Piriformis Syndrome
What’s piriformis syndrome?
In piriformis syndrome, the sciatic nerve presses against the piriformis muscle, resulting in back and buttock pain and numbness. The primary symptoms of the illness are pain in the buttocks and pain that travels down the lower limb. Other symptoms include weakness, numbness, and issues with the bladder and bowel.
A little muscle that extends deep into the buttock region and joins to the hip is called the piriformis. This muscle directly borders the sciatic nerve, which can entrap it and cause Piriformis Syndrome. This is a disorder that causes pain to travel down the leg from the hip. Walking, sitting, and other everyday tasks may become difficult due to the severe pain.
When standing on one leg, this muscle aids in maintaining balance and in turning your leg outward. The piriformis muscle can become tight or spastic following an injury, which is typically the cause of piriformis syndrome. A disorder known as diastasis symphysis pubis, or the separation of the pelvic bones, may be the cause in certain instances.
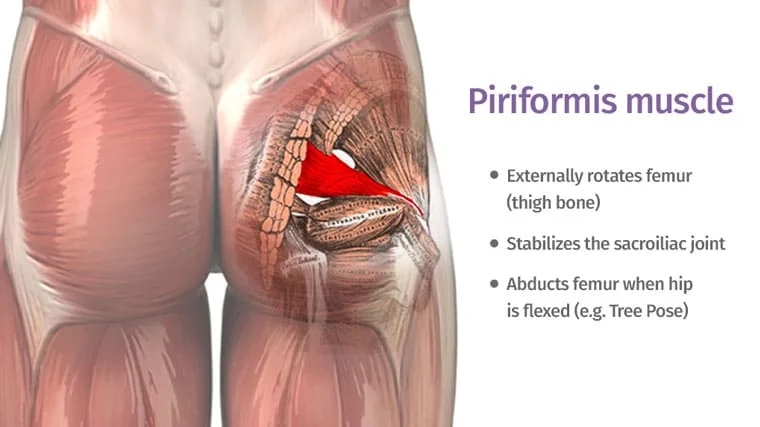
Piriformis Muscle Anatomy:
The muscle, which is triangular in shape, originates from the anterior surface of the hip joint capsule as well as the posterior surfaces of the sacrum and coccyx. The femur’s greater trochanter receives its insertion. The hips are externally rotated, abducted, and partially extended by the Piriformis muscle.
Pathology:
- One of the following conditions might produce secondary piriformis syndrome: microtrauma, microtrauma, ischemic mass effect, or local ischemia.
- Most frequently, microtrauma to the buttocks results in soft tissue inflammation, muscular spasm, or both, and ultimately nerve compression, which causes piriformis syndrome.
Piriformis syndrome causes:
The following conditions may produce piriformis syndrome in one or more cases:
- damage to the hips and buttocks region.
- spasm in the piriformis muscle.
- injuries following surgery, for example. replacement of the hip joint
- Pathologies of the lumbar and sacroiliac joints
- muscular tightness caused by changed lower limb biomechanics
- the piriformis muscle hypertrophy.
- arthritis in the sacroiliac joint
- “Wallette neuritis,” or bursitis of the piriformis muscle, is a result of repeated stress from extended periods of time spent sitting on hard surfaces.
- During weight-bearing activity, the excessive hip movement primarily adducts and internally rotates; as a result, a larger eccentric load may be transferred to the piriformis muscle due to gluteal muscle weakness.
- Following laminectomy surgery, myositis, hematoma, and abscess may occur.
- Klippel-Trénaunay Syndrome.
- intraluminally injection.
- Sciatica: Sciatic nerve neuropathic pain.
Piriformis syndrome symptoms and signs:
Additional related typical signs and symptoms include:
- Numbness that tingles in the back of the hip may spread to the leg.
- Comfortable long-term sitting is difficult
- lower back pain.
- Sciatica is a pain that radiates.
- stiffness in the hip joint.
- walking a long distance can be difficult.
- swelling in the legs and ankles if the situation gets worse.
- There have also been reports of sexual life disturbances.
The pain that radiates down your legs and buttocks can be more acute and even incapacitating in the most extreme circumstances. You can lose the ability to do simple, daily activities including walking, crouching, and prolonged sitting.
Differential Diagnosis:
- Sacroiliac joint inflammation, lesion, and dysfunction
- Inferior gluteal artery pseudoaneurysms after gynecological surgery
- Blood clot in the iliac vein
- intervertebral disc herniation
- Coccygodinia post-laminectomy syndrome
- False positive pelvic fracture
- Osteochondrosis of the back
- Unidentified kidney stones
- Radiculopathies of the lumbar region
- Osteoarthritis of the lumbar spine
- sacroiliac joint syndrome
- Degenerative disc disease Fractures caused by compression
- Hip joint intra-articular pathologies include femurs-acetabular impingement (FAI) and labral tears.
- lumbar Spine stenosis
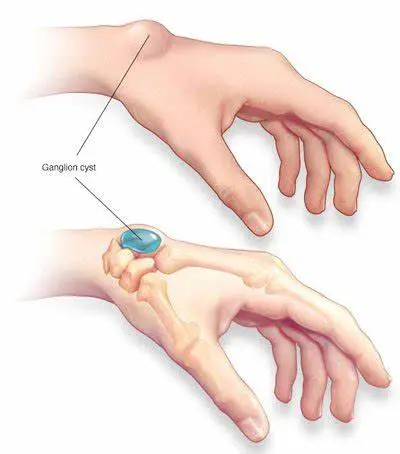
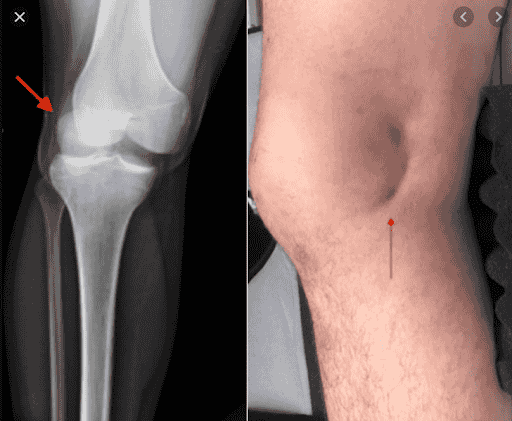
- cysts and tumors
- gynecological disorders
- diseases including pyelitis, hypernephroma, appendicitis, prostate, uterus, and pelvic visceral cancers etc.
- Psychogenic disorders include physical exhaustion, despair, and annoyance.
- sacroiliac disease
Diagnosis:
MRI/CT scans, X-rays, EMG investigations, and physical examinations by physical therapists or doctors are the primary methods used to diagnose Piriformis syndrome.
Investigation:
Studies using radiographic X-rays are not very important for diagnosis.
To rule out the other possibility that the patient’s symptoms are related to the lumbar spine or the hip region, anteroposterior (AP) x-rays of the pelvis and hips, lateral hip views on x-ray, and/or CT scans or MRIs of the lumbar spine are advised.
Electromyography (EMG): Muscles close to the piriformis muscle will exhibit aberrant EMG responses due to compression of the intervertebral nerve root.
When diagnosing piriformis syndrome, physical examinations involving active movements, like the FAIR test, maybe more valuable and specific than other tests currently in use.
Physical Examination:
a physical structural examination, paying particular attention to any disparities in leg length and the lumbar spine, pelvis, and sacrum.
examinations for diagnosis.
Test for piriformis syndrome:
- Palpation:
A careful, deep probing can reveal the presence of a Piriformis muscle spasm.
Deep digital probing of the gluteal and retro-trochanteric regions may reveal pain and tenderness, as well as an aggravation of tightness and numbness in the legs.
- Pace sign:
This exam measures how uncomfortable and weak the hip external rotation and abduction are when sitting.
- Lasèque sign / Straight Leg Raise Test:
The patient experiences radiating pain in the buttocks and leg that gets worse as the examiner raises his or her leg passively.
- FAIR sign:
Stretching the piriformis causes pain in the hip joint’s flexion, adduction, and internal rotation
- Hip Abduction Test:
The patient may be instructed to slowly abduct their leg while the examiner stands in front of them at the level of their feet and watches without touching them.
Hip abduction to 45° is normal.
Along with limb shortening on the affected side, patients with PS may also exhibit gluteal muscular atrophy.
Muscle hypotrophy is observed on the side of the body that is affected in chronic situations.
- Positive Trendelenburg signs are also possible.
Piriformis Syndrome Treatment:
The three major treatments for piriformis syndrome are physical therapy, medicine, which is sometimes referred to as a conservative course of treatment, and surgery as a last resort.
Medical Treatment:
The mainstays of medical treatment for post-stroke syndrome (PS) are non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, neuropathic pain medication, physical therapy, active lifestyle alterations such as avoiding activities that exacerbate pain and other symptoms, and adequate rest.
Applying a hot or ice pack to the back of the leg or hip. To avoid using an ice pack that comes into contact with your skin, cover it with a cotton towel. Next, apply a hot pack for approximately the same duration. To help with the pain and spasms, try doing it every two to three hours. Applying a combination of ice and heat packs to your legs or buttocks may help ease pain.
The limitations of procedures and anatomical variances should be known to the doctors. It has been demonstrated that this method is useful for both the diagnosis and treatment for treating PS.
Surgery may be recommended to relieve the piriformis muscle’s pressure on the sciatic nerve if you are still unable to find relief. However, this is rarely needed.
Physical therapy Treatment:
- Pain-relieving electrotherapy techniques used in physical therapy treatments include ultrasound therapy, TENS/IFT, soft tissue mobilization, stretching and strengthening of the piriformis muscle, and the application of hot or cold packs.
- In addition, the treatment included functional exercise therapy for the hips, which aims to strengthen the hip extensors, abductors, and external rotators in addition to correcting improper movement patterns and posture.
- The patient typically attends 4 to 5 sessions each week for around 6 to 8 weeks in order to get decent outcomes.
- Ultrasound Therapy
- Hot Pack/Cold Pack: Before exercising, applying a hot or cold pack might help minimize pain and muscular spasms.
- The intervention’s main goals were to strengthen the hip extensors, abductors, and external rotators and to address improper movement patterns. It also included functional exercise treatment for the hips.
- The patient typically has 2-3 treatments per week for 2-3 months in order to see a 60–70% improvement.
- The patient must initially be positioned in the FAIR posture (Flexed Adducted Internally Rotated) and in contralateral decubitus.
- Start with a 10-to 14-minute ultrasound treatment at 2.0–2.5 W/cm2.
- To reduce pain, it is highly helpful to apply heat and cold before stretching. Subsequently, commence the piriformis stretching exercise, which can be performed in multiple methods.
- The therapist can also offer several suggestions to prevent the symptoms from getting worse. Included in this is: Keep away from prolonged sitting.
- Every twenty minutes, get up and stroll.
- When driving, stop frequently to stretch and stand up.
- Avoid causing harm to the gluteal area.
- keep away from more offensive actions.
- It is advised to stretch every day to prevent the piriformis syndrome from returning.
- Additionally, the patient can exercise and receive treatment at home by rolling from side to side while flexing and extending their knees while lying on either side.
- Every few hours, spend a minute rotating side to side while standing with your arms relaxed.
- Have a hot bath.
- Lay flat on your back and use your hands to raise your hips while using your legs to pedal like you’re on a bicycle.
A few pointers to prevent the symptoms from getting worse might also be provided by the physical therapist. These are:
- Avoid spending a lot of time sitting down during regular activities.
- Avert abrupt movements towards the gluteal area.
- keep away from anything uncomfortable to do.
- It is advised to perform stretching exercises on a regular basis to prevent the piriformis issue from returning.
Other workouts and therapies that you can perform at home are as follows:
- Regularly take a warm bath.
- Supine Knee bends: lie flat on your back, lift your hips with your hands, and pedal with your legs as though you were riding a bike.
Piriformis syndrome exercises:
- Gluteal stretch:

A slight stretch will be felt in your buttocks and potentially on the outside of your hip on the upper leg. Do this twice or three times.
- Standing hamstring stretch:
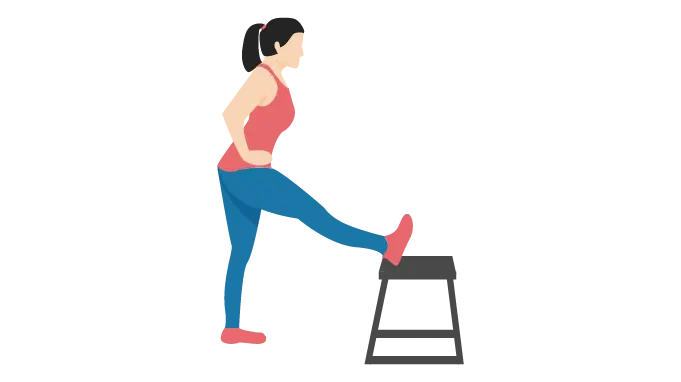
Be cautious about maintaining a straight knee. When performing this exercise, make sure to bend only at the waist and avoid moving your shoulders as this will stretch your lower back rather than your leg. Stretch for eight to ten seconds. Three times, repeat.
- Resisted hip abduction:
in a sideways stance next to a doorway. Wrap an elastic bandage over your affected leg’s ankle, facing away from the entrance. After tying the theraband’s opposite end, shut the knot inside the door. Maintaining a straight knee, abduct your leg to the side.
- Prone hip extension (Knee flex):
- Quadruped arm/leg raise:
Raise one arm and the opposing leg away from you while tensing your back muscles to maintain a straight spine. Slowly Lower your leg and arm gradually, then repeat on the other side.
- Partial curl:

Squeeze the muscles in your abdomen. Put your chin down against your chest. Arrange your hands in front of you and curl your upper body forward until your shoulders are off the ground. Keep your posture for three seconds. Avoid holding your breath. Exhaling while you raise your shoulders aids in this process. Calm down. Ten times, repeat. Up to three sets of ten.
- Stretch IT band supine hip rotation:
Only extend yourself as far as you can. Keep your knee from going all the way to the floor. Maintain a floor-level back and hips.
On your back, bend your knees. Proceed with the opposite leg. Hold the exercise for ten seconds.
- Stretch hip/knee:
On your back, bend your knees. Transfer left ankle to right knee. Proceed with the opposite leg. Hold the exercise for ten seconds.
- Partial sit-up exercise:
incline With your knees bent and your feet flat on the ground, assume a prone position on a comfortable mat. After 2 to 5 seconds of holding this posture, progressively relax. 8–10 times, repeat. Up to three sets of ten. Gripping your hands behind your head and extending your elbows to the side can make things more tough for you.
- Stretch piriformis supine crossed leg:

incline laying on your back on a comfortable surface with your ankle crossed over your opposing leg and your knee bent. Until a little stretch is felt in the affected buttocks area, grab the knee and pull the thigh across while consciously attempting to shift the right knee inside. Remain calm and repeat. Twice a day, perform one set of eight to ten repetitions. For 8–10 seconds, hold the exercise.
- Stretch Piriformis Long sitting:

With the injured knee bent and the ankle on the outside of the left leg, assume a lengthy sitting position. Holding onto the knee, drag the thigh across the chest and toward the other shoulder. Relax little by little. For 8–10 seconds, hold the exercise.
- Resist hip external rotation(ER) stand with elastic:
Secure something at waist level by attaching elastic. As you balance on the involved leg, contact your toes with the uninvolved leg. Take a minute off in between each set. Every 4 seconds, perform one repetition.
- Resist hip with elastic:
Secure something at ankle level by attaching elastic. Replicate from the beginning position. Once every other day, perform three sets of 210 repetitions. Take a minute off in between each set. Every 4 seconds, perform one repetition.
- Resist hip extension stand with elastic:
encircle the ankle with a loop. Faced toward the pull, stand. Take a minute off in between each set. Every 4 seconds, perform one repetition.
- Resist hip abduction sit with elastic:
occupy a chair. Replicate from the beginning position. Take a minute off in between each set. Every 4 seconds, perform one repetition.
Piriformis syndrome surgery:
- It is only appropriate to offer surgical treatment in cases where non-medical treatments have failed and the symptoms are becoming incapacitating.
- Another potential source of sciatica pain to be taken into account is the obturator internus muscle.
- Active range-of-motion (ROM) exercises and crutches for two to three weeks are part of the postoperative care. The surgical procedure mentioned above produced immediate benefits.
Conclusion on Piriformis Syndrome:
The usual approach to treating piriformis syndrome consists of physical therapy, stretching exercises, and, occasionally, medicine or injections to lessen pain and inflammation. Although conservative treatment works well most of the time, persistent cases could need more sophisticated measures like surgery. For better results and less suffering, an all-encompassing treatment strategy and an early diagnosis are essential.
To stop a recurrence, patients are advised to continue their normal exercise regimen, abstain from activities that could make their symptoms worse, and adhere to a customized rehabilitation program.
FAQs
How Can I Tell the Difference Between Piriformis and Sciatica?
It is important to understand that these are two different illnesses, mostly characterized by the type of pain you feel. Therefore, if you only experience pain in your hips and buttocks, you probably have piriformis syndrome. If your legs hurt more and your lower back hurts less, it’s most likely sciatica.
For whom is piriformis syndrome most likely to occur?
Sedentary lifestyle: Piriformis syndrome is more common in those whose employment or manner of life requires them to spend most of their days sitting down.
Is there a cure for piriformis syndrome?
Undoubtedly, piriformis syndrome is entirely curable. For the most part, physical therapy combined with rest is sufficient to reduce pain; but, if it persists, you should consider seeking medical attention. It could be necessary for certain people to take medication, engage in activities, and employ heat or ice therapy in order to totally and completely heal.
What are piriformis’s primary symptoms?
Primary signs of piriformis include:
a chronic ache in the buttocks.
Sciatica pain radiating to the foot, leg, and back of the thigh
Excruciating Stair Climbing or Walking
Long periods of sitting cause more pain.
Hip stiffness (reduced range of motion in the hip joint)
What is the piriformis syndrome’s best course of treatment?
Physical therapy, botulinum toxin injections, steroid injections, and dry needling are available forms of treatment. If conservative treatment is ineffective for piriformis syndrome, there are less intrusive treatments.
Which three factors frequently lead to piriformis syndrome?
Three typical reasons for piriformis syndrome
Inappropriate lifting that damages the piriformis muscle
Not warming up sufficiently before or after an activity session.
Putting forth a lot of effort or doing repetitive activities, such as jogging a long distance. prolonged periods of time spent sitting (like someone who works from a desk all day).
With piriformis syndrome, how should one sleep?
If you have piriformis syndrome, the key to improved sleep is to support your hips and spine. You can achieve this by sleeping on your side or back, using a medium-firm mattress, and placing support pillows beneath or between your knees. Throughout the day, stretching exercises can be helpful as well.
Is the piriformis condition irreversible?
The majority of piriformis syndrome patients recover with treatment and lifestyle modifications. Make sure you follow your doctor’s advice as treating this issue might result in irreversible nerve damage if left untreated.
References
- Dhameliya, N. (2024, July 31). Piriformis Syndrome: Physiotherapy Treatment, Exercise. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/piriformis-syndrome-physiotherapy-treatment-exercise/
- Physiotherapist, N. P. (2023c, December 13). Piriformis Syndrome and Physiotherapy Treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/piriformis-syndrome-physiotherapy-management-and-rehabilitation/




3 Comments