and atrophy are made worse by the death of motor neurons, which progressively spreads to other parts of the body. Daily tasks including breathing, swallowing, speaking, and walking get harder and harder.
Advanced Disease Stage
The majority of muscles are now significantly weak, which results in substantial impairment. Patients frequently lose their ability to walk or stand on their own and need help with self-care activities. Breathing and swallowing difficulties become frequent.
Rapid Decline Stage
Although each person’s decline path is unique, most ALS patients eventually require ongoing care. Breathing and swallowing problems worsen, and paralysis may spread to the trunk and limbs.
Final Decline Stage
There is widespread paralysis at this stage. Along with the loss of speech and swallowing abilities, the functional use of arms and legs also declines. Significant breathing impairment results, requiring the use of feeding tubes and ventilators.
End-Stage ALS
Except for ocular movements, patients enter a state of total paralysis. Complete communication loss results and breathing requires constant ventilator support.
Death
Mostly as a result of respiratory failure, the last stage ends in death. Although roughly 10% of people survive for ten years or longer, the typical survival time from onset to death is three to five years.
Causes of ALS
The cause of ALS is unknown to researchers. They think it’s a mix of the following factors:
- Genetics: Up to 70% of familial cases and 5% to 10% of sporadic cases of ALS may be caused by mutations or variations in specific genes. ALS has been associated with more than 40 genes. The genes that control how neurons function—C9orf72, SOD1, TARDBP, and FUS—are the most often impacted.
- Environment: ALS may be caused by physical trauma, infections, or exposure to specific toxic compounds (such as lead or mercury).
Symptoms
- Muscle weakness (arms, legs, and neck).
- Fasciculations are twitches in your tongue, hands, feet, or shoulders.
- Stiff muscles (spasticity).
- Speech challenges (slurring words, trouble forming words).
- Involuntary emotional expressions (like laughing or crying).
- Fatigue.
- Trouble swallowing (dysphagia).
- Drooling of saliva (sialorrhea)
- Speaking or forming words (dysarthria)
- Breathing problem(dyspnea)
- Unintentional emotional outbursts, such as laughing or crying (pseudobulbar symptoms)
- Constipation
- Maintaining weight and getting enough nutrients
- Paralysis
- Muscle atrophy
- Cytoskeletal protein defects
- Autoimmune and inflammatory mechanisms
- Accumulation of protein aggregates (clumps)
- Viral infections
- Depression
- Changing expressions of emotions (emotional lability)
- Muscle cramps
- Muscle contractions are called fasciculations.
- Weight loss
These symptoms worsen after beginning mildly. The rate at which symptoms appear varies from person to person. You could find it more difficult to perform daily tasks like buttoning your shirt or writing your name. You may require more time than normal to eat meals. The symptoms will extend to other areas of your body, regardless of where they start.
People who have ALS will eventually lose the ability to walk or stand, get in and out of bed independently, use their hands and arms, or breathe on their own. They are conscious of their progressive loss of function since they typically still can reason, remember, and comprehend. Both the ALS patient and their loved ones may experience anxiety and depression as a result. Though less frequent, ALS patients may also have trouble speaking or making decisions. Additionally, some people have FTD-ALS, a type of dementia.
Within three to five years of the onset of symptoms, the majority of ALS patients pass away from respiratory failure, or the inability to breathe on their own. But roughly 10% make it for ten years or longer.
Risk factors
ALS risk factors include:
- Genetics. A risk gene was inherited from an immediate family member in roughly 10% of ALS patients. We refer to this as hereditary ALS. Children of the majority of persons with hereditary ALS have a 50% chance of receiving the gene.
- Age. Up until the age of 75, the risk increases with age. Most people with ALS are around the ages of 60 and the middle of their 80s.
- Sex. Under the age of 65, ALS is significantly more common in males than in women. This sex difference diminishes after the age of 70.
- Smoking. Smoking is an environmental risk factor for ALS. Smokers appear to be significantly more vulnerable, especially after menopause.
- Environmental toxin exposure. According to some data, ALS may be related to lead or other drug exposure at work or home. Despite extensive research, no single chemical or substance has been reliably linked to ALS. A higher risk of ALS has been linked to environmental factors including the following.
- Military service. Military veterans are more likely to develop ALS, according to studies. What military duty might cause ALS is unknown. It could involve severe exertion, injuries caused by trauma, viral infections, or exposure to specific metals or chemicals.
Diagnosis
Examination
The physical exam may show:
- Weakness often begins in one area of the body.
- Twitches, spasms, tremors, or a decrease in muscle mass
- Twitching of the tongue (common)
- Abnormal reflexes
- Stiff or clumsy walk
- Decreased or increased reflexes at the joints
- Inability to control laughter or tears (also known as emotional incontinence)
- Loss of gag reflex
How does one identify and treat amyotrophic lateral sclerosis (ALS)?
Getting a precise ALS diagnosis as soon as possible is crucial. Treatments for ALS might work best in the early stages of the disease. Early diagnosis of ALS symptoms can be facilitated by a neurologist with experience in the disease.
ALS cannot be definitively diagnosed by a single test. A medical professional will examine the patient physically and go over their entire medical history. Muscle strength, reflexes, and other reactions will be tested during a neurologic examination. To determine whether symptoms are worsening over time, these tests should be conducted frequently.
A doctor may employ radiology and muscle tests to rule out other problems. An ALS diagnosis may be supported by this.
If you have received an ALS diagnosis, you will require several tests, such as:
- Blood tests.
- Urine tests.
- Your muscles and nerves’ electrical activity can be measured with an electromyogram (EMG).
- A nerve conduction investigation to evaluate the signaling capacity of your nerves.
- Use magnetic resonance imaging (MRI) to check for damage to your spine or brain.
- Other tests can help rule out other disorders that might cause similar symptoms, but they cannot diagnose ALS:
A lumbar puncture. Lumbar puncture, or spinal tap. Your doctor inserts a specialized needle into the region surrounding the spinal cord in the lower back during this test. The pressure in the brain and spinal canal can be measured there. A tiny sample of cerebrospinal fluid (CSF) will be extracted by your healthcare professional, who will then examine it for infections and other issues. The fluid that surrounds the brain and spinal cord is called CSF.
Muscle and nerve biopsy. During this process, a sample of tissue or cells is taken from the body and examined under a microscope by your healthcare professional.
By evaluating the nerve’s capacity to transmit a signal to the muscle or along the nerve, a nerve conduction study (NCS) gauges the electrical activity of muscles and nerves. A needle exam is a recording method that uses a needle electrode to identify electrical activity in muscle fibers.
Depending on the patient’s symptoms, test results, and neurological exam findings, blood and urine tests may be conducted. Cerebrospinal fluid (CSF), the fluid that surrounds the brain and spinal cord, may occasionally be obtained for further testing through a spinal tap (lumbar puncture). To rule out another disease, a doctor could prescribe these tests. To help identify if the patient has a muscle disease other than ALS, a muscle biopsy may be done.
Treatment
Damage to motor neurons cannot be repaired. Nonetheless, getting therapy can improve your quality of life and reduce the onset of your symptoms.
Your care team may recommend one of the following ALS treatments:
- Medications.
- Therapies or rehabilitation.
- Nutritional support.
- Breathing support.
You may need additional or different types of treatment as your condition progresses. To help you live as comfortably and independently as possible for as long as feasible, supportive care is also provided to match your needs.
Currently, there is no cure for ALS or a way to repair damage to motor neurons. Nonetheless, some therapies might prolong survival, enhance quality of life, and decrease the disease’s course. In recent years, new therapies have been developed, and scientists are still looking at a variety of ways to halt or even reverse the progression of ALS.
Physicians, pharmacists, physical, occupational, speech, and respiratory therapists, dietitians, social workers, clinical psychologists, and home care and hospital nurses are some examples of the integrated, multidisciplinary teams of specialists that are most suited to provide supportive health care. To keep patients as mobile, comfortable, and independent as possible, these teams can create a customized treatment plan and supply specialized equipment.
To assist in controlling symptoms including muscle stiffness and cramps, excessive phlegm and saliva, unwelcome bursts of laughter or tears, or other emotional outbursts, a doctor may recommend additional drugs or therapies. Additionally, medications can aid with constipation, depression, pain, and sleep issues.
ALS patients can benefit from the following therapies and interventions:
- Proper body positioning
- Exercise regimens, physical and occupational therapy
- Devices and supports to help people walk.
- Splints and braces for the arms and legs
- Customized wheelchairs
- Home evaluation to facilitate mobility within the house
- Technological devices that help people communicate
- Suggestions for easier-to-swallow foods and liquids
- Support from a nutritionist
- Nasogastric feeding tube
Medical treatment
To supplement an ALS treatment plan, physicians may prescribe the following drugs that have been approved by the US Food and Drug Administration (FDA):
- Riluzole (Rilutek)
- Edaravone (Radicava)
An oral drug called ribulose is thought to lessen motor neuron damage by lowering glutamate levels, which are involved in the transmission of information between nerve cells and motor neurons. Ribulose may extend survival by a few months, according to clinical trials conducted on ALS patients. If the patient has trouble swallowing, the tablet that dissolves on the tongue or the thickened liquid version can be chosen.
It has been demonstrated that degradome, an antioxidant administered intravenously or orally, can halt the functional decline of certain ALS patients. One type of degradome that can be administered orally or through a feeding tube is called RADICAVA ORS.
An oral drug called sodium phenylbutyrate/ursodiol was developed to stop nerve cell death by preventing cells from sending out stress signals. Based on the safety and effectiveness findings of a single, smaller ALS research trial, the FDA authorized Relievo in September 2022. The producer of Relievo took the medication off the market in 2024 when a larger clinical trial failed to validate the earlier results.
People with ALS who have been shown to have a mutation in the SOD1 gene are administered Towermen via spinal injection. It may function by lowering one of the indicators of neuronal damage, though the advantages of this medication are still being investigated.
Treatments to control other symptoms include:
- Diazepam or Baclofen for spasticity that gets in the way of everyday tasks.
- Trihexyphenidyl or amitriptyline for people with problems swallowing their saliva.
Rehabilitation
Rehabilitation, which should be customized to the patient’s needs and may involve physical, occupational, and speech therapy, is typically a part of an ALS treatment strategy.
For ALS, your doctor may suggest various forms of therapy or rehabilitation, such as:
Maintaining your independence and safety is the aim of physical therapy for ALS. Mild cardiovascular exercises like swimming or walking can improve general health and help you gain muscle.
Occupational therapy: This field gives you methods and approaches to get through your day. If you need assistive technology, such as a wheelchair, walker, or braces, this is advantageous. You can learn how to utilize these gadgets and move while feeling worn out with the assistance of occupational therapists.
Speech and communication support
People with ALS can learn how to communicate more effectively and loudly with the assistance of speech therapists. Eye-tracking sensors are used by computer-based voice synthesizers to enable users to text on customized screens and browse the web. People with ALS occasionally utilize voice banking to save their voices for use in computer-based speech synthesizers in the future.
A brain-computer interface (BCI) is a device that uses just brain activity to enable people to interact with one another or operate devices like wheelchairs. More effective mobile BCIs for those with severe paralysis and/or vision impairments are being developed by researchers.
Communication training helps you keep talking for as long as possible, and speech therapy offers techniques for safer swallowing. Speech therapists can also teach you nonverbal communication strategies. Nonverbal expression saves energy when verbal communication is not possible.
Home care advise
At various stages of the disease, physical therapy can assist the person with ALS in maintaining function, including reducing their risk of falls and joint pain and increasing their level of independence.
Range-of-motion exercises combined with low-impact activities like swimming, walking, or riding a stationary exercise bike can help preserve muscular function and strength. Occupational therapists can assist with self-care and everyday life activities. To help the client become as independent as possible, they can also recommend assistive gadgets for grooming, bathing, and feeding.
ALS patients often experience weight loss. The disease itself makes more food and calories necessary. However, swallowing and choking problems make it difficult to consume enough. A tube may be inserted into the stomach to aid with feeding. Healthy food tips can be obtained from a nutritionist with expertise in ALS.
Receiving a diagnosis of ALS can be frightening and upsetting. ALS is always deadly, and although treatment can help control symptoms and potentially slow the loss of function, there is no known cure.
Offering to assist a loved one in making decisions related to a terminal disease is one of the best ways to support them during this time.
This entails talking about your loved one’s preferences for hospital care, treatment alternatives, and financial decisions. They might eventually be unable to speak up for themselves. As ALS worsens, being aware of their desires might help guarantee that they are respected.
Additionally, you can offer assistance by:
- Keeping their appointments
- facilitating correspondence between insurance companies, caregivers, and medical specialists to arrange doula or palliative care services
- keeping an eye out for indications of pain, suffering, or mental health issues in your loved one
- Assisting them with errands or housework and spending time with them in a friendly manner—talking, listening, reading, etc.
- When someone you care about suffers from a terminal disease, it’s tough for you too. Remember to look after yourself.
Taking care of yourself is not selfish; rather, it’s a strategy to keep you resilient throughout this trying time.
Support for nutrition, breathing, and feeding
Chewing, swallowing, and obtaining the nutrition they require can be difficult for those with ALS. Registered dieticians and nutritionists can help you identify items to avoid and arrange short, nutrient-dense meals throughout the day. A feeding tube can lower a person’s risk of pneumonia and choking when they are unable to eat with assistance.
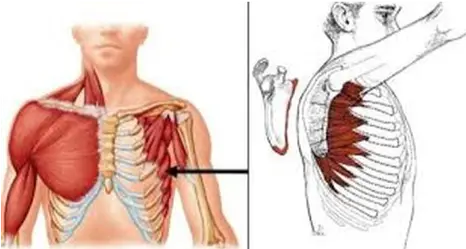
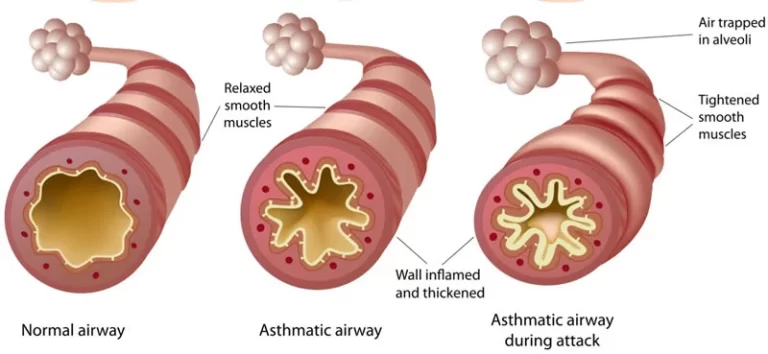
People with ALS may experience dyspnea when exercising and have trouble breathing at night or while they are lying down as their respiratory muscles begin to deteriorate. A mask is typically worn over the mouth and/or nose to provide noninvasive ventilation (NIV), a form of breathing support. For many ALS patients, it might lessen breathing difficulty. NIV might only be required at night at first, but it might later be used all the time. As the disease worsens, the patient might require mechanical ventilators, or respirators, to help them inflate and deflate their lungs.
People with ALS may also have difficulty coughing vigorously because the muscles that regulate breathing weaken. There are several methods, such as using mechanical cough assistance devices, to augment the force of coughing.
Nutritional support
With ALS, it might be challenging to consume enough food and liquids to meet your body’s demands. You can lose weight quickly and not obtain enough vitamins and minerals to sustain and strengthen your body if you have problems swallowing or eating certain meals.
Dietitians can design a meal plan that gives you the proper number of calories, fiber, and fluids while avoiding items that are difficult to swallow. Eating balanced, healthful meals is guaranteed when you receive nutritional coaching. In cases where swallowing becomes challenging, a dietitian can also suggest alternative foods.
You might eventually require a feeding tube to receive the nutrition you require. Additionally, a feeding tube lowers the risk of pneumonia and choking. These problems result from inadvertently breathing food or drink into your lungs.
Breathing support
As your ALS worsens, you can have trouble breathing. Noninvasive ventilation (NIV) is a sort of breathing support that may be helpful for you. NIV is administered by wearing a mask over your mouth and nose. It may improve the ease of breathing. Later on, you might require NIV full-time, but initially, you might only need it at night.
Non-invasive machines (like CPAP or BiPAP) are referred to as breathing devices. Others require a tube in the trachea (invasive ventilation).
You might eventually require mechanical ventilation, which entails wearing a respirator. This device facilitates breathing. It causes your lungs to expand and contract.
If you have trouble breathing, especially when you’re lying down or exercising, let your care team know. They will talk about ways to ease breathing.
Support Groups
Since mental functioning is unaffected, emotional support is essential for managing the disease. People who are dealing with the disorder may be able to get support from organizations like the ALS Association.
There is also available and potentially highly beneficial support for those who are caring for someone who has ALS.
A person with ALS will require increasing assistance with everyday tasks as their disease worsens. Although it is gratifying, caring for someone with ALS can be difficult for both the caregiver and the person’s loved ones. Caregivers should look for themselves and get help when they need it. Resources for home health care services and support are available both for free and for a fee. To locate local help, check out the organizations mentioned in this article.
Prevention
Is it possible to avoid ALS?
- There isn’t a known way to stop ALS. To further comprehend the reasons and risk factors, research is being done to help create future prevention solutions.
Complications
As ALS symptoms worsen, your life expectancy will decrease. Your mental health may suffer as a result of learning about this diagnosis and coping with it daily. You might experience tension, overwhelm, confusion, or despair. As a result, despair and anxiety are common among patients with ALS.
Complications of ALS include:
- Breathing in food or fluid (aspiration)
- Loss of ability to care for self
- Lung failure
- Pneumonia
- Pressure sores
- Weight loss
ALS is difficult to handle alone. Make sure to look after your mental health in addition to your physical health, which will be treated by a variety of experts. Seek assistance from a mental health professional or your care team.
ALS has no known cure. Most people’s disease will worsen over three to five years, preventing them from moving their arms or legs voluntarily. In some individuals, the disease may progress slowly over many years or quickly worsen over a few months. Every individual is impacted uniquely. You will eventually require assistance with eating, moving around, and personal hygiene. Additionally, the diaphragm’s ability to move for breathing is compromised. For breathing, you could require a device called a ventilator. Respiratory failure kills the majority of ALS patients. Due to their decreased movement, people with ALS are susceptible to additional consequences. Among these are pressure injuries. Additionally, they run the danger of losing weight due to a decrease in muscle mass.
Breathing problems
Breathing muscles become weak as a result of ALS over time. To assist them breathe at night, people with ALS may require a mask ventilator, or similar equipment. The gadget resembles something a person with sleep apnea may wear. By wearing a mask over the mouth, nose, or both, this kind of gadget helps the user breathe.
A tracheostomy is a choice for some patients with severe ALS. This is a surgically made opening that leads to the windpipe at the front of the neck. On a tracheostomy, a ventilator might function more effectively than a mask.
The primary cause of death for people with ALS is breathing difficulty. Within 14 to 18 months of receiving a diagnosis, half of ALS patients pass away. Nonetheless, some ALS patients survive for ten years or more.
Speaking problems
The majority of ALS patients experience weakening in their speech-forming muscles. Usually, this begins with slurred words and slower speaking. Speaking therefore becomes more difficult. This may worsen to the point that the person’s speech becomes incomprehensible to others. Communication is done through technology and other means.
Eating problems
ALS patients may experience impairment in the swallowing muscles. Malnutrition and dehydration may result from this. Additionally, they are more likely to inhale food particles, beverages, or saliva, which can result in pneumonia. In addition to ensuring adequate nourishment and hydration, a feeding tube can lower these risks.
Dementia
Decision-making and language are issues for some ALS patients. Frontotemporal dementia is a type of dementia that some people are eventually diagnosed with.
Prognosis
What is the ALS prognosis?
- Because ALS impairs the way your motor neurons operate, your prognosis is not good. The rate of damage to motor neurons determines your prognosis. Damage to motor neurons cannot be reversed by any existing treatment. However, your doctor will present choices to assist slow the progression of symptoms.
Does ALS have a hereditary component?
Indeed, there are hereditary forms of ALS. Your biological parents may pass on the genetic alterations that cause ALS to you. However, inherited ALS is uncommon. Genetic alterations can occasionally occur at random and have no family history.
Life expectancy for ALS
Three to five years is the typical life expectancy following an ALS diagnosis. 10% to 20% of people survive for at least ten years, while 30% of people live for five years or longer. To find out more about your circumstances, speak with your healthcare professional as your life expectancy may differ from these figures.
Although some individuals may live for years or even decades following diagnosis, the average life expectancy is two to five years. After being diagnosed with ALS, almost half of the patients survive for three years or more. Up to 10% of people live longer than ten years, and about 25% live five years or more. Some patients have extended lifespans. For instance, Stephen Hawking, a well-known physicist, survived his diagnosis for over 50 years.
Living with ALS
ALS will eventually cause death and disability. Your mind and capacity for thought are typically unaffected, but your ability to move and breathe on your own will be. Your healthcare practitioner will collaborate closely with you and your family to manage symptoms as they appear. Taking medication can extend your life by several months, especially if you have swallowing difficulties. Talk about the usage of wheelchairs and other mobility aids, as well as strategies to make living areas more accessible. Discussing end-of-life choices with your loved ones is crucial.
Clinical trials might be of interest to you if you have ALS. These tests and investigations are conducted on specific diseases to assist researchers in developing new treatment choices or preventative strategies. By doing this, the condition can be better understood. Researchers can learn more about the origins and risk factors of ALS as well as the disease itself, which could lead to a future cure.
Who is more susceptible to amyotrophic lateral sclerosis (ALS)?
A risk factor is a condition or behavior that is more common in people with a disease or who are more likely to develop one than in people without the risk factor. The presence or absence of a risk factor does not ensure that you will develop a disorder. ALS risk factors include:
- Age: Although the disorder can strike anyone at any age, symptoms usually start to show up around the ages of 55 and 75.
- Biological sex: ALS is significantly more common in men than in women. Men and women, however, have an equal chance of receiving an ALS diagnosis as they age.
- ALS affects persons of all races and ethnicities, however, White people and non-Hispanics are more likely to have the disease.
Although the exact cause is unknown, some research indicates that military veterans have a 1.5–2 times higher risk of developing ALS. Veterans may be at risk for exposure to environmental pollutants, pesticides, and lead. Further research is required to fully understand the relationship between head injuries and increased risk for ALS, as some studies have suggested.
In the United States, 93% of ALS patients are Caucasian, and men make up about 60% of those with the disease. According to US demographic surveys, there are about 15 new instances of ALS identified every day in the US, or a little over 5,600 persons annually. Up to 30,000 Americans are thought to have the disease at any given moment. With an average diagnostic age of 55, ALS often strikes patients between the ages of 40 and 70. People in their 20s and 30s do, however, occasionally have the condition.
Conclusion
The seven stages of Amyotrophic Lateral Sclerosis (ALS) illustrate the significant effects that the disease has on those who are affected and their loved ones. The progressive nature of ALS needs a thorough understanding, early diagnosis, and a multidisciplinary approach to treatment and therapy, as symptoms can range from mild to total paralysis.
Understanding each stage can help us better understand how the requirements of people with ALS change over time, opening the door to more patient-centered care, support, and ultimately more sophisticated therapeutic interventions.
The degenerative disease known as ALS is caused by the death of motor neurons in the spinal cord. Early ALS symptoms often affect a single body part and result in minor disability. More areas are impacted as ALS worsens, and voluntary muscular control may completely disappear.
Although life expectancy varies, ALS is a fatal disease. After being diagnosed, some people continue to survive for over ten years. Symptom management and disease progression can be slowed with treatment.
Researchers are trying to find ways to prevent ALS in persons who have risk factors for the disease. Early claims of some products or potentially beneficial lifestyle modifications require more research. Schedule a consultation with your physician if you have any ALS risk factors.
Your quality of life can be enhanced and the disease’s progression slowed with early detection and treatment.
FAQs
How fast does ALS develop?
With ALS, there is no time limit on how soon symptoms appear. In the absence of treatment, they might advance more quickly. Additionally, the speed may differ depending on your age, weight at diagnosis, and symptoms. To limit the growth of the disease, your doctor might advise you to take specific medications.
What is amyotrophic lateral sclerosis’ primary cause?
People who have familial ALS only need to acquire the disease from one parent to experience symptoms because it is caused by an inherited mutation in a dominant gene. Novel mutations in the genes. Individuals who have sporadic ALS may exhibit spontaneous genetic mutations that are not inherited and are the source of their ALS.
How long does it take for someone with ALS to live?
Additionally, 20% of ALS patients live for five years, 10% for ten, and 5% for twenty years or more, even though the average survival period is three years. Additionally, an individual’s progress isn’t necessarily linear. Weeks to months of periods with little to no function loss are not uncommon.
Which three ALS symptoms are present?
Muscle twitches and cramps, particularly in the hands and feet.
Impairment of hand and arm motor control.
Difficulty moving the arms and legs.
Falling after tripping.
Letting things fall.
persistently high levels of weariness
Uncontrolled bursts of tears or laughter.
Does having ALS cause pain?
Does pain occur with ALS? Yes, even though it usually does so in an indirect manner. According to our current understanding, the disease process in ALS solely impacts the motor neurons—the nerve cells that govern strength—in the brain, spinal cord, and peripheral nerves.
Which ALS patient has lived the longest?
How uncommon is Hawking’s lifespan? Very uncommon. Although the longest-living ALS patient in North America, a Canadian named Steven Wells, has had the disease for nearly 40 years, just 5% of ALS patients live for more than 20 years, and it is almost unheard of to live for 50 years or more, according to the ALS Association.
What are ALS’s latter stages?
Mobility is very restricted; a caregiver is required to meet demands. Fatigue, hazy thinking, headaches, and an increased risk of pneumonia can all be symptoms of poor breathing. It can become impossible to speak. Oral consumption of food and liquids is not feasible.
How may ALS be reversed naturally?
Are there natural cures for ALS? As of this now, ALS has no known cure. According to some research, several herbal remedies, may help alleviate some ALS symptoms and reduce the disease’s progression.
Why is ALS so prevalent today?
Using data from the National ALS Registry and Biorepository, for instance, researchers discovered in 2024 that exposure to five particular chemicals present in steel, rubber, dyes, batteries, and solvents raised the risk of developing ALS by three to six times.
Reference
- Amyotrophic lateral sclerosis (ALS). (n.d.). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/amyotrophic-lateral-sclerosis-als
- Amyotrophic lateral sclerosis (ALS). (2025, February 7). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16729-amyotrophic-lateral-sclerosis-als
- Amyotrophic lateral sclerosis (ALS): MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/000688.html
- Amyotrophic lateral sclerosis (ALS) – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/amyotrophic-lateral-sclerosis/symptoms-causes/syc-20354022
- Cona, L. A., MD. (2024, June 5). 7 Stages of ALS: Disease progression (2024). https://www.dvcstem.com/post/7-stages-of-als
- Gillette, H. (2023, April 12). What are the stages of ALS? Healthline. https://www.healthline.com/health/stages-of-als#summary




One Comment