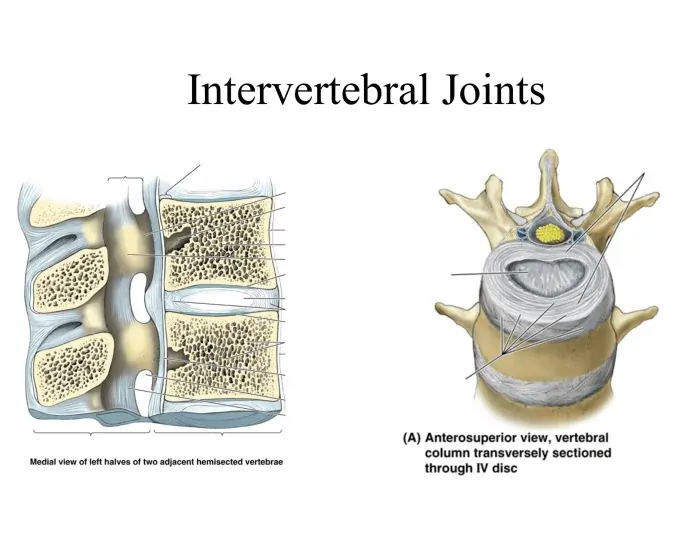
Intervertebral Joints
Three intervertebral joints connect each neighboring vertebra from the axis to the sacrum: two between the facets of adjacent vertebral arches and one between the vertebral bodies (zygapophysial joints, also known as facet joints).
Introduction
The intervertebral joints join the vertebrae of the vertebral column which are closely nearby. Three distinct joints make up each intervertebral joint: two zygapophyseal (facet) joints and one intervertebral disc joint (intervertebral symphysis).
Articular surfaces
The intervertebral symphyses, or intervertebral disc joints, go from the C2 to the S1 vertebral levels. Adjacent vertebral bodies and the intervertebral disc that sits between them create them. At the C0-C1 and C1-C2 vertebral levels, there are no intervertebral discs.
Both the superior and inferior surfaces of the vertebral bodies have a lot of texture. Their centers are very asymmetrical, with a modest smoothness at the edges. Additionally, the vascular foramina that penetrates the joint surfaces exacerbates their irregularity. The basivertebral veins and intraosseous nutritional arteries, which deliver and remove blood from the vertebral bodies, are transmitted by these foramina.
In the vertical plane, the joint surfaces can be sellar (concave) with raised borders that resemble lips or relatively flat. In the cervical vertebrae, where they create the uncovertebral joints, these raised borders, also known as uncinate processes, are particularly noticeable. As the spinal cord passes through the vertebral foramen, the articular surfaces appear convex anteriorly and concave posteriorly in the horizontal plane. The cervical vertebrae are an exception, as their posterior joint surfaces may be nearly flat.
The vertebral bodies’ discal surfaces are covered with vertebral end plates. They are irregular and less than 1 mm thick, with the center being the narrowest. Both bone and hyaline cartilage make up vertebral end plates in the early stages of life. In adulthood, the cartilage mineralizes and is replaced by bone. The vertebral end-plate’s roles include strengthening the intervertebral disc joint and absorbing shock.
Fibrocartilaginous intervertebral discs separate the articular surfaces of successively neighboring vertebral bodies. In addition to the bony vertebral rim, they also stick to the vertebral end plates. Through ring apophyses, it is attached to the vertebral bodies. The anterior region of the wedge-shaped intervertebral discs is especially thick. A nucleus pulposus and an annulus fibrosus make up each intervertebral disc.
The inner core of the intervertebral disc is formed by the nucleus pulposus. It is very pliable, gelatinous, and soft. These features make it easier for the intervertebral disc and joint to move, particularly in the cervical area. The nucleus pulposus is surrounded by the peripheral annulus fibrosus. Comprising fibrocartilage and collagen, it has a lamellar structure. It is therefore less flexible and more rigid than the nucleus pulposus. The annulus fibrosus reinforces the vertebral column by enclosing the nucleus pulposus and connecting the vertebrae.
Ligaments and joint capsule
There isn’t a joint capsule around intervertebral disc joints. The anterior and posterior longitudinal ligaments give them stability.
There are two longitudinal ligaments, although the anterior longitudinal ligament is the stronger. It reaches the pelvic surface of the upper sacrum from the root of the occipital bone. It connects to the anterior parts of the vertebral bodies, the annulus fibrosis of the intervertebral discs, and the vertebral end plates along the way. The anterior longitudinal ligament’s function is to provide anterior support for the vertebral column.
In the vertebral canal of the vertebral column, directly in front of the spinal cord, is the posterior longitudinal ligament. From the second cervical vertebra to the first sacral vertebra, it stretches. The posterior parts of the intervertebral discs, the vertebral end plates, and the edges of the vertebral bodies are where it attaches along the route. This ligament’s function is to support the back of the vertebral column.
Innervation
From the anterior ramus of the spinal nerve, the sinuvertebral nerve innervates the zygapophyseal joints and the intervertebral disc. The spinal nerve’s gray communicating branch provides sympathetic input to the sinuvertebral nerve as it travels. The medial branch of the posterior ramus of the spinal nerve also innervates the zygapophyseal joint, unlike the intervertebral disc joint.
Blood supply
The segmental arteries of the vertebral column, including the costocervical trunk and vertebral, ascending cervical, posterior intercostal, lumbar, iliolumbar, and lateral sacral arteries, supply arterial blood to the intervertebral joints. The posterior spinal branches of these segmental arteries deliver blood to the zygapophyseal joints and the most peripheral region of the nucleus fibrosis. Additionally, they supply the articular surfaces of the vertebral bodies with peripheral, metaphyseal, and nutritional arteries. The avascular intervertebral discs receive oxygen and nutrients by diffusion from this point.
Blood flows into the spinal and basivertebral veins from the intervertebral joints. These then enter into the intervertebral veins via the vertebral venous plexuses.
Movements
The intervertebral disc joint is classified structurally as a fused, fibrocartilaginous symphysis. Functionally speaking, nonetheless, it is regarded as an amphiarthrosis that allows for a restricted range of motion. The intervertebral disc can translate, tilt, rock, and compress due to its soft and pliable nature, which expands the spinal column’s range of motion.
According to structural classification, the zygapophyseal joint is a plane synovial joint. It operates similarly to a uniplanar diarthosis, permitting nonaxial motions in a single plane (translation). However, because of the various orientations of the articular processes in each region of the vertebral column—forward flexion and extension in the lumbar spine, lateral flexion and rotation in the cervical spine, and lateral flexion and rotation in the thoracic spine—zygapophyseal joints allow the spine to move in multiple planes and directions. Thus, the zygapophyseal joints guide movement, whereas the intervertebral disc joints constitute the main constraint on the spine’s range of motion.
When the intervertebral joints are combined, the vertebral column can move multiaxially in three degrees of freedom (the average maximum glenohumeral active RoM is displayed in brackets):
- Cervical spine
- (Anterior) flexion (25°) – Extension (85°)
- Bilateral flexion (40°)
- Bilateral axial rotation (50°)
- Thoracic spine
- (Anterior) flexion (30-40°) – Extension (20-30°)
- Bilateral flexion (20-25°)
- Bilateral axial rotation (35°)
- Lumbar spine
- (Anterior) flexion (55°) – Extension (30°)
- Bilateral flexion (20-30°)
- Bilateral axial rotation (1-2°)
The superior vertebral body moves anteriorly during spinal flexion, leaning forward and squeezing the anterior intervertebral disc segments. As a result, the superior vertebra’s inferior articular surface moves both superiorly and anteriorly to the inferior vertebra’s superior articular surface, resembling a seesaw. The superior zygapophyseal joint widens posteriorly as a result. The articular process’s 45° position within the sagittal plane allows the lumbar spine to have a higher range of motion in flexion. The zygapophyseal joints are less restricted and the vertebral bodies can slide more anteriorly since flexion and extension also occur in the sagittal plane.
The thoracic cage (thoracic spine only), the posterior longitudinal ligament, the ligament flava, the nuchal ligament (cervical spine alone), the joint capsule of the zygapophyseal joint, and the tone of the deep, or intrinsic, muscles of the back, which are placed paravertebrally all limit flexion.
The reverse happens with spinal extension. The posterior part of the intervertebral discs is compressed, tipped back, and slid posteriorly by the superior vertebral body. The anterior region of the superior zygapophyseal joint widens as the inferior articular surface shifts inferiorly and posteriorly. Since the articular process affects the broad spinous processes of the vertebrae across the thoracic and lumbar spines, extension is much reduced in these regions as opposed to the cervical area. The anterior longitudinal ligament’s tension, the posterior vertebral processes’ impaction, and the tone of the anterior neck (only the cervical spine) and anterior abdominal muscles (only the thoracic spine) all limit extension.
The ipsilateral (right) articular processes extend when the vertebral column is bent laterally to the right, whereas the contralateral (left) articular processes flex at the zygapophyseal joints. The superior vertebra’s right inferior articular process glides inferiorly and posteriorly with the inferior vertebra’s superior articular process. Concurrently, the intervertebral disc’s left side is stretched while its right side is compressed.
The opposite happens when the vertebral column flexes contralaterally to the left; the right zygapophyseal joints flex and the left ones lengthen. Since the vertebral column cannot do pure lateral flexion, it must couple this movement with a small amount of axial rotation. Due to its extremely limited axial rotational capacity, the lumbar spine is an exception. Since the articular processes are placed obliquely, 45° between the transverse and frontal planes, the cervical area experiences the highest lateral flexion. Their ability to easily connect axial rotation (transverse plane) with lateral flexion (frontal plane) is therefore enhanced.
Compression of the intervertebral discs, impaction of the articular processes, tension of the contralateral trunk muscles, ligamenta flava, and intertransverse ligaments (thoracic, lumbar spines only) all limit lateral flexion. The thoracic cage’s form changes in tandem with lateral flexion in the thoracic area of the spinal column.
The inferior process of the superior vertebra slips outwardly and laterally to the superior process of the inferior vertebra during axial rotation. The result is a shared axis around which the vertebral bodies spin concerning each other. A simultaneous twisting of the intervening intervertebral disc draws the vertebrae closer together. It has the same effect as squeezing a washcloth repeatedly. There is never complete rotation in the spinal column; instead, there is always some lateral flexion.
The restricted articular space of the articular processes in the lumbar spine severely restricts rotation. The rotation of the articular processes immediately affects the tiny space between them. The orientation of the lumbar articular surface in the sagittal plane is another factor contributing to the restriction. Rotation is restricted by the impaction of opposing articular processes, the tension in the ligamentS flava, supraspinous and interspinous ligaments, and opposing trunk muscles, such as the abdominal obliques. The lumbar spine’s articulated ribs rotate as a result of the vertebrae’s axial rotation.
The intervertebral joints are in the open-packed (resting) position halfway between flexion and extension, and in the closed-packed position, they are fully extended. Extension and equally limited lateral flexion and rotation are the capsular patterns of the joints. Through manual manipulation, additional accessory (arthrokinematic) motions can occur at the intervertebral joints. At the cervical intervertebral joints, traction and lateral sliding may take place. The thoracic intervertebral joints allow for rocking, apposition, separation, and distance. The last auxiliary movements that can occur in the lumbar spine are rotation and anterior gliding.
Muscles acting on the intervertebral joint
The intervertebral joints move because of the muscles in the neck and trunk.
| Flexion | Scalenus anterior, rectus abdominis, longus capitis, longus colli, sternocleidomastoid, and abdominal oblique muscles |
| Extension | The quadratus lumborum, rotatores, interspinal, semispinalis multifidus, iliocostalis, spinalis, trapezius, splenius capitis, splenius cervicis, and longissimus |
| Lateral flexion | Longus colli, levator scapulae, splenius capitis, splenius cervicis, iliocostalis, longissimus, splenius thoracic, semispinalis cervicis, semispinalis thoracis, multifidus thoracic, multifidus lumborum, intertransversarii, quadratus lumborum, trapezius, scalenus medius, scalenus posterior, sternocleidomastoid, longus colli, and splenius cervicis |
| Axial rotation | Multifidus thoracic, multifidus lumborum, rotatores, lavatories costarum, abdominal oblique, transversus abdominis, splenius capitis, splenius cervicis, longissimus capitis, sternocleidomastoid, and scalenus anterior Muscles acting on the intervertebral joint |
Muscles acting on the intervertebral joint
At the intervertebral joints, the cervical prevertebral muscles (longus colli, longus capitis) are the primary flexors that move the vertebral column. The sternocleidomastoid, scalenus anterior, and anterolateral abdominal muscles (rectus abdominis and abdominal obliques) assist them farther inferiorly in the thoracic and lumbar regions. The spinal column is flexed and the extensors’ activity is countered by the bilateral tension of these muscles. An upright posture is maintained when these opposing muscles contract at the same time.
The suboccipital and trapezius muscles assist the posterior cervical muscles (splenius capitis, splenius cervicis), which are the main extensors of the intervertebral joints. The deep (intrinsic) back muscles that work on the spine in the lumbar and thoracic areas are the interspinal, transversospinales, and erector spinae. The spinal column stretches and hyperextends when both sides contract. They are regarded as the primary postural muscles and work in opposition to the flexors.
A unilateral contraction of the corresponding muscles can also cause the aforementioned muscles to stretch laterally. At the same time, the spine will flex ipsilaterally as the contralateral muscles relax. Since these muscles extend superiorly and either anteriorly or posteriorly for the intervertebral joints’ rotation axis, they can also rotate axially. The vertebrae will therefore spin to one another when the muscle fibers contract.
Clinical significances
For spinal mobility, stability, and load bearing, the intervertebral joints are essential. Their malfunction can result in some clinical disorders that impair movement, produce discomfort, and create neurological symptoms. The primary clinical relevance of the intervertebral joints is listed below:
Degenerative Disc Disease (DDD)
- Degeneration of the intervertebral discs with age.
- Causes discomfort, osteophyte development, and disc height reduction.
- Can be a factor in persistent stiffness and lower back discomfort.
- Through an annulus fibrosus rip, the nucleus pulposus emerges.
- L4-L5 and L5-S1 are frequently affected, resulting in sciatica, or pain that travels down the leg.
- Can result in numbness, weakness, and compression of the nerve.
Spinal Stenosis
- Spinal canal narrowing that compresses the spinal cord or nerve roots.
- Causes weakness, numbness, pain, and trouble walking.
- Can happen in the lumbar or cervical spine.
Spondylolisthesis
- One vertebra slides forward over another as a result of facet joint instability.
- Commonly observed in L5-S1, it causes sciatica, back pain, and abnormalities in gait.
- In severe cases, surgical fusion can be necessary.
Spondylosis (Spinal Osteoarthritis)
- Spinal joint wear and tear arthritis.
- Causes disc degeneration and bone spur (osteophyte) development.
- May cause discomfort, rigidity, and compression of nerves.
Vertebral Compression Fractures
- Frequently caused by trauma, tumors, or osteoporosis.
- Leads to kyphosis (a malformation of the hunchback), extreme pain, and height loss.
Discitis & Spondylodiscitis (Spinal Infections)
- Infection of the nearby vertebrae and intervertebral disc.
- Leads to strong back pain, fever, and possible neurological deficits.
- Frequent pathogens: Staphylococcus aureus, Mycobacterium tuberculosis (Pott’s disease).
FAQs
Intervertebral joints: are they mobile?
Complex structures that provide multidirectional motion, and spinal intervertebral joints have been the subject of numerous experimental investigations that have shown moment-rotation response.
Which two intervertebral joints are they?
Each segment has two joints. The superior and inferior joints are the upper and lower, respectively. Each inferior joint fits into the superior joint of the vertebra immediately below it due to the alignment of the joints. A little bridge called the interarticular connects the two joints.
What kinds of vertebral joints are there?
The vertebral column may move in a variety of ways because of its many joints. The vertebral bodies, vertebral arches, craniovertebral joints, costovertebral joints, and sacroiliac joints constitute the usual organization for these joints.
The intervertebral joints are what?
Intervertebral synovial facet joint: each vertebra has two superior and two inferior articular facets that are coated in articular cartilage and are located on the vertebral arch, between the pedicle and lamina. Above and below, these articulate with the corresponding facets of the vertebrae.
Which names are used for the vertebral joints?
Craniovertebral joints, joints between vertebral bodies, zygapophyseal joints, costovertebral joints, and sacroiliac joints are all considered to be part of the vertebral column.
Do intervertebral joints consist of cartilage?
The manubriosternal joint, which connects the manubrium to the sternum’s body, intervertebral discs, and the pubic symphysis are a few instances of secondary cartilaginous joints in human anatomy.
In what way do the intervertebral joints move?
Complex structures and spinal intervertebral joints provide flexion-extension (FE), lateral bending (LB), and axial rotation (AR) action.
References
- Knipe, H., & Gunasena, R. (2016). Intervertebral joint. Radiopaedia.org. https://doi.org/10.53347/rid-44861
- Intervertebral joints. (2023, October 26). Kenhub. https://www.kenhub.com/en/library/anatomy/intervertebral-joints