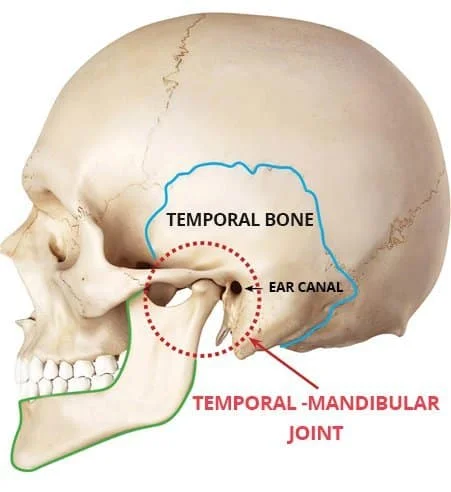
Temporomandibular joint
The temporomandibular joint (TMJ) connects the jawbone (mandible) to the skull (temporal bone) on both sides of the face. It allows movements like chewing, speaking, and yawning.
The joint consists of bones, cartilage, muscles, and a disc that cushions movements. Dysfunction in the TMJ can lead to pain, clicking sounds, or restricted jaw movement.
Introduction
A synovial joint that enables the intricate movements required for life is the temporomandibular joint (TMJ), also known as the jaw joint. This joint is between the temporal bone’s mandibular fossa and the mandibular condylar head. This system, which includes the TMJ, teeth, and soft tissue, is involved in speech, eating, and breathing.
The TJM is classified as a ginglymoarthrodial joint due to its ability to rotate in the sagittal plane and translate on its axis, which causes additional movement. Numerous passive forces, including passive tension of the muscles and ligaments, limit these motions.
TMJ dysfunction can lead to excruciating discomfort and restrictions in one’s lifestyle.
Accurate diagnosis and suitable therapy depend on a thorough understanding of the anatomy of the TMJ and associated tissues.
Structure
These include the articular disc, mandibular condyles, temporomandibular ligament, sphenomandibular ligament, temporomandibular ligament, articular surface of the temporal bone, lateral pterygoid muscle, and joint capsule.
Anatomy
The squamous portion of the temporal bone, known as the glenoid fossa, hosts the jaw’s condyle and makes up the cranial side of the TMJ. We locate a bone piece termed the postglenoid process laterally to the posterior articular ridge, the fossa’s posterior section.
A medial bone prominence at the posterior border of the zygomatic bone is formed by the articular eminence, which is the anterior limit of the temporal bone’s glenoid fossa. We locate a bone piece termed the postglenoid process laterally to the posterior articular ridge, the fossa’s posterior section. The upper wall of the external acoustic meatus is formed in part by the postglenoid process region.
The medial bone prominence at the posterior border of the zygomatic bone is formed by the articular eminence, which is the anterior limit of the temporal bone’s glenoid fossa. Anterior to the fossa and the base of the skull is the articular eminence, which is reached by the slightly slanted preglenoid plane. The articular eminence is located anterior to the pit, as is the base of the skull, and is reached by the slightly slanted preglenoid plane. The articular disk and the condyle can move freely and easily in this region. A bone ridge called the articular tubercle is located close to the zygomatic process’s root on the lateral surface of the articular eminence.
Comparing the mediolateral and anteroposterior regions of the glenoid fossa, the latter is wider. The upper region of the mandible is represented by the glenoid fossa’s inferior articular surface. It is composed of the mandibular condyle, which has a transverse dimension of roughly 15 to 20 mm and an anteroposterior measurement of roughly 8 to 10 mm.
Both the front (about 2 mm) and posterior (approximately 3 mm) portions of the cartilaginous disc, with a narrower diameter in the middle, are part of the biconcave or oval articular disc that covers the condyle and interposes beneath the glenoid fossa. The disk’s anterior region is made up of a fibrous layer on the bottom and a layer of fibroelastic fascia on top. To keep the disc from slipping as the mouth opens, the upper part makes touch with the postglenoid process. The bottom part of the disk is responsible for preventing the disk from rotating too much about the mandibular condyle.
The joint capsule, articular eminence, condyle, and upper region of the lateral pterygoid muscle are all in touch with the anterior part of the articular disk.
Attached to the mandibular condylar structure are the medial and lateral aspects of the cartilaginous disc. The disc’s edges partially merge with the fibrous capsule that envelops the joint.
Joint
The TMJ is a condylar, hinge-type, synovial joint. Fibrocartilaginous surfaces and an articular disc, which separates the joint into two chambers, are components of the joint. These superior and inferior articular cavities are bordered by separate superior and inferior synovial membranes.
Capsule
Attached to the neck of the mandibular condyle below, and the perimeter of the mandibular fossa and the articular tubercle directly in front is the articular capsule, also known as the capsule ligament. Its flexible attachment to the mandibular neck permits unrestricted mobility.
Articular disc
It is the articular disc that makes the temporomandibular joint distinctive. The disc, which is situated between the mandibular fossa of the temporal bone and the head of the mandibular condyle, is made of dense fibrocartilagenous tissue. The temporomandibular and sternoclavicular joints are two of the few synovial joints in the human body that have an articular disc. Each joint has two compartments, the lower and upper chambers, separated by the disc. These two spaces are called synovial cavities, and they are made up of an upper and a lower synovial cavity.
The fluid that fills these spaces is made by the synovial membrane that lines the joint capsule. The form of the disk is biconcave. Furthermore, the superior head of the lateral pterygoid inserts into the anterior part of the disc. It is attached to the temporal bone in the back. Unless the disk is damaged, the upper and lower compartments cannot communicate with one another.
Since the central region of the disc is avascular and innervated, it receives its nourishment from the synovial fluid around it. In contrast, there are both blood vessels and nerves in the posterior ligament and the surrounding capsules. Fibroblasts and white blood cells are among the few cells that are present. In comparison to the outer section, which is thicker but more cushioned, the core portion is likewise thinner but denser in consistency.
The avascular core region of the disc is nourished by the synovial fluid in the synovial cavities. As people age, the disc as a whole thins and may develop new cartilage in the middle, which can cause the joint to move less freely. Except for the surfaces of the articular disc and condylar cartilage, the inner surface of the articular capsule in the TMJ is covered by the synovial membrane.
The first movement of the jaw when the mouth opens is called rotational movement, and it is facilitated by the lower joint compartment made up of the mandible and the articular disc. Translational movement is the secondary gliding motion of the jaw when it is widely expanded, and it is facilitated by the upper joint compartment made up of the temporal bone and the articular disc.
In certain instances of anterior disc displacement, the condyle compresses this region on the articular surface of the temporal bone, causing pain as the jaw moves.
Retrodiscal tissue
The retrodiscal tissue is strongly innervated and vascular, in contrast to the disc itself. Therefore, when there is inflammation or compression in the joint, the methodical tissue frequently plays a significant role in the pain associated with Temporomandibular Disorder (TMD).
Articulating Surfaces
The articular tubercle (from the squamous portion of the temporal bone), the mandibular fossa, and the mandibular head are the three surfaces that make up the temporomandibular joint.
An articular disk keeps the bones’ articular surfaces apart, preventing them from ever coming into contact with one another. This joint has a special mechanism. When such a disk is present, the joint is divided into two synovial joint chambers, each of which is bordered by a synovial membrane. Fibrocartilage, rather than hyaline cartilage, covers the articular surface of the bones.
Ligaments
Three ligaments—two minor and one major—are connected to the temporomandibular joints. These ligaments are crucial because they define the mandible’s boundary movements or the furthest ranges of motion. Normal function rarely permits mandibular movements beyond the functional limits permitted by the muscle attachments since doing so will cause unpleasant stimuli.
Numerous proprioceptive afferents are sent by several ligaments that control the TMJ forces. Several components, including the capsule, masticatory muscles, skin receptors, and receptors within the periodontal ligaments, contribute to the joint’s proprioception. The way the TMJ functions is significantly influenced by the tension that the articular ligaments feel.
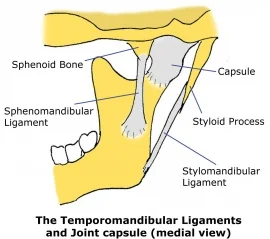
Sphenomandibular ligament
The Meckel cartilage remnant is the sphenomandibular ligament (SML). On its way to the jaw, it inserts itself into the medial wall of the TMJ joint capsule after emerging from the sphenoid spine, which is also the source of the pterygospinous ligament. It affects the malleus and forms some fibers of the malleus’ anterior ligament through the petrotympanic fissure.
It descends farther to affix itself to the mandibular lingula (jaw, middle ear, and sphenoid). The pterygomandibular fascia is in contact with the mylohyoid nerve and some vessels that traverse the ligament. The inferior alveolar nerve, the medial meningeal artery, the internal maxillary artery, the auriculotemporal nerve, and the lateral pterygoid muscle are all in superior and lateral relationships with it. After 10 degrees of mouth opening, its primary function is to shield the TMJ from an excessive translation of the condyle.
Stylomandibular ligament
From the styloid process of the temporal bone to the posterior edge of the jaw or the jaw angle, the stylomandibular ligament (STML) develops. The deep cervical fascia, specifically the parotid fascia, is thought to have thickened. It helps to prevent the jaw from protruding too much. The middle ear stapes will develop from the first and second branchial arches, which are their embryological ancestors (via the Reichert cartilage). It crosses the inner part of the medial pterygoid muscle on its way.
Pterygomandibular ligament
The thickening of the buccopharyngeal fascia is known as the pterygomandibular ligament or raphe (PTML). It extends to the rear region of the mandibular bone’s retromolar trigone from the apex of the hamulus of the internal pterygoid plane of the skull. The buccinator muscle (anterior) and the pharyngeal constrictor muscle (posterior) are two muscles that come into contact with PTML. The ligament is derived from the mesenchymal attachment of the first and second branchial arches in embryology. PTML restricts overly forceful jaw motions.
Pinto or malleolomandibular or discomalleolar ligament
From the perspective of embryology, it originates in the tympanic region. There are two parts to the ligament. The extra-tympanic area, or the posterosuperior portion of the TMJ joint capsule in contact with the retro-discal tissues (passing through the petro-tympanic fissure), is the subject of the second. The first one discussed the middle ear and the malleus concerning the anterior ligament of the malleus. There are two purposes for it. The synovial membrane is shielded from the stresses of the surrounding structures by the TMJ. It would appear that it controls or influences the proper pressure for the middle ear.
The collateral ligament is made up of two symmetrical fiber bundles that insert at the medial and lateral poles of the mandibular condyle after starting at the level of the articular disk’s intermediate fascia. The disk is anchored to the condyle by it.
Nerve supply
The mandibular (CN V), face (CN VII), and C1, C2, and C3 muscles innervate the muscles that act on the TMJ.
As branches of the mandibular nerve (CN V3), which is itself a branch of the trigeminal nerve (CN V), the auriculotemporal and masseteric nerves supply sensory innervation to the temporomandibular joint. Free nerve terminals innervate the TMJ’s muscles, ligaments, and bones; many of these endings function as nociceptors. It is necessary to clarify that the fibrocartilage covering the TMJ condyle is not innervated.
Blood supply
Branches of the external carotid artery, primarily the superficial temporal branch, furnish its arterial blood flow. The arterial blood flow of the joint may also be influenced by other branches of the external carotid artery, including the maxillary, ascending pharyngeal, anterior tympanic, and deep auricular arteries.
In healthy individuals, there is no blood flow to the fibrocartilage covering the TMJ condyle.
Neurovascular supply
The external carotid branches—primarily the superficial temporal branch—provide the arterial feed to the TMJ. The maxillary, ascending pharyngeal, and deep auricular arteries are additional branches that contribute.
The auriculotemporal and masseteric branches of the mandibular nerve (CN V3) innervate the TMJ.
Development
The development of the articular disc and joint spaces at roughly 12 weeks in utero results in the formation of the temporomandibular joints. At around 10 weeks, the mesenchyme between the growing temporal bone and the mandibular condylar cartilage shows the component of the fetus’s future joint. In this area, two slits resembling joint cavities and an intermediate disk appear by 12 weeks. The fibrous capsule of the joint is formed by the mesenchyme surrounding it. The role of newly developing muscles in joint development is mostly unknown. The front part of the fetal disk is where the lateral pterygoid muscle’s growing superior head attaches. The disk also connects to the middle ear’s malleus after continuing posteriorly through the petrotympanic fissure.
The head of each mandibular condyle contains a growth center before the individual reaches adulthood. This growth center is made up of hyaline cartilage on the condyle’s articulating surface, beneath the periosteum. As the body’s final bone growth center, it can grow in multiple directions, unlike a normal long bone. As the individual reaches adulthood, appositional growth causes this portion of the bone’s cartilage to lengthen.
Through endochondral ossification, the bone gradually replaces the cartilage. This mandibular growth center in the condyle enables the mandible to grow longer, which is necessary for the larger permanent teeth and the adult’s larger brain. This mandibular growth is tracked and referred to throughout orthodontic therapy because it also affects the face’s overall form. The condyle’s growth center for bone has vanished by the time an individual achieves full adulthood.
Function
The right and left joints work in tandem and are dependent upon each other since the TMJ is attached to the mandible.
The discomandibular space rotates and the translational discotemporal space acts simultaneously when the mouth opens; the rotation happens before the translation. Lateral movement of the condyle can occur through rotation, anterior sliding of the same condylar structure, and anterior translation/rotation of the opposing condyle in the medial direction. While the opposing condyle slides forward, the condyle can travel backward. The anterior sliding causes the bilateral or ipsilateral TMJ protrusion.
The TMJ’s intricate motions enable several purposes:
- Chewing
- Sucking
- Swallowing
- Phonation
- Facial expressions
- Breathing
- Protrusion, retrusion, lateralization of the jaw
- Opening the mouth
- Preserve the proper middle ear pressure
Movements
The hyoid muscles and masticatory muscles are responsible for movements at this joint. Different roles are played by the temporomandibular joint’s two divisions.
Protrusion and Retraction
The mandible can protrude and retract, or move anteriorly and posteriorly, thanks to the upper portion of the joint.
The protrusion is accomplished by the lateral pterygoid muscle (with assistance from the medial pterygoid), while retraction is accomplished by the posterior fibers of the temporalis. The mandible alternately extends and retracts on each side to provide a lateral movement (i.e., for chewing and grinding).
Elevation and Depression
The mandible can be raised and lowered, opening and closing the mouth, thanks to the lower portion of the joint. Gravity is the main cause of depression. The mylohyoid, geniohyoid, and digastric muscles help, though if there is resistance. The contraction of the temporalis, masseter, and medial pterygoid muscles results in elevation, which is a very powerful movement.
Jaw movement
From the edge of the lower front teeth to the edge of the upper front teeth, the normal whole jaw openness is 40–50 millimeters. The vertical range of motion must be evaluated with consideration for the overbite. If the overbite is 3 millimeters and the distance between the edges of the upper and lower front teeth is 40 millimeters, for instance, the jaw openness is 43 millimeters.
Only the mandible moves when the jaw moves.
Excursions are normal mandibular movements that occur during activity, such as chewing or mastication. The forward excursion, called protrusion, is one of two lateral excursions (left and right). Retrusion is the opposite of protrusion.
A transient underbite is created when the jaw is shifted into protrusion, causing the mandibular incisors, or front teeth, to transcend the maxillary (upper) incisors after first coming edge to edge with them. To do this, the condyle in the upper part of the joint is translated down the articular eminence, whereas, in the lower part of the joint, just a small amount of rotation occurs. In addition to what is required to prevent the mandibular incisors from colliding with the maxillary incisors.
The two temporomandibular joints define the precise movement of the mandible during chewing. While the opposing side of the mandible is known as the balancing or circling side, the side that travels laterally is called the working or rotating side. The latter terminology is more accurate because it defines the sides based on the movements of the corresponding condyles while being a little out of date.
When the jaw is moved into a lateral excursion, the balancing side condyle does the translation, and the working side condyle, which is the condyle on the side of the mandible that extends outwardly, only does rotation (in the horizontal plane). In real functional chewing, rotation (in a vertical plane) also plays a role in both condyles, as the teeth are moved not just side to side but also up and down when biting is included.
The four masticatory muscles—the masseter, medial pterygoid, lateral pterygoid, and temporalis—are largely responsible for moving the jaw. These four muscles, which are all innervated by V3, the trigeminal nerve’s mandibular division, cooperate in various groups to move the mandible in various directions. With the help of gravity, the lateral pterygoid muscle contracts to move the disc and condyle forward within the glenoid fossa and down the articular eminence. This motion causes the jaw to protrude, and the digastricus muscle also opens the jaw. Three other muscles shut the mouth: the temporalis pulls up on the mandibular coronoid process, and the masseter and medial pterygoid pull up the mandibular angle.
Clinical significance
Pain
There are four main causes of temporomandibular joint pain.
- Myofascial pain dysfunction syndrome, which mostly affects the masticatory muscles. This is the most frequent reason.
- An irregular connection between the disc and any other joint component is known as an internal derangement. Internal derangement includes, for instance, disc displacement.
- A degenerative joint condition affecting the articular surfaces is osteoarthritis of the temporomandibular joint.
- Temporal arteritis, for which it is regarded as an accurate diagnostic standard
Temporomandibular joint dysfunction, often known as temporomandibular joint disorder (TMD), is the term used to describe pain or joint dysfunction. This phrase describes a collection of concerns about the temporomandibular joints as well as the blood vessels, ligaments, muscles, tendons, and other tissues that are connected to them.
Other pathologic disorders, though uncommon, can also impair temporomandibular joint function, resulting in pain and swelling. Chondrosarcoma, osteosarcoma, giant cell tumors, and aneurysmal bone cysts are among these disorders.
Disc displacement
Disc displacement is the most prevalent condition affecting temporomandibular joints. This occurs when the articular disc, which is connected to the superior head of the lateral pterygoid muscle anteriorly and the methodical tissue posteriorly, extends from the space between the condyle and the fossa, causing the mandible and temporal bone to make contact with something other than the articular disc. This is typically extremely painful, as previously mentioned, because the center part of the disc lacks sensory innervation, in contrast to these surrounding tissues.
The disc is typically displaced anteriorly following translation, or the condyle slides anteriorly and inferiorly forward within the fossa and along the articular eminence, in the majority of disorders. The condyle returns to the disk when the joint opens, causing a “pop” or “click” that is typically felt as well as occasionally heard. “Reducing the joint” refers to this procedure (disc displacement with reduction). Another “click” or “pop” will occur when the condyle slides off the rear of the disc upon closing, indicating that it is posterior to the disc. The bilaminar region, as well as the nerves, arteries, and veins, are compressed against the temporal fossa by the condyle as it clenches, resulting in discomfort and irritation.
When opening in disc displacement without reduction, the disc remains in front of the condylar head. There is a restricted amount of mouth opening and no “pop” or “click” sound when opening.
Congenital disorders
- Aplasia of the cranium or mandible
- Hypoplasia of the cranium or mandible
- Hyperplasia of the cranium or mandible
- Dysplasia and aberrant tissue growth
Traumatic disorders
- Mandibular dislocation
- Fracture
- Subluxation
Inflammatory disorders
- Synovitis
- Capsulitis
- Myositis
Degenerative disorders
- Osteoarthritis
- Rheumatoid arthritis
- Juvenile idiopathic arthritis
Idiopathic disorders
- Temporomandibular disorder (TMD, sometimes known as “temporomandibular joint pain-dysfunction syndrome”) is characterized by pain and dysfunction in the masticatory muscles (the muscles that move the jaw) and the TMJ. Due to its poorly known pathophysiology and heterogeneous origin, TMD does not easily fall into any one etiologic group. After dental pain (i.e., toothache), TMD is the second most common source of orofacial discomfort and is responsible for most TMJ pathology.
- Fibromyalgia
FAQs
Which joints are temporomandibular?
Your lower jaw is joined to your skull by two joints called the temporomandibular joints (TMJ). They are, more specifically, the joints that slide and rotate in front of each ear and are composed of the mandible (the lower jaw) and temporal bone (the side and base of the skull).
How terrible is the temporomandibular joint?
Individual differences exist in the consequences of TMJ dysfunction. For some, it’s a short-term problem that disappears within a week or two. Others have a chronic illness that lowers their quality of life. Inform your healthcare physician of any regular headaches, facial pain, jaw pain, or other TMJ symptoms.
Do I need to be concerned about TMD?
Failure of jaw bone mass and cartilage: Temporomandibular disorder, or TMD, can cause irreversible damage to the jaw if treatment is not received. Both the jawbone and the cartilage supporting the joint or junction may degenerate. In addition to increasing the risk of jaw dislocation, this produces painful friction in the jaw.
Is TMJ’s condition a concern?
After being diagnosed with temporomandibular joint dysfunction (TMD), many people in Nashville, Tennessee, wonder if the condition is serious. The reason for this is that, although the condition is not life-threatening, it can significantly harm your dental health and general fitness.
What does TMJ mean?
When you chew, yawn, or talk, your jaw discomfort may get worse. It might be dull, acute, or persistent.TMJ disorders can sometimes make it difficult to open the mouth completely, which can make speaking or eating challenging. It can also cause excruciating earaches and tension headaches.
Can someone cure TMJ?
The difficulty of treating joint issues is one factor. Additionally, we don’t fully comprehend the condition, which is part of the problem. However, there is also some positive news. Although there isn’t a cure for TMJ, many people can live pain-free lives after finding relief from their symptoms.
References
- TeachMeAnatomy. (2023b, January 19). The temporomandibular joint – Structure – Function – TeachMeAnatomy. https://teachmeanatomy.info/head/joints/temporomandibular/
- Wikipedia contributors. (2024b, August 5). Temporomandibular joint. Wikipedia. https://en.wikipedia.org/wiki/Temporomandibular_joint
- Bordoni, B., & Varacallo, M. A. (2023, July 17). Anatomy, head and neck, temporomandibular joint. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538486/