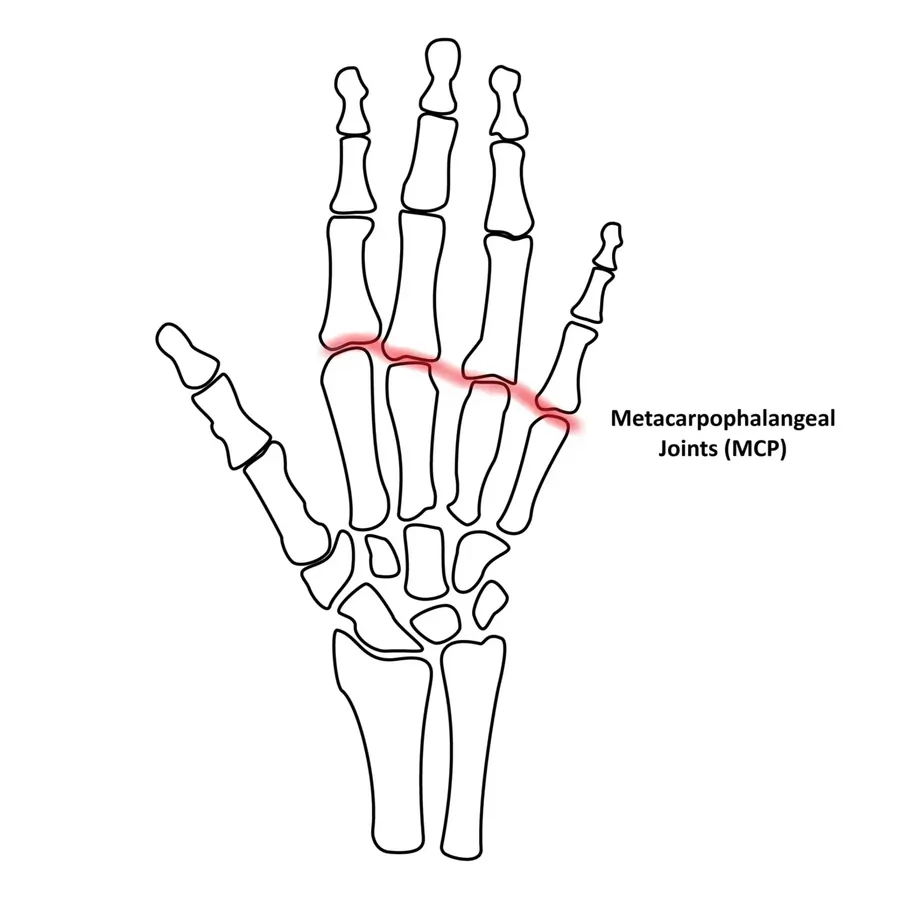
Metacarpophalangeal (MCP) Joints
The metacarpophalangeal (MCP) joints are the knuckle joints where the metacarpal bones of the hand meet the proximal phalanges of the fingers. These synovial joints allow flexion, extension, abduction, adduction, and limited rotation, enabling fine motor movements. They are supported by collateral ligaments, the volar plate, and the extensor hood, contributing to joint stability and hand function.
Each metacarpal bone is connected to the matching proximal phalanx of each finger by five distinct metacarpophalangeal joints. Concave bases of the proximal phalanges accept convex heads of the metacarpal bones to form each metacarpophalangeal joint.
The metacarpophalangeal joints can move in the following directions: flexion, extension, circumduction, abduction, adduction, and limited rotation. The ligaments, joint capsule, and surrounding musculotendinous structures all contribute to the stability and flexibility of the fingers, which are essential for hand function.
Introduction
Metacarpophalangeal (MCP) joints are diarthrodial joints in which the concave proximal aspect of each phalange articulates with the massive convex heads of the distal aspect of the metacarpals. Each metacarpal head and proximal phalange has a hyaline cartilage articulating surface. As transitions between the palm and the fingers, each hand has five distinct MCP joints. In layman’s terms, the MCP joints are known as the “knuckles,” the metacarpal heads are most apparent dorsally while making a fist.
Stability and flexibility are combined in these joints to provide the hand’s necessary dexterity. Muscles act on the MCP joints, just like on other joints in the body, to enable particular joint movements. These motions consist of limited circumduction, flexion, extension, abduction, and adduction. A classic and distinguishing characteristic of rheumatoid arthritis (RA) from osteoarthritis (OA), which usually affects the distal interphalangeal (DIP) joints, is arthritis affecting the MCP joints.
Structure and Function
The human hand’s ability to function depends critically on the MCP joints. Although the thumb’s MCP joint and the MCP joints of the other digits are physically and functionally identical, there are some variances, which will be mentioned as appropriate. The thumb’s MCP joint is a hinge joint that permits little extension, adduction, or abduction and up to 80 to 90 degrees of flexion. The two to five-digit MCP joints are shallow ball and socket joints that permit minimal circumduction, flexion, extension, abduction, and adduction.
Along with differences in muscle attachment sites, the thumb’s MCP joint’s range of motion differs significantly from that of the fingers’ MCP joints. The form of the metacarpal heads explains this discrepancy. Range of motion (ROM) is decreased in the thumb because the metacarpal head is flatter than the metacarpal heads of the second through fifth MCP joints. Despite this, there is a great deal of variation in thumb range of motion because different people have more spherical metacarpal heads.
The MCP joint’s design offers very little inherent stability. The joint capsule, ligaments, and the surrounding musculotendinous balance are the main stabilizing factors of the joint.
The dense fibrocartilaginous thickening of the palmar aspect of the MCP joint capsule is called the volar plate. The main purpose of the volar plate is to keep the joint from becoming too stretched. After starting on the metacarpal head, it attaches to the nearby proximal phalange. Two sesamoid bones are embedded in the thumb, and the proximal part of the palmar plate is narrower than the distal third.
Together with the palmar plate and A1 annular ligament, the sesamoids—which are joined by the phalangoglenoid ligament—form a synovial sheath that stabilizes the flexor pollicis longus tendon as it crosses the MCP joint. The deep transverse metacarpal ligament, which supplies stability and keeps the metacarpal heads from separating, connects the palmar plates of digits two through five.
There is a collateral ligament on the radial and ulnar aspects of every MCP joint, which is made up of an auxiliary collateral ligament and a proper collateral ligament. The main stabilizers of the MCP joint are the appropriate collateral ligaments, which are robust cord-like structures. The appropriate collateral ligaments arise from the lateral-dorsal face of the metacarpal head and traverse the joint to insert onto the volar border of the next proximal phalange.
The accessory collateral ligaments fan out obliquely to insert onto the distal part of the volar plate, having a more volar and proximal origin than the true collateral ligament. The proper collateral ligaments are taut in joint flexion, while accessory collateral ligaments are taut in joint extension because of the two collateral ligaments’ different orientations and the metacarpal head’s distinctive oval form. Furthermore, these variations produce a cam effect that allows for a significant range of motion (ROM) in both the flexion extension and adduction-abduction axes.
Along with the palmar plate and collateral ligaments, the joint capsule envelops the MCP joint. It keeps the joint taut during joint flexion and stabilizes it dorsally.
The plantar plate gives rise to sagittal bands, which superficially encircle the MCP joint and form a “lasso” around the extensor muscle-tendon underneath. The extensor muscle may extend the MCP joint thanks to this structure, even though it has a weak attachment to the proximal phalanx.
Embryology
The zone of polarizing activity (ZPA), the apical ectodermal ridge (AER), and the nonridged ectoderm are the three main signaling centers that work in concert to guide the creation of the proper developmental axis for the upper extremities.
The conclusion of the fourth week of embryonic development marks the emergence of four limb buds from the ventrolateral surface of the growing embryo. The lateral plate mesoderm gives rise to the somites and mesenchyme that make up the limb buds, which are then encased in a layer of cuboidal ectoderm.
Later, the cells from the lateral plate mesoderm will develop into the connective tissue of the extremities. When the somites’ paraxial mesoderm cells move into the limb buds, they produce the limb musculature. The AER is finally formed by the ectoderm layer at the distal tip of the developing limb growing larger. As more proximal limb cells farther from the AER start to develop into connective tissue and muscle cells, the AER causes nearby mesenchymal cells to stay undifferentiated and keep growing.
As the sixth week of embryonic development concludes, chondrocytes have produced a basic hyaline cartilage construct that will later undergo endochondral ossification to build the upper extremity’s bones. This cartilage forms the MCP joints when chondrogenesis is locally stopped by factor signaling, which eventually leads to the creation of a joint cavity. The joint capsule develops from mesenchymal cells that are close to the joint cavity. The epiphyses ossify postnatally, whereas the diaphyses of the metacarpal and proximal phalanges are ossified by the ninth week.
Articular surfaces
The joints that link the palm and fingers are called metacarpophalangeal joints. The rounded biconvex head of the metacarpal bones is home to the proximal articular facet. Anteriorly, this articular surface is larger than posteriorly.
The significantly smaller concave articular facets on the bases of the proximal phalanges engage with the metacarpal heads. The palmar ligament, which serves as a hinge, elongates the facets of the phalanges anteriorly. Hyaline cartilage lines the articular surfaces of the phalangeal and metacarpal processes.
Two of the hand’s bones articulate to form the metacarpophalangeal joint:
- The metacarpal head is a convex, massive articulating surface.
- The proximal phalanx’s base has a concave, smaller articulating surface.
Hyaline cartilage lines the articular surfaces of the metacarpal and phalangeal bones.
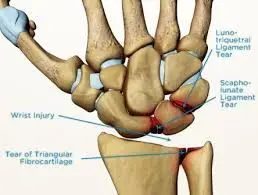
Ligaments and joint capsule
A loose fibrous capsule that is attached around the articular facets’ edges envelops the joint. Through collateral metacarpophalangeal ligaments, the joint capsule is reinforced and thickened on its medial and lateral sides. The posterior capsule gets fibers from the tendons of the long extensors of the forearm (extensor pollicis longus, extensor indicis, extensor digitorum, and extensor digiti minimi), while the palmar metacarpophalangeal ligament primarily replaces the capsule on its anterior aspect.
Collateral ligaments
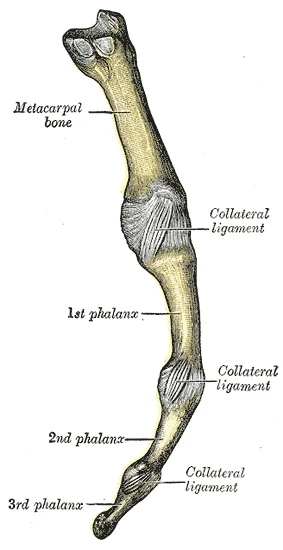
The collateral ligaments, which are found on the radial and ulnar sides of the MCP joint, are important stabilizers of the joint. Proper collateral and auxiliary collateral ligaments make up these ligaments. Together, these robust ligamentous bands restrict the range of motion in the adduction-abduction and flexion-extension axis.
The palmar aspect of the nearby proximal phalanx, just distal to the base, is where the appropriate collateral ligaments extend from the posterior tubercles on the dorsolateral aspect of the metacarpal head. These ligaments’ main function is to restrict the MCP joint’s range of motion.
The accessory collateral ligaments connect to the distal third of the palmar (also called volar) plate more distally after attaching more proximally to the metacarpal head. The joint’s range of motion is restricted by the accessory collateral ligaments’ taut extension.
Palmar ligament
A dense fibrocartilaginous thickening on the palmar face of the MCP joint capsule is called the palmar ligament, sometimes known as the palmar or volar plate. Their attachment to the palmar side of the metacarpal neck is slack, but they are securely attached to the palmar surface of the neighboring proximal phalanx’s base. The collateral ligament and the palmar ligament’s sides merge. The thumb’s palmar ligament comprises two sesamoid bones that articulate with the thumb’s metacarpal head’s palmar facets. The primary purpose of this ligament is to keep the MCP joint from being overextended.
Deep transverse metacarpal ligaments
The thin fibrous bands that connect the second through fifth metacarpophalangeal joints by running across their palmar surfaces are known as the deep transverse metacarpal ligaments. They are located posterior to the lumbricals and anterior to the interossei muscles. The central palmar aponeurosis’s digital slips are attached to their palmar surfaces. The stability of the MCP joints during grip functions is mostly facilitated by these ligaments.
Joint Capsule
The loose fibrous joint capsule that covers each metacarpophalangeal joint affixes along the articulating surface edges. Collateral ligaments strengthen the thicker joint capsule on the medial and lateral sides.
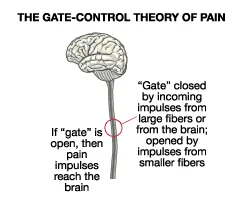
Innervation
The nerves listed below innervate the metacarpophalangeal joints:
- The radial nerve’s branch known as the posterior interosseous nerve (C5-T1)
- The C8-T1 deep terminal branch of the ulnar nerve
- The median nerve’s palmar branches (C6-T1)
Blood Supply and Lymphatics
The ulnar and radial arteries, which anastomose in the superficial palmar and deep palmar arches, provide blood to the hand. The dorsal and palmar metacarpal arteries, the radial artery of the index finger, the common palmar digital arteries, and the Princeps pollicis artery are only a few of the many branches that supply the MCP joints.
Both superficial channels that run beside the basilic and cephalic veins and deep channels that run alongside the arteries are responsible for the hand’s lymphatic drainage. The cubital and epitrochlear lymph nodes are among the lymph nodes in the elbow where these lymphatics flow before finally emptying into the axillary or infraclavicular lymph nodes.
There are branches of the radial and ulnar arteries that give blood to the MCP joints.
- Princeps pollicis artery
- Palmar and dorsal metacarpal arteries
- Radialis indices artery
- Common palmar digital arteries
Nerves
The three primary forearm nerves—medial, ulnar, and radial—provide innervation to the muscles that traverse the MCP joint by branches. The palmar branches of the median nerve, the deep terminal branch of the ulnar nerve, and the posterior interosseous nerve innervate the MCP joints.
Mobility and Stability
The metacarpophalangeal joint is stabilized mostly by the collateral ligaments. Whereas the supplementary collateral ligaments restrict hyperextension, the proper collateral ligaments mainly restrict hyperflexion.
The palmar ligament’s primary purpose is to stop overextension. When performing grip functions, the deep transverse metacarpal ligaments help to stabilize the MCPJ.
Movements
There are two planes of motion in each metacarpophalangeal joint. Flexion, extension, abduction, adduction, circumduction, and restricted rotation of the digit are all permitted.
The hand and forearm muscles are responsible for moving the joint.
Thumb
- The flexor pollicis brevis and longus muscles cause flexion.
- Extensor pollicis brevis and longus create extension.
- Adductor pollicis produces adduction.
- Abductor pollicis longus and brevis create abduction.
- The flexor and abductor pollicis brevis muscles contract together to cause axial rotation.
Digits 2-5
- Flexor digitorum superficialis, flexor digitorum profundus, lumbricals, and flexor digiti minimi (5th digit) all contribute to flexion.
- Extensor digitorum, extensor indicis (second digit), and extensor digiti minimi (fifth digit) all contribute to extension.
- The palmar interossei muscles create adduction.
- The muscles that produce abduction are the dorsal interossei. It is also the abductor digit minimi that causes the abduction of the fifth digit.
Metacarpophalangeal joints can move in flexion, extension, adduction, abduction, circumduction, and limited rotation. Every joint has two degrees of freedom.
Flexion and extension
The two main movements in the metacarpophalangeal joint are thought to be flexion and extension. While extension spans from 10° in the index finger to 30° in the little finger, active flexion has a range of motion of about 90°. A minor lateral rotation is associated with flexion in the third to fifth MCP joints, whereas a slight medial rotation is associated with flexion in the second MCP joint.
About 60°, or nearly total flexion, is the thumb MCP joint’s full range of motion. Antagonistic muscles and ligamentous tissues around the joint restrict mobility in this axis.
Abduction and adduction
About 25 to 30 degrees is the complete range of motion in this axis. Abduction is primarily responsible for this rather limited range of motion. Collateral ligaments and the metacarpal head’s width and shape mostly restrict these motions. The above-described configuration of the collateral ligaments prevents either abduction or adduction from occurring while the MCP joints are flexed. The movements in the corresponding carpometacarpal joints always follow abduction and adduction in the MCP joints.
The thumb’s MCP joint is most affected by axial rotation, which happens during opposition. There are two types of rotation: active and passive. The flexor pollicis brevis and abductor pollicis brevis muscles work together to produce the active axial rotation. While passive movement might go either way, active rotation is always directed medially.
Full flexion is the close-packed position of the second to fifth metacarpophalangeal joints, whereas maximal opposition is the close-packed position of the first metacarpophalangeal joint. Slight flexion is the open packed (resting) position for every joint. The capsular arrangement of the joints restricts flexion more than extension.
These joints also have some auxiliary movements. Anteroposterior and lateral translation of metacarpals or phalanges, as well as accessory rotation at the thumb joint, are the main aspects of this.
Muscles acting on the metacarpophalangeal joint
All of the MCP joints’ movements are controlled by the hand and forearm muscles.
- The flexor pollicis brevis, with assistance from the flexor pollicis longus muscle, is the primary muscle responsible for thumb flexion. Flexor digitorum superficialis, flexor digitorum profundus, lumbricals, and flexor digiti minimi brevis (fifth digit) are responsible for flexing digits two through five.
- The extensor pollicis brevis is the primary muscle responsible for thumb extension (from the flexed position), with some assistance from the extensor pollicis longus muscle. Extensor digitorum, extensor indicis (second digit), and extensor digiti minimi (fifth digit) all contribute to the extension of digits 2 through 5.
- Adduction of the thumb is performed by the adductor pollicis, whereas the palmar interossei muscles cause adduction of the other four digits.
- Abductor pollicis longus and abductor pollicis brevis create abduction of the thumb; abductor digiti minimi produce abduction of the fifth digit; and dorsal interossei muscles produce abduction of fingers 2–5.
- Flexor pollicis brevis and abductor pollicis brevis co-contraction actively produce axial rotation.
Clinical Significance
Metacarpophalangeal joint pain
Metacarpophalangeal (MCP) joint pain refers to discomfort or inflammation in the knuckle joints, which can result from various causes, including arthritis (such as rheumatoid or osteoarthritis), injury, overuse, or ligament strain.
Hand function may be impacted by symptoms such as discomfort, stiffness, edema, and decreased range of motion. In order to control symptoms and stop more joint deterioration, a proper diagnosis and course of treatment are crucial.
One characteristic of rheumatoid arthritis is that it affects the MCP, whereas osteoarthritis affects the distal interphalangeal joint.
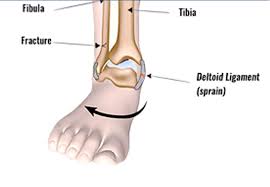
Skier’s Thumb
An injury to the ulnar (medial) collateral ligament of the first metacarpophalangeal joint is referred to as a “skier’s thumb.” Usually, it happens when the thumb is violently abducted.
Skiers who fall on an outstretched arm while carrying a ski pole are most likely to experience it because the thumb is forced to stay in an abducted position.
To heal severe injuries like displaced bone avulsion fractures or total ligamentous rupture, surgery is necessary.
Rheumatoid Arthritis With MCP Joint Involvement
The inflammatory disease known as rheumatoid arthritis (RA) is characterized by significant inflammation of the synovium, hyperplasia, and the loss of cartilage and osseous tissue.MCP and proximal IP joints are the most often attacked minor joints by autoantibodies. Anti-cyclic citrullinated protein (anti-CCP) and rheumatoid factor (RF) antibodies are disease markers that are usually associated with high C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Swelling and joint discomfort are the most typical signs of RA. Along with additional physical issues, some patients may experience psychological issues and cardiovascular problems.
RA differs from other joint illnesses in that it involves the MCP joint. An imbalance between the active and passive forces acting on the joint is caused by connective tissue inflammation, which results in deformity, discomfort, and instability. Usually, bilaterally symmetric MCP joint edema is discovered early. A physical examination reveals pain while applying pressure or moving passively. MCP joint dislocation is frequent; in the later stages of the disease, it typically manifests as flexion and ulnar deviation. Consideration must be given to surgical intervention when the deformity significantly impairs function.
A systemic inflammatory disease that lasts a lifetime is RA. For RA patients who are surgical candidates, a thorough assessment of their dietary and general condition is necessary. The best surgical treatment is determined in part by the extent of bone loss and deformity.
MCP Joint Dislocation
MCP joint injuries are frequently the result of direct trauma.
Swelling, bruising, deformity, palpable discomfort, and restricted range of motion are common symptoms of MCP joint dislocation. The distal osseous fragment and its location with the proximal osseous element are usually affected by the disease. Dorsal dislocation is the most typical pattern of presentation.
MCP joint dislocations can be further divided into two categories: basic and complicated. Closed reduction is an effective method for treating simple dislocations, whereas open reduction is typically necessary for complex ones.
The following characteristics characterize a classic complicated dorsal MCP dislocation:
- High proximal phalanx extension
- Avulsion from the proximal metacarpal head and rupture of the volar plate
- Dorsal to the metacarpal head, the volar plate prevents closed reduction.
- Ulnar displacement of the flexor tendons
- Both radial and volar displacement of the metacarpal head
“Button-holes” in the metacarpal head between four structures:
- Lumbrical
- Flexor tendon on the displaced digit’s ulnar side
- The distal transverse bands of the natatory ligaments
- Superficial transverse ligament (proximal)
Entrapment of the volar plate, sesamoid bones, bone fragments, and flexor pollicis longus tendon may result from dislocation of the thumb MCP joint.
FAQs
The MCP joints are what?
The point where the finger and hand bones meet is called the metacarpophalangeal joint (MCP joint), or knuckle. The fingers have various directions of motion at the MCP joint. They may spread apart, bend, straighten, and move in unison. MCP joints are crucial for gripping and pinching.
What are the metacarpophalangeal joints’ articulating features?
A condyloid synovial joint is what the metacarpophalangeal (MCP) joint is classified as. Each digit is combined to form the palm. The articulation between two hand bones makes up the metacarpophalangeal joint: The metacarpal head is a convex, large articulating surface.
What are the phalanges and metacarpals?
A condyloid synovial joint is what the metacarpophalangeal (MCP) joint is classified as. The palm is created by combining each digit. Two of the hand’s bones articulate to form the metacarpophalangeal joint: The metacarpal head has: a large, convex articulating surface.
How many joints are metacarpophalangeal?
Each finger’s proximal phalanx is connected to the metacarpal bone by five distinct metacarpophalangeal joints.
What are the metacarpophalangeal joints’ main functions?
The concave bases of the proximal phalanges accept the convex heads of the metacarpal bones, which together form each metacarpophalangeal joint. The metacarpophalangeal joints can move in the following directions: flexion, extension, circumduction, adduction, abduction, and restricted movement.
How is the capsule of the metacarpophalangeal joint supported?
Many ligaments and adjacent musculoskeletal structures support the metacarpophalangeal joint capsule. Proper and accessory collateral metacarpophalangeal ligaments support the medial and lateral portions of the joint capsule.
What is the metacarpophalangeal joints’ arterial supply?
The radial and ulnar arteries’ branches provide the arterial supply to the MCP joints. The metacarpophalangeal joints can move in the following directions: flexion, extension, adduction, abduction, circumduction, and fixed rotation.
References
- Metacarpophalangeal (MCP) joints. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/metacarpophalangeal-mcp-joints
- Wikipedia contributors. (2024, December 4). Metacarpophalangeal joint. Wikipedia. https://en.wikipedia.org/wiki/Metacarpophalangeal_joint
- TeachMeAnatomy. (2023, April 15). The metacarpophalangeal joint – ligaments – TeachMeAnatomy. https://teachmeanatomy.info/upper-limb/joints/metacarpophalangeal/
- H. Rupapara. April 5, 2023. The anatomy of the Samarpan metacarpophalangeal (MP or MCP) joint. Physiotherapy Clinic of Samarpan. The metacarpophalangeal joint (MCP) can be found at https://samarpanphysioclinic.com.

2 Comments