Bone Cancer
Bone cancer is a rare disease that occurs when cells in the bone begin to grow out of control. It can develop in any bone but most commonly affects the long bones of the arms and legs. The main types include osteosarcoma, chondrosarcoma, and Ewing sarcoma.
- Symptoms often include persistent bone pain, swelling, fractures, and reduced mobility. The exact cause is unclear, but genetic factors and previous radiation exposure may increase risk.
- Treatment options include surgery, chemotherapy, and radiation therapy, depending on the type and stage of the cancer.
Introduction
- When normal cells in the bone change into abnormal cancer cells that multiply uncontrollably.
- Bone cancer : a rare and serious disease which forms in the bones. Primary bone cancer means the cancer begins in the bones, whereas secondary bone cancer means the cancer spreads to the bones from another part of the body.
- An abnormal growth of tissue inside a bone is called a bone tumor.
- Cell Growth Without Control:
- In cancer, bone cells begin to grow and uncontrollably replace themselves.
A mass or tumor is created inside the bone by these aberrant cells.
- In cancer, bone cells begin to grow and uncontrollably replace themselves.
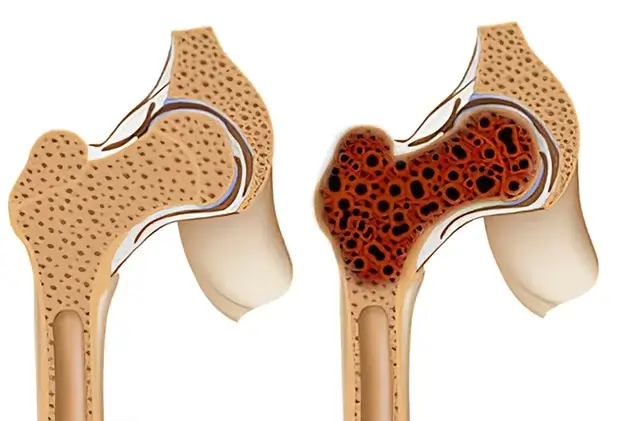
- Bone structure damage:
- The normal structure of the bone is disrupted by the expanding tumor.
It may weaken the bone, increasing the risk of fractures.
- The normal structure of the bone is disrupted by the expanding tumor.
- Effect on the Tissues Around It:
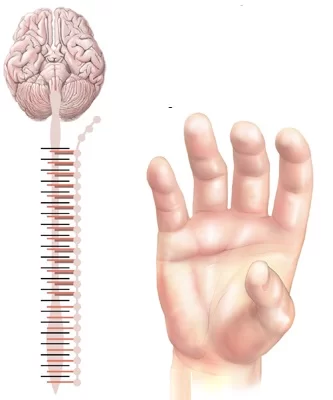
- The tumor may compress or spread to neighboring blood arteries, nerves, and other tissues as it grows.
Types of Bone Cancer
Primary Bone Cancer
Cancer that develops inside the bone itself.x
Osteosarcoma
- Most often occurring in teenagers and young adults, osteosarcoma is the most prevalent form of bone cancer.
- A type of cancer called osteosarcoma arises in the osteoblasts, which are cells that create bones.
- The abnormal bone produced by these malignant cells is weaker than normal bone.
- It most frequently affects the body’s long bones, including: The distal femur, the bottom portion of the thighbone.
- The proximal tibia, the top portion of the shinbone
- The proximal humerus, the upper arm bone
- Symptoms includes
- Pain in the bones (usually worse at night)
Tenderness or swelling close to the affected area
Unaccounted fractures
Restricted range of motion - Although exactly why is unknown but possible contributing variables include:
- Rapid bone growth: Osteosarcoma is more common in teens because it frequently arises during times of rapid bone growth.
- Radiation exposure: The risk may be increased by prior radiation treatment for other cancers.
- Genetic factors: Li-Fraumeni syndrome is one genetic disorder that may raise the risk.
Chondrosarcoma
- Chondrosarcoma is a rare type of cancer that develops in cartilage cells. In numerous areas of the body, such as the nose, ears, and the ends of bones, cartilage—a firm, elastic substance—supports and cushions the body.
- Its source is cartilage cells.
- Typical Places:
The Shoulder, Hip ,Pelvis
In the arms, legs, and ribs, less often.
Growth: May proceed at a slower pace or more rapidly. - Certain varieties have the ability to spread to other bodily areas, usually the lungs.
- The most common type, Conventional chondrosarcoma is graded according to its aggressiveness and rate of growth.
- Dedifferentiated chondrosarcoma: begins as a low-grade tumor and progresses to a more aggressive, high-grade tumor;
- Mesenchymal chondrosarcoma: is uncommon and aggressive; and clear cell chondrosarcoma is less aggressive and frequently found in the upper arm and thigh.
Ewing sarcoma
- Children and young adults are the main victims of the uncommon bone cancer known as Ewing sarcoma.
- Origin: Takes root in the bone or surrounding soft tissue.
- Typical Sites:
Bones of the legs (femur, tibia)
Arms and Pelvis
The ribs
the spine - Bone pain is frequently the first and most prevalent symptom, and it might get worse at night.
- Swelling: Around affected location, a noticeable lump or mass may form.
- Fever: In certain situations, it may be present.
- Unidentified Bones that are fractured may become weaker and more brittle.
- Fatigue and Weight Loss
- Genetic Alterations: A particular genetic defect that arises after birth is the cause of Ewing sarcoma.
Chodroma
- A chondroma is a cartilage-based benign (non-cancerous) tumor.
- The firm, pliable connective tissue known as cartilage supports and cushions many inside components, including the nose, ears, and the ends of bones.
- Types:
- Enchondromas: These develop inside the bone’s marrow cavity.
- Chondromas periosteal: These develop on the bone’s surface.
Typical Sites: - Found most frequently in the little bones of the hands and feet.
- Can also happen in the ribs, thighbone (femur), and upper arm (humerus).
- Signs and symptoms
- Frequently, no symptoms.
- Fractures with pain and swelling (the bone may weaken)
Fibrosarcoma
- A rare kind of soft tissue sarcoma is called fibrosarcoma. Malignancies known as sarcomas start in the body’s connective tissues, which include bone, muscles, tendons, and ligaments.
- Origin: Grows in the fibrous connective tissue that gives the body structure and support.
- Typical Sites:
Legs (most typical)
Arms
Abdominal trunk symptoms: - A bump that is tender or painless is frequently the initial symptom.
- As the tumor expands and presses against nerves, pain may be experienced.
- Reduced range of motion due to swelling
- Feeling numb or tingling.
- Reasons:
- Most of the time, unknown.
- Possible Risk Elements:
- Radiation exposure: The risk may be increased by prior radiation treatment for other cancers.
- Specific genetic disorders:
- A genetic condition that damages nerve tissue is called neurofibromatosis.
An genetic condition called Li-Fraumeni syndrome raises the risk of developing a number of malignancies.
Adamantinoma
- A rare kind of bone cancer is called anaemia.
- Rarity: Less than 1% of all bone tumors are caused by it.
- Location: Usually in the middle part, it mostly affects the tibia (shinbone).
- Age: Young adults (20–40 years old) are most affected.
- Growth: Slow, yet capable of causing harm to the nearby bone and maybe spreading to the lungs.
- Signs and symptoms
- Pain: Usually the initial symptom, it might come on gradually or suddenly.
- Swelling: The shinbone may have a prominent bulge or bulk.
- Limited Range of Motion: The affected leg is difficult to move.
- Shinbone Bowing: The tibia may curve in certain situations.
- Reasons: Unknown, It’s unclear exactly what caused it.
Secondary bone cancer
Metastatic bone cancer
Cancer cells from another area of the body can move (metastasize) to the bone, resulting in metastatic bone cancer.
- Origin: It is not a bone-related primary cancer. Cancer cells move from the initial (primary) cancer location to the bone via the lymphatic or circulatory systems.
- Common Cancers:
- Breast cancer
Breast cancer
Lung cancer
carcinoma of the kidneys
Thyroid cancer - A form of blood cancer called myeloma
- Typical Locations of Bone Involvement:
- The Spine Ribs
The pelvis
Long bones (humerus, femur) - Symptoms: The most frequent and initial symptom is frequently bone pain. It may start off as a dull ache or get worse at night.
- Fractures: Cancer weakens bones, making them more brittle.
- High blood calcium levels caused by bone deterioration are known as hypercalcemia, and they can cause symptoms like disorientation, nausea, constipation, and exhaustion.
- Back discomfort, paralysis, numbness, and maybe a loss of bladder and bowel control can result from spinal cord compression, which is caused by cancer in the spine pressing on nerves.
Rare type of bone cancer
Giant cell tumor
- An uncommon, usually benign (non-cancerous) tumor that develops in the bone is called a giant cell tumor of bone.
- Origin: Found in the bone, usually close to the end of lengthy bones.
- In the surrounding of the knee (upper end of the tibia, lower end of the femur)
- Additional sites: the pelvis, wrist, and shoulder.
- Age: Most prevalent among young people (those aged 20 to 40).
- Growth: Has the capacity to expand quickly and forcefully, which could harm nearby bone.
- Signs: Pain is frequently the initial indication and gets worse as you move.
- Swelling: There may be a visible bulk or lump.
- Having trouble moving the affected joint is known as limited range of motion.
- A fracture occurs when a bone weakens and breaks.
Malignant fibrous histiocytoma
- Sarcomas are malignancies that start in the body’s connective tissues, including muscles, tendons, ligaments, and bone. One kind of soft tissue sarcoma is malignant fibrous histiocytoma (MFH).
- Origin: Takes root in the body’s soft tissues, including deep layers of skin, muscles, tendons, and ligaments.
- Typical Sites:
- The legs, particularly the thighs
- Abdomen, arms, and trunk
- Symptoms:
- A bump that is tender or painless is frequently the initial symptom.
- As the tumor expands and presses against nerves, pain may be experienced.
- Reduced range of motion due to swelling
- Feeling numb or tingling.
- Reasons:
- Most of the time, unknown.
- Possible Risk Elements:
- Radiation exposure: The risk may be increased by prior radiation treatment for other cancers.
Eosinophilic granuloma
- The mildest type of Langerhans cell histiocytosis, a rare condition that causes your body to manufacture an excessive number of immune cells, is called eosinophilic granuloma.
- Benign Tumor: Eosinophilic granulomas are not carcinogenic; they are classified as benign bone tumors.
- Common in Children: Children under the age of ten are typically affected.
- The skull, pelvis, ribs, humerus (upper arm bone), mandible (jaw bone), femur (thigh bone), and spine are the most often affected areas.
- Signs and symptoms
- Frequently no Symptoms: A large number of kids with eosinophilic granulomas don’t exhibit any symptoms.
- Pain: Pain is a common symptom, if it exists.
- Tenderness or swelling could appear close to the affected location.
- Additional Possible Symptoms:
- A headache
- heightened urination and thirst (diabetes insipidus)
- Stiffness (if a joint is close to the growth)
- Skin discoloration above or close to the growth
Symptoms
- Bone pain: the most prevalent and first symptom is frequently bone pain.
- The discomfort could be:
- Persistent: Lasting a lengthy period.
- Night time worsening: Usually more obvious when you’re sleeping.
- Localized: Focused on a particular region.
- Deep and aching: This type of pain might be mild or more intense, throbbing.
- Swelling: A significant lump or swelling may appear around the bone’s injured location.
- Tenderness: The bone’s surrounding tissue may feel sensitive to the touch.
- Limited Range of Motion: Inability to move the affected joint because of discomfort or edema.
- Unaccounted-Fractures: Even mild injuries might cause the bone to deteriorate and break more readily than usual.
- Fatigue: The state of being abnormally exhausted despite getting enough sleep.
- Weight Loss: Sometimes people lose weight without knowing reason.
- Fever: There may be a fever in some situations.
Diagnosis
- A comprehensive evaluation by a healthcare professional is necessary to determine the cause of bone pain.
- The following is a general outline of the diagnostic process:
- Medical History and Physical Examination: Detailed Medical History, The doctor will collect information about your symptoms, such as: Location and nature of the pain: Where exactly does it hurt? Is it sharp, dull, aching, or throbbing?
- Onset and duration: When did the pain start? Is it constant or intermittent? Aggravating and relieving factors : What causes the pain to worsen (e.g., activity, weight-bearing) or what relieves it (e.g., rest, medication)?
- Other symptoms: Any accompanying symptoms like swelling, redness, fever, fatigue, or weight loss? Previous medical history: Any surgeries, injuries, or medical conditions?
Medications: Any medications you are currently taking? - Physical Examination: The physician will closely inspect those affected region, looking for:
- Swelling: Any lumps or swelling that are noticeable.
- Tenderness: Touch-sensitive areas.
- Range of motion: Any restrictions on how the affected joint can move.
- Any odd forms or irregularities in the bone are called deformities.
Imaging examinations:
- X-ray: Frequently the initial imaging test carried out.
- Can show problems such as arthritis, bone cancers, and fractures.
- Magnesium resonance imaging, or MRI, produces fine-grained pictures of bone cancers, soft tissues, and bone marrow.
- Compared to X-rays, a CT scan (Computerized Tomography) produces cross-sectional images of the body that provide more detailed information.
- A radioactive tracer is used in a bone scan to find regions of elevated bone metabolism, which may be a sign of malignancies, infections, or fractures.
The biopsy
- A biopsy could be required in certain circumstances in order to collect a sample of bone tissue for microscopic inspection.
- Two types: needle biopsy and open biopsy
Staging Bone Cancer
The American Joint Committee on Cancer’s (AJCC) TNM method is used to determine the stage of bone cancer
TNM system
T (tumor): explains the primary tumor’s size and scope.
- T1: The tumor’s largest dimension is 8 cm or smaller.
- T2: The tumor’s largest dimension exceeds 8 cm.
- T3: The same bone contains many cancerous areas.
N (Node):
- Explains if adjacent lymph nodes have been affected by the malignancy.
- N0: There are no cancerous cells in the lymph nodes nearby.
- N1: Nearby lymph node cancer cells.
M (Metastasis):
- Explains if the disease has spread to other body parts.
- M0: No metastases to other places.
- M1a: Lung metastatic disease.
- M1b: Spreading beyond the lung to other areas of the body.
Grouping of Stages Overall:
- Stage 1: Small, confined, low-grade tumor (T1 N0 M0)
- Stage 2: Larger, higher-grade tumor that has not spread (T2/3 N0 M0)
- Stage 3: Any size tumor that has migrated to lymph nodes (T1-3 N1 M0)
- Stage 4: Any T, Any N, or M1 distant metastases are present.
Treatment
Surgical approach
This is often the primary treatment.
Limb-sparing surgery
- The goal of limb-sparing surgery, sometimes referred to as limb-salvage surgery, is to remove only the diseased area of the bone in order to preserve a limb that has been affected by bone cancer. When possible, this method is chosen over amputation since it greatly enhances a patient’s functional ability and quality of life.
- Tumor Removal: To assure the patient that the tumor is completely removed, the surgeon carefully removes the diseased bone along with a margin of healthy tissue surrounding it.
- Reconstruction: One of the following is used to replace the collected bone.
Metal implant (prosthesis): To give structural support, a synthetic implant is placed. - Bone graft: To replace the removed bone, bone tissue is either auto grafted from another region of the patient’s body or allografted from a deceased donor.
- Rehabilitation: To rehabilitate and regain full function of the limb, extensive physical and occupational treatment is essential.
- limb-sparing surgery considered when,The tumor has not spread to other areas of the body; it is confined.
- Because of its size and placement, the tumor may be completely removed without impairing limb function.
- The patient is in sufficient general health to endure the procedure and the ensuing recovery.
Amputation
- Necessary if the tumor cannot be completely removed or limb/joint function cannot be maintained; this is most frequently the case with pelvic cancers whose position or extent precludes limb-sparing.
- Despite previous surgeries, it is occasionally required for malignant sarcomas or recurring tumors.
- Prosthetic limbs may now bend and rotate for better function .
- A typical long-term adverse effect that requires pain management is phantom limb pain.
- Strength, balance, and movement coordination with a prosthesis are the main goals of rehabilitation.
Bone Reconstruction
- One of the most important parts of limb-sparing surgery for bone malignancy is bone rebuilding.
- In order to restore the limb’s structural integrity and functionality, the excised malignant bone must be replaced with an appropriate substance.
- Method of bone reconstruction is Metal prosthetics, or implants:
- These are synthetic implants composed of metals such as stainless steel or titanium.
- They offer structural support and can be tailored to meet the patient’s unique requirements.
- Rods, plates, and specially designed prostheses are examples of implant types.
- Grafts of bone:
- Autograft: The patient’s hip or fibula (a smaller bone in the lower leg) are two examples of other body parts from which bone tissue is taken.
- Allograft: A deceased donor’s bone tissue is used.
Composite grafts: A mix of bone transplants and metal implants.
Radiation therapy
- Radiation Therapy: An Effective Treatment for Bone Cancer
- High-energy rays are used in radiation therapy, a cancer treatment, to destroy cancer cells. It is essential for treating bone cancer and is frequently combined with chemotherapy and surgery.
- How Does Bone Cancer Radiation Therapy Operate?
Radiation therapy applies targeted radiation doses to the malignant region. - These high-energy radiations harm cancer cells’ DNA, stopping them from proliferating and reproducing.
- Bone Cancer Require Radiation Therapy when
- Prior to Neoadjuvant Surgery:
- To reduce the tumor’s size so that surgery can remove it more easily.
- To increase the likelihood that limb-sparing surgery will be effective.
- Following Adjuvant Surgery:
- To eliminate any cancer cells that could have remained after surgery.
- As an alternative to surgery:
- For tumors that, because to their location or size, cannot be surgically removed entirely.
- For patients with underlying medical issues that make them unsuitable candidates for surgery.
- For Symptom Relief: To manage pain and additional tumor-related symptoms, such as spinal cord or nerve compression, in circumstances where a cure is not possible
Types of Radiation Therapy
- External Beam Radiation Therapy (EBRT) is one type of radiation therapy used to treat bone cancer.
- the most prevalent kind, in which radiation is administered externally by a machine.
Stereotactic body radiation therapy (SBRT) and intensity-modulated radiation therapy (IMRT) are two methods that minimize harm to nearby healthy tissues while enabling more accurate tumor targeting. - Brachytherapy:
- Include positioning radioactive sources close to or inside the tumor.
- Utilized in some circumstances, such as during surgery for intraoperative radiation treatment (IORT).
- Side effects of radiation therapy
- Skin irritation: The treated area’s skin becomes red, dry, and sensitive.
- Fatigue: Weakness and discomfort.
- Vomiting and nausea: Although less frequent with contemporary radiation treatments.
- A reduction in blood cell counts may result from bone marrow suppression.
- Long-term adverse effects: The risk of developing secondary malignancies, bone weakening, and harm to adjacent organs may vary depending on the location and intensity of radiation exposure.
Chemotherapy and Targeted Therapy in Bone Cancer
- Systemic treatments for bone cancer include chemotherapy and targeted therapy, which can affect cancer cells all over the body. For many individuals, these treatments are essential in boosting their results.
- For bone cancer, common chemotherapy medications include:
- Ifosfamide, Cisplatin, and Doxorubicin,Etoposide
- Although chemotherapy can effectively cure bone cancer,
- There are some potential side effects, including:
- Vomiting and feeling queasy
Loss of hair
Weariness
Sores in the mouth
Having diarrhea
A higher chance of infection - The type and stage of bone cancer, along with the patient’s general health, will determine the best course of treatment. Before choosing a course of treatment, it is crucial to discuss the advantages and disadvantages of chemotherapy with a physician.
- Drugs are used in targeted therapy for bone cancer to target particular flaws in cancer cells. Compared to chemotherapy, this kind of treatment is less likely to harm good cells, but it might not work for all forms of bone cancer.
- Denosumab is one approved targeted therapy medication for the treatment of bone cancer.
- Bone cancer may also be treated with the following targeted therapies:
- Kinase inhibitors: These medications target proteins that aid in the growth and metastasis of cancer cells. A uncommon kind of bone cancer called chordomas is frequently treated with kinase inhibitors.
- Immunotherapy: This kind of treatment supports the body’s defenses against cancer. Although they are not yet generally accessible, immunotherapy medications are being researched for the treatment of bone cancer.
Care and Rehabilitation Support
Helpful Care
- The broad variety of services included in supportive care are intended to manage treatment side effects and enhance general comfort. Among the crucial facets of supportive care are:
- Pain management: The treatment of bone cancer can be painful. Effective pain management techniques, such as drugs, nerve blocks, and other treatments, can be created by pain management specialists.
- Handling Fatigue: A typical side effect of cancer and its treatments is fatigue. Fatigue can be managed with strategies including exercise, energy conservation, and dietary advice.
- Management of Nausea and Vomiting: Anti-nausea drugs and dietary changes can help control these chemotherapy side effects.
- Handling Mouth Sores: Using specialist mouthwashes and practicing good oral hygiene can help prevent and manage mouth sores.
- Nutrition and Hydration: Throughout therapy, it’s critical to maintain proper nutrition and hydration. Personalized dietary advice can be obtained from a licensed dietitian.
- Psychological and Emotional Assistance:
- Cancer can affect a person’s emotions profoundly. Patients can manage their anxiety, depression, and other emotional difficulties with the aid of counseling, support groups, and other psychosocial interventions.
Rehabilitation exercises
- Physical Therapy: Strength, flexibility, range of motion, and balance can all be enhanced with the assistance of physical therapists. Exercises to enhance coordination and gait can also be taught by them.
- Occupational Therapy: Occupational therapists can assist patients in creating plans for independent living and adjusting to changes in their everyday routines. This could entail employment retraining, house changes, and assistive technology.
- Prosthetics and Orthotics: Prosthetic limbs and other supporting devices can be made and fitted by prosthetists and orthotists for patients who have had limb-sparing surgery or amputation.
- Management of Lymphedema: Certain cancer treatments may result in lymphedema, a swelling caused by fluid accumulation.
- To treat this illness, lymphedema therapists can offer customized compression and massage treatments.
Psychological and emotional assistance
- A person’s emotional and psychological health can be greatly impacted by a cancer diagnosis, particularly bone cancer.
- Typical Psychological and Emotional Issues:
- Significant anxiety can be caused by a fear of the unknown, adverse treatment effects, recurrence, and the influence on day-to-day functioning.
- Depression: Feelings of sorrow, helplessness, and a loss of interest in activities might result from the emotional strain of receiving a cancer diagnosis.
- Fear and Uncertainty: Receiving a diagnosis and not knowing how a therapy will turn out can be quite stressful.
- Issues with Body Image: Self-esteem may be impacted by physical changes caused by surgery, adverse treatment effects (such as hair loss), or the requirement for prosthesis.
- Grief and Loss: Grief and mourning can be caused by facing the possibility of losing one’s ability to function, one’s independence, or even one’s life.
- Financial Concerns: The expenses of medical care, missed wages, and possible disability can lead to a great deal of financial strain.
Support That Is Available
- Psychotherapy: Cognitive-behavioral therapy (CBT) and other talking treatments can assist people in managing their emotional problems, such as depression and anxiety.
- Support groups: Making connections with people who have gone through comparable struggles helps to understanding and a sense of community.
- Counseling: Communication problems, relational difficulties, and emotional distress can all be addressed through individual or family counseling.
- Social Work Support: Social workers can aid with practical issues such as obtaining community services, managing insurance, and financial support.
- Support from Loved Ones: It’s critical to have open lines of communication with family and friends.
- Encourage family members to lend a sympathetic ear, practical help, and emotional support.
- Mind-Body Techniques: Stress and anxiety can be reduced by practicing relaxation techniques like yoga, deep breathing, and meditation.
Getting Assistance
- Healthcare Team: Social workers, nurses, and oncologists can all be referred to support groups and mental health specialists by your healthcare team.
- Cancer organizations: Resources and support services are available for those with cancer from groups such as the National Cancer Institute and the American Cancer Society.
- Numerous internet resources provide cancer patients communal forums, support, and information.
Prevention and perspective
Prevention strategies
Continue to Lead a Healthful Lifestyle:
- A balanced diet should emphasize lean protein, entire grains, fruits, vegetables, and low-fat dairy products. For strong bones, make sure you’re getting enough calcium and vitamin D.
- Frequent Physical Activity:
- Take part in weight-bearing activities on a regular basis, such as jogging, walking, or weightlifting.
- Every week, try to get in at least 150 minutes of moderate-intensity exercise.
Reduce Risk Elements:
- Reduce Radiation Exposure: Reduce needless radiation exposure from medical procedures.
- Take the appropriate safety measures if you work in an environment where radiation exposure is a possibility.
- Avoid Dangerous Substances: Reduce your exposure to substances that are known to raise your chance of developing cancer, such as those present in particular locations or jobs.
- Give Up Smoking: Smoking raises your risk of developing a number of malignancies, including several that can damage your bones.
Early Identification:
- Frequent Checkups: Make an appointment for routine checkups with your physician, particularly if you have a family history of cancer or other risk factors.
- As soon as you notice any strange symptoms or changes in your bones, report them.
Genetic Guidance:
- Consider genetic counseling to determine your risk and go over possible preventive steps if bone cancer or other malignancies run in your family.
Outlook and rates of survival
- The prognosis and survival rate for bone cancer vary depending on several factors, including the type of cancer, stage at diagnosis, location of the tumor, and overall health of the patient.
- Here’s a general overview:
- Overall Survival Rate: The five-year survival rate for all bone cancers combined is about 70%. However, this number can vary significantly depending on the specific type and stage of the cancer.
- Type of Bone Cancer: Some types of bone cancer have better prognoses than others. For example, chondrosarcomas tend to have a higher survival rate compared to osteosarcomas.
- Stage at Diagnosis: Early-stage bone tumors that are still limited to the bone have a considerably better prognosis than those that have migrated to other regions of the body.
- Location of the Tumor: Tumors located in certain areas, such as the limbs, may be easier to treat and have a better prognosis compared to tumors in the pelvis or spine.
- Overall Health: Patients with good overall health and no other significant medical conditions tend to have a better prognosis.
FAQs
How can bone cancer be identified early?
X-rays. When a bone tumor of any kind is detected, an x-ray of the bone is frequently the first test performed.
Which seven indicators point to bone cancer?
Pain. Even if you’re sleeping, you may experience pain or tenderness most of the time.
swelling. It is not usually possible to see or feel a lump, but you may have some swelling.
Moving around is problematic…
A fractured bone….
Exhausted (fatigued)…
A fever, or high temperature…
Loss of weight
What causes bone cancer to begin?
When DNA alterations occur in cells within or close to a bone, bone cancer begins.
Is it possible to cure bone cancer?
In otherwise healthy individuals whose cancer has not spread, bone cancer is typically considerably easier to cure.
What are the symptoms of bone cancer?
bone cancer can result in discomfort, edema, and trouble moving. Fatigue, a lump, and inexplicable weight loss are further symptoms.
Is bone cancer painful?
The most typical indication of bone cancer is pain near the tumor. The pain may not always be present at first. while the bone is used, like while walking for a tumor in a thigh bone, it could get worse at night.
Referances
- Bone cancer. (2024, December 27). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17745-bone-cancer
- Stuart, A. (2024, December 17). Bone cancer. WebMD. https://www.webmd.com/cancer/bone-tumors
- Macon, B. L. (2022, February 16). Bone cancer: types, causes, symptoms, and more. Healthline. https://www.healthline.com/health/bone-cancer
- NCI Dictionary of Cancer Terms. (n.d.). Cancer.gov. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/bone-cancer
- Bone Cancer: diagnosis and treatment principles. (2018, August 15). PubMed. https://pubmed.ncbi.nlm.nih.gov/30215968/