Trendelenburg Gait
Introduction
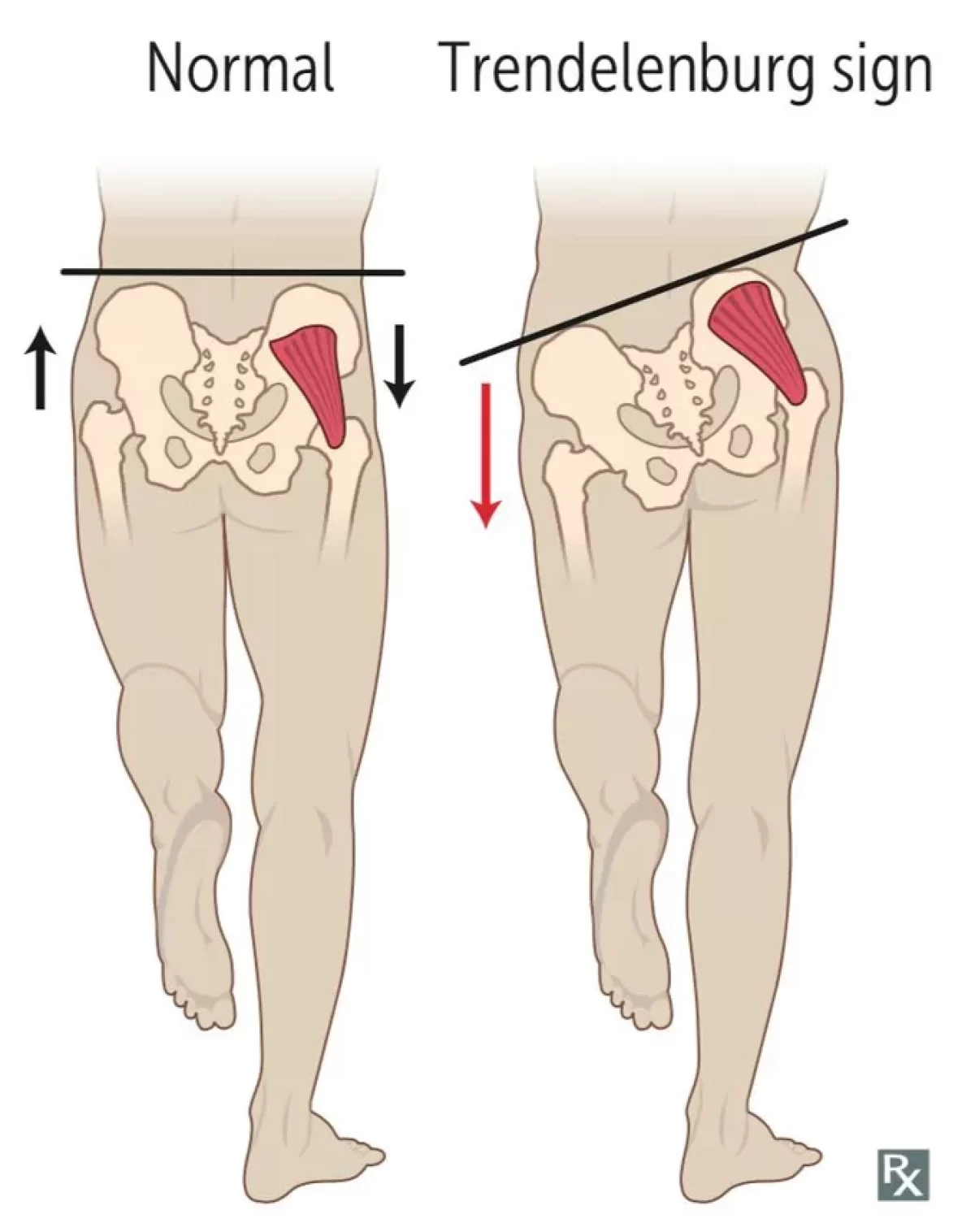
Trendelenburg gait is an abnormal walk caused by a ruptured hip abductor system. Being made up of the gluteus medius and gluteus minimus, the gluteal muscular group is the main muscle group that is impacted.
Walking causes the pelvis to descend to the opposite side due to muscle weakness. This course focuses on Trendenlenburg gait evaluation and management, emphasizing the role of interprofessional team members in providing well-coordinated care and improving patient outcomes.
What is Trendelenburg Gait?
- Trendelenburg gait happens whenever the hip abductors, specifically the gluteal muscles, are weak individually. A lesion in the fifth lumbar spine or injury to the superior gluteal nerve could be the source of this disability.
- Weight-bearing is challenging on the side impacted by this condition. While doing the stance phase of a normal gait, both lower limbs carry half of the body weight.
- During the swing phase, when one lower limb is elevated, the other carries the entire load. The pelvis lowers the weight-bearing leg and raises the non-weight-bearing extremity during the stance phase while walking.
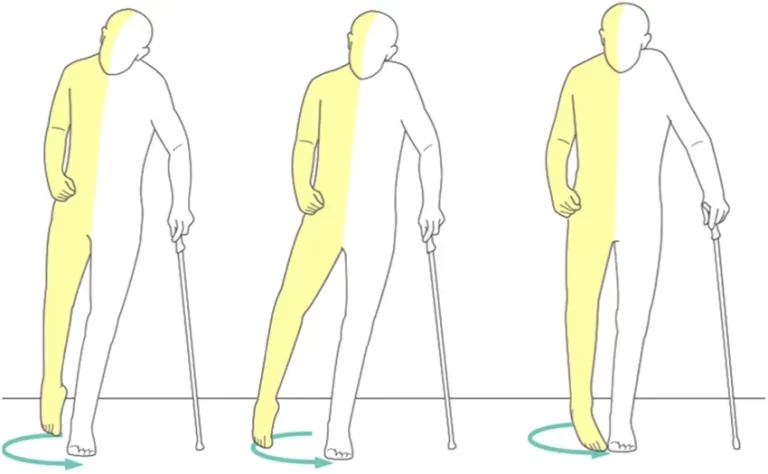
- In contrast, a weak hip abductor leads the non-weight-bearing extremity to lean downward rather than upward. To offset this effect, the person tries to tilt their trunk laterally outward from the injured hip. A lower pelvic drop results from the person’s center of gravity existing mainly on the stance limb.
Relevant Anatomy
- The hip joint‘s acetabulum and femoral head make up its bone composition. These structures are surrounded by 22 muscles and soft tissues. These muscles give the femur the force and stability it needs to move during activity.
- The gluteus medius and gluteus minimus, the two main hip abductors, sustain the pelvis’ opposition and keep it from falling. The superior gluteal nerve originates in the nerve roots L4-S1 and this nerve exits the pelvis through the sciatic notch, supplying the tensor fascia lata, gluteus medius and minimus muscles, and hip joint.
What are the causes of the Trendelenburg Gait?
This gait is frequently the result of your hip abductor muscles being strained when exercising. Gluteal strengthening exercises are frequently the cause. In this instance, the gait will probably diminish as the inflammation in the muscles subsides.
Furthermore, this gait may appear after total hip replacement surgery. Your surgeon will need to create cuts in the gluteus medius muscle during this treatment. You may get this gait as a result of the muscle becoming weakened.
Other causes are :
- Nerve injury or malfunction, particularly in the nerves that supply your gluteal medius and minimus muscles
- Poliomyelitis, a disease linked to the polio virus that affects your muscles, and osteoarthritis, a form of arthritis that develops when joint cartilage begins to deteriorate
- Cleidocranial dysostosis, a congenital defect that can lead to abnormal bone development, and muscular dystrophy, a condition that gradually weakens your bones and muscles
What are the symptoms of the Trendelenburg Gait?
- Swing and stance are the two stages of your gait as you walk. The second leg remains motionless and maintains your balance while one leg swings forward (swing).
- Trendelenburg gait is characterized by one leg swinging forward as the hip goes down and travels outward. This occurs as a result of the opposite leg’s hip abductor being unable to sustain your weight.
- To keep your balance when walking, you could lean slightly to the side or back. As your pelvis changes unevenly, you can raise your foot higher off the ground with each stride to prevent tripping over your feet or losing your balance.
What is the diagnosis of Trendelenburg gait?
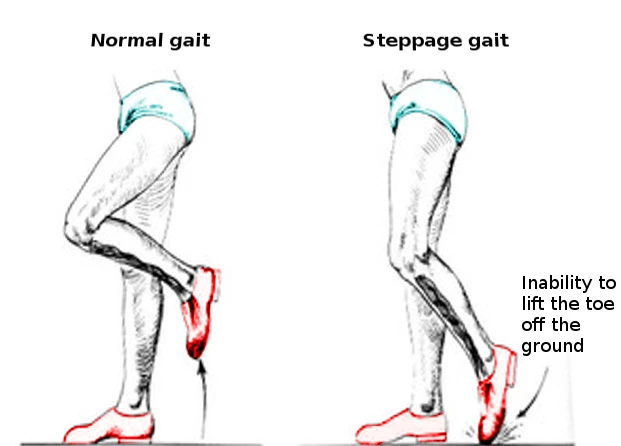
An examination and evaluation of your medical history are necessary to accurately diagnose Trendelenburg’s gait and rule out other gait abnormalities caused by weak hip muscles. These might include the following:
- An unpleasant way of walking
- High-stepping position
- Lenk-extension gait
- Stomping step
The Trendelenburg test may also be used by your physician to make this diagnosis.
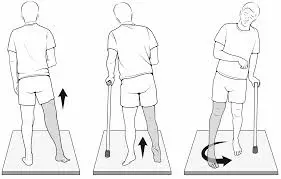
Trendelenburg’s sign
A clinical test called Trendelenburg’s sign is used to evaluate the strength of the gluteus medius, a crucial hip muscle. It’s especially useful for detecting weakness or dysfunction in this muscle, which frequently results in issues like back or hip pain.
How to perform?
- As they stand, the examiner faces away from the patient.
- One leg must be raised off the floor by the patient.
- The examiner glances at the pelvis behind him.
What does a positive Trendelenburg’s sign mean?
When the leg is elevated, it is seen as a good Trendelenburg sign if the pelvis tilts or sinks to the opposite side. The gluteus medius muscle on the side of the raised leg is impacted, according to a positive Trendelenburg sign.
To determine the reasons behind your gluteus medius or minimus weakness, your doctor might also perform hip X-rays.
What is the treatment for the Trendelenburg gait?
The underlying causes of a compensated Trendelenburg gait in patients can be attempted to be addressed by medical treatment.
- An over-the-counter nonsteroidal anti-inflammatory medicine (NSAID), like ibuprofen (Advil) or acetaminophen (Tylenol), can assist in relieving pain associated with your gait. Your doctor might recommend cortisone injections to help with pain management in extreme situations.
- Without the requirement for preoperative traction, open reduction and salter innominate osteotomy (SIO) are successful treatments for hip developmental dysplasia in children under six.
- Patients with untreated congenital dislocations benefit considerably from pelvic support osteotomies in terms of posture, gait, and walking tolerance.
- Osteopathic manipulative treatment (OMT) may help people with somatic dysfunctions improve their gait characteristics by using a GaitMat II system.
- Wearing a lift in one or both of your shoes can also help your doctor adjust for the weakness in your hip abductor muscles. As a result, the distance from the ground would be declined.
Physical Therapy for the Trendelenburg gait
- Trendelenburg gait can cause various hip and knee bone disorders, for example, arthritis and premature hip joint damage. As a result, it is vital to find a type of physical therapy that can diminish Trendelenburg’s gait and lower the risk of further injuries.
- Weak hip abductors cause an unstable gait known as the Trendelenburg gait. The primary goal of physical therapy for Trendelenburg gait is to strengthen the hip joint muscles.
- The best technique to strengthen the hip abductors is for the patient to rest on their side and abduct their upper leg toward the ceiling’s edge. To make the workout more difficult, you can wrap a weight or theraband around the active limb. Exercise can be advanced concerning the force of gravity, weight, and frequency.
- It is also crucial to strengthen the remaining hip muscles on the side that is impacted.
Exercises for the Trendelenburg gait
- When completing these exercises to improve your Trendelenburg gait, always remember to be cautious.
- Additionally, you’re probably adjusting because you’ve been walking in this manner for a while. If you experience any kind of pain, you should slow down and stop.
- Consult your physician before starting an exercise program if you have chronic pain or have just undergone total hip replacement surgery. This will help to prevent subsequent problems.
Exercises
Hip Flexion

- Although you are resting on your rear end, fully extend your legs in front of you.
- Your hands should remain at your sides, palms facing downward.
- Drop your leg back down. Change legs.
- Instead of keeping the leg bent all the time, try straightening it. Rather than putting your hands around the front of your knee, you will reach behind it.
- Perform this exercise ten times each leg, three times throughout the week.
Hip Adduction

- Secure a resistance band around a solid object, such as the leg of a couch.
- Insert your other leg through the resistance band’s opposite side. You and the band don’t need to be at odds here.
- Your free leg should be shoulder-width apart.
- The resistance band-wrapped leg should be pulled until it meets the ankle of the free leg.
- Take a step back.
- After ten repetitions, switch legs. All you have to do is stand backward to switch legs.
- It could be simpler to wrap the band over the knees.
- This exercise should be done three times throughout the week, or for ten repetitions per leg.
Hip Abduction

- Make sure your feet are almost shoulder-width apart as you stand.
- Cover both sides of your ankles with an elastic band.
- Lift one leg and extend it as far away from your body as you are able.
- Put your legs shoulder-width apart again.
- Change legs.
- Avoid using a resistance band if your leg becomes immobile. Just extend your leg as far away from your body as you are able to. If you need balance, use a chair.
- This stretch should be executed five times for each leg three times a week.
Leg Lift

- Take a lying position on your left.
- Maintain a straight line between your right and left sides.
- Place your right elbow on the floor and lower your arm in front of you.
- To help you stay steady, place your left hand beneath your head.
- Raise your right leg to where it feels tight in your thigh.
- Drop your leg. Do this lift ten times, and change your legs.
- Use a chair if hip dysplasia makes this too painful. Stand on the chair’s side, holding onto it with your hand for balance, and raise your left side ten times on each side, three times a week.
Side Plank
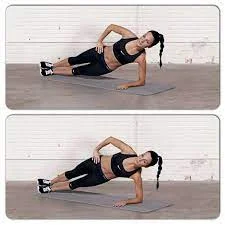
- First, rest on your left side on a mat.
- Place your right leg over your left.
- Raise your body gradually into a straight line. To perform this lift, you will place your weight on the outside of your left foot and your left forearm.
- To assist you stay steady, place your right hand on your right hip.
- Hold for 30 seconds.
- Change sides and do it again.
- Try to maintain the position for as long as you can if you are unable to do so for 30 seconds.
- Three times a week, complete three sets of 30 seconds each.
Squats
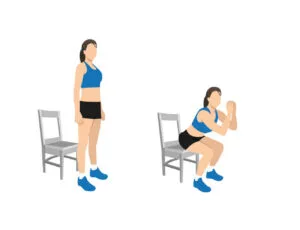
- Take a chair and sit up straight. Cross your arms and stand erect.
- Preserve your back muscles tense and your hips outstretched.
- Drop until your glutes make contact with the chair.
- Make sure your back is straight as you carefully stand back up.
- If you are unable to descend to the chair, try to go as far as you can.
- To make it more challenging try a one-leg squat. Raise your right leg and maintain it there while standing erect. Switch legs after three sets.
- Three times a week, perform three sets.
Single Leg Step
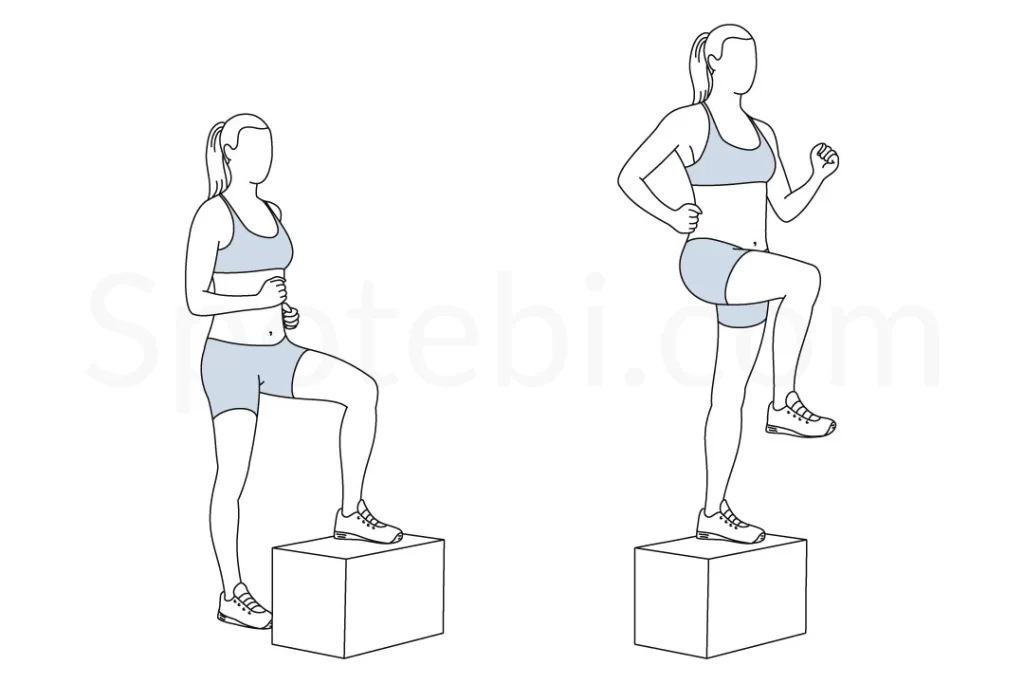
- Standing upright, rest your hands on your hips.
- Immediately behind you, tap one leg.
- The leg in front of you should be tapped with the same leg.
- Continue tapping for thirty seconds. Change your feet.
- For 30 seconds, you should be able to maintain this position on each foot. You should completely avoid doing this workout if you are not going to do it.
- Spend 30 seconds on each foot, every day.
Bridging

- Facing up while lying down.
- Your knees should be bent.
- Compress your heels into the mat while keeping your arms flat on the floor.
- Raise your glutes and torso till your body forms a bridge with the floor.
- Bring your hips down to the ground.
- If this puts too much strain on your back, start from a higher position by placing a box or step beneath your feet.
- Try to finish three sets on average three times a week.
Monster Walk

- Encircle both sides of your ankles with an elastic band.
- To ensure that the resistance band has tension, place your feet slightly wider than hip-width apart while standing.
- To maintain tension on the resistance band, take a step forward that is slightly diagonal.
- Step forward with the other leg while keeping the elastic strap stretched.
- Keep moving ahead by ten steps and backward by ten. It looks like you are walking like a “monster.”
- If this is too challenging for your level of coordination, skip traveling backward; alternatively, place the band above your knees, since this may be simpler. Finish three sets every three days.
Butterfly Strech
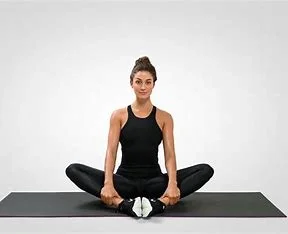
- Sit with your legs bent on the ground next to you.
- Press your foot soles together until they make contact.
- You need to keep your heels near to your body.
- With your arms outstretched, descend your knees to the flooring.
- For 30 seconds, maintain this position.
- If this hurts your inner thighs, extend your heels further.
- Three times a week, perform this stance five times.
Hip Flexor Stretching

- With your right leg bowed and your right foot flat in front of you, make a lunge. Lower your left knee to the surface while keeping your hips upright.
- Your hands should be on your hips.
- Lean your pelvis and body forward slightly.
- Reposition your torso and pelvis gently.
- Continue this back-and-forth motion for 20 repetitions.
- Perform this exercise three times a week for twenty repetitions.
Standing kick
- Place your hips shoulder-length apart and face ahead.
- As if you were prepared for battle, place your hands in a boxer stance.
- Throughout the count of three, raise your right leg out to the side, getting higher each time.
- Return your leg to the floor. Change legs.
- The leg should be raised straight in front of you rather than sideways.
- Practice this exercise 15 times on each leg three times during the week.
- Even though this may seem like a lot of exercises, doing them three times a week can help you develop a normal gait and strengthen your hip abductor muscles. This can help you return to walking and running pain-free and minimize future costly health problems.
Summary
Despite its annoying appearance, Trendelenburg gait may typically be treated with appropriate shoes or exercises that strengthen your hip abductor muscles. If your gait is caused by an underlying condition, such as muscular dystrophy or osteoarthritis, your doctor will collaborate with you to establish an appropriate treatment plan.
The condition’s effects on your health and walking abilities can be lessened with medication and physical treatment. Treatment can help you walk more smoothly and lower your risk of problems, even if Trendelenburg’s gait may not always be completely correctable.
FAQs
What is the Trendelenburg gait?
An irregular gait caused by a malfunctioning hip abductor mechanism is known as Trendelenburg gait. The gluteal musculature is the main muscle group that is engaged. Muscles of the gluteus, such as the medius and minimus.
What does a positive Trendelenburg sign mean?
When evaluating for hip dysfunction, a physical examination observation described as the Trendelenburg sign is observed. Weakness in the hip abductor muscles, which include the gluteus medius and gluteus minimus, is typically indicated by a positive Trendelenburg sign.
The Trendelenburg sign involves which nerve?
Unilateral weakness in the hip abductors, mainly affecting the gluteal musculature, is the cause of the Trendelenburg gait. A lesion in the fifth lumbar spine or injury to the superior gluteal nerve could be the cause of this disability.
References
- Kelly, E. (2023, March 17). 8 of the Best Hip Flexor Stretches and Exercises. Healthline. https://www.healthline.com/health/fitness-exercise/hip-flexor-exercises#stretches
- Patel, D. (2023, December 13). Trendelenburg Gait – Causes, Treatment, Exercise – Mobile Physio. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/trendelenburg-gait/
- Prajapati, N. (2023, March 17). Trendelenburg Gait – Symptoms, Treatment, Exercise – Samarpan. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/trendelenburg-gait/
- Trendelenburg Gait. (n.d.). https://www.physiotherapy-treatment.com/trendelenburg-gait.html