Decerebrate Posture
What is Decerebrate Posture?
Decerebrate posture, also known as decerebrate rigidity or extensor posturing, is a specific type of abnormal body posture that typically indicates severe damage to the brainstem.
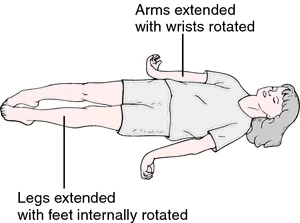
It’s characterized by rigid extension of the arms and legs, with the arms positioned straight out and the legs extended and internally rotated. The posture results from dysfunction or damage to the brainstem, which disrupts the normal balance of neural signals controlling muscle tone and movement.
Decerebrate posture often occurs in response to serious head injuries, strokes, or other traumatic brain injuries that affect the brainstem. It reflects a loss of inhibitory control over the muscles by higher brain centers, leading to exaggerated and uncontrolled muscle contractions. The presence of decerebrate posture is concerning and indicates a significant neurological injury that requires urgent medical attention.
Extensor posturing, decerebrate stiffness, and decerebrate reaction are other names for decerebrate posturing. It explains how the upper extremities extend involuntarily in reaction to outside stimuli. The head is arched back, the arms stretched out to the sides, and the legs are extended in a decerebrate stance.
Decerebrate postures are regarded as abnormal reactions to stimuli that are often unpleasant, whether they originate internally or externally. Both entail conventional trunk and extremity motions and are usually suggestive of serious brain or spinal damage. Charles Sherrington, the Nobel laureate, first documented decerebrate posturing in 1898 following his transection of live monkey and cat brainstems.
The term decerebrate posture is associated with identifiable anatomical regions that may not be as prescriptive as they seem, which has led to criticism of their usage in therapeutic settings in the literature. Both postures can be caused by brain injuries in several anatomical locations, however they generally include some degree of brainstem damage. Nonetheless, it is known that in order to decorticate, an injury must usually be more rostral than in a decerebrate posture. This level is referred to as the red nucleus at the midbrain’s intercollicular level in the majority of books.
Extended elbows are a defining characteristic of the decerebrate stance. The limbs are stretched and internally rotated. The patient’s teeth are tightly closed and they are stiff.
The symptoms may be irregular, limited to the arms, and present on one side or both of the body.
In the motor part of the Glasgow Coma Scale (for adults) and the Pediatric Glasgow Coma Scale (for newborns), a person who exhibits decerebrate posture in response to pain receives a score of two because their muscles are expanding as a result of their neuro-muscular response to the trauma.
Damage to the brain stem below the level of the red nucleus, such as a mid-collicular lesion, is indicated by decerebrate posture. People who have compression or lesions in the cerebellum and midbrain display it. In pontine strokes, decerebrate posture is frequently observed. A patient exhibiting decorticate posture may exhibit decerebrate posturing or alternate between the two posing styles.
The transition from decorticate to decerebrate posture is frequently a sign of tonsilar or uncle (transtentorial) brain herniation. Studies in animals have demonstrated that dorsal root transection removes decerebrate stiffness symptoms, leading to the hypothesis that activation of gamma motor neurons plays a significant role in decerebrate rigidity. Higher inhibitory controls are released from the centers below the site through transaction.
Posturing, usually involving the forearms, can happen during competitive contact sports when there is a head collision. This is known as the fencing reaction. In this instance, the brief posturing display denotes a brief disturbance of brain neurochemicals that goes away in a matter of seconds.
Epidemiology
There is no published data on the prevalence of aberrant posture. On the other hand, the prevalence of diseases that frequently result in decerebrate posture is known. Traumatic brain injury is the most frequent cause of decorticate and decerebrate posture (TBI). According to a 2019 systematic study, 69 million TBIs occur globally every year, of which 7.95% are classified as serious. Patients who have a GCS of 8 or lower are considered to have severe TBI.
Causes of Decerebrate Posture:
In addition to more common diseases like metabolic and infectious reasons, there are many other causes of aberrant postures, such as supratentorial and infratentorial lesions:
Lesions in the supratentorial area
- Abscess
- Subdural and extradural hematomas that are extra-axial.
- Hydrocephalus.
- Tumor.
- Intracerebral hemorrhage.
- elevated intracranial pressure.
- Diffuse Axonal Injury: A Traumatic Brain Injury.
Infratentorial Lesion of Tumor
- Abscess.
- Hydrocephalus.
- Brainstem or bilateral diencephalic infarct.
- Brainstem or cerebellar bleeding within the brain.
- Diffuse Axonal Injury: A Traumatic Brain Injury.
- Tumor.
Diffuse and Metabolic
- Electrolyte abnormalities: hyponatremia, hypomagnesemia, and hypocalcemia
- Cerebral malaria
- Encephalitis
- Encephalopathy of the liver
- Brain damage caused by hypoxia
- Low blood sugar
- poisoned with lead
- Meningitis
- Reye Syndrome
Episodes of decerebrate posturing can happen in individuals who have underlying anatomical lesions of the central nervous system in reaction to a variety of physiological conditions, such as fever, hypoxia, metabolic disruption, meningeal irritation, sensory irritation, and hypoglycemia.
Pathophysiology
Usually, the intercollicular line at the level of the red nucleus is the anatomical division linked to decerebrate posture. Though the brainstem is usually implicated, this idea has been questioned because injuries in the supratentorial area can also produce both decerebrate postures.
Although both posture styles are conventional, they can exist in different proportions and even asymmetrically, with one side decorticate and the other side decerebrate. A posture that is shown inconsistently usually indicates less severe damage.
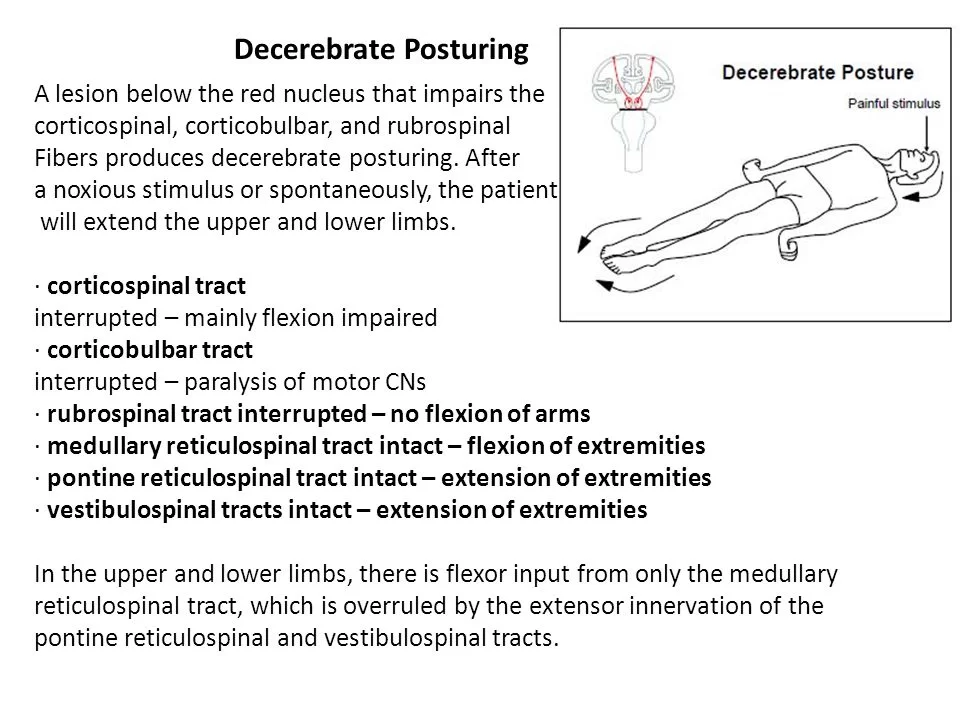
Decerebrate Posturing
In monkeys with a transecting lesion at the level of the superior and inferior colliculi in the midbrain, decerebrate posturing has been shown. It is also stated that this is at or below the red nucleus’s level. Sherrington conducted tests on live animals in which he removed the cerebral cortex from the intercollicular level upwards in sedated monkeys.
The animals developed the conventional extension stiffness of the extremities and continued to breathe on their own. Extensor posturing only happened in the presence of noxious stimuli, passive head hyperextension, or metabolic disturbances such as hypoxia, according to research using intercollicular transection.
Patients with significant bilateral forebrain injuries that proceed caudally into the diencephalon and midbrain may exhibit decerebrate posture. A posterior fossa lesion squeezing the midbrain or rostral pons may potentially be the reason. Even because decerebrate posture suggests a catastrophic structural injury, metabolic disorders that are reversible, including hypoglycemia and hepatic encephalopathy, can also be the cause.
It has been demonstrated that the vestibulospinal tract is crucial for decerebrate posturing in both human and animal models. Flexor motor neurons in the spine are inhibited by vestibulospinal pathways, but extensor motor neurons in the spine are excitatory. The cerebral cortex and the cerebellum’s fastigial nucleus provide modulatory signals to the vestibular nuclei, which also receive input from the vestibular apparatus and spinal somatosensory pathways.
When the vestibular nucleus is isolated, it activates the spinal cord’s extensor motor neurons and inhibits the flexor motor neurons through the vestibulospinal tract. However, this reaction is prevented under normal physiology by the higher brain regions of the cerebellum and cortex, which suppress the vestibular nuclei. Unsuppressed extensor posturing arises from a disconnection between the vestibular nuclei and the modulatory higher regions, which leads to decerebrate posturing.
Differential Diagnosis
Normal flexion might resemble decorticate posture, which is sometimes referred to as withdrawal to pain. On the other hand, aberrant flexion is characterized by sluggish, stereotyped motions, whereas normal flexion moves quickly and variably. Normal flexion is characterized by the wrist being either neutral or extended, the shoulder abducting away from the body, and—most importantly—no lower limb extension. Abnormal flexion causes the wrist to flex with forearm pronation, the shoulder to adduct, and the internal rotation to occur. The lower limbs’ extension is a crucial component.
After brain death, spinal reflexes might still exist. According to one research, 22% of individuals with proven brain death had motor spinal reflexes. These may be confused with aberrant posturing gestures like decerebration.
Extra-pyramidal aberrant posture, or opisthotonus, is observed in cases of cerebral palsy, tetanus, drowning, traumatic brain injury, and poisoning. It’s an odd posture with a slightly arched neck and spine. Additionally resembling aberrant posture, paratonia, also known as gegenhalten, is generally caused by encephalopathy or neurological diseases.
Finally, spasticity can occur in people who have had corticospinal tract traumas, such as hemorrhages, tumors, or ischemic strokes. Similar to decorticate posture, flexor muscles often predominate in the upper limb and extensor muscles in the lower limb. The retention of awareness in spastic individuals is the most notable distinction between aberrant posture and spasticity.
Diagnosis:
History and Physical
In their initial publication on the Glasgow coma scale, Teasdale et al. proposed that in the early stages after brain damage, categorizing the reaction as either flexion or extension may be adequate because it takes an experienced observer to discriminate between normal and pathological flexion.
Adduction and internal rotation of the shoulder, flexion of the fingers, and extension at the elbows with pronation of the forearm are all considered decerebrate posture. Similar to decorticate posing, the lower limbs exhibit plantar flexion of the foot, extension of the knee, and internal rotation at the hip. Usually, toes are hyperextended and abducted. Teasdale and Jennett recommended using the term “extension” instead of “decerebrate” when assessing coma since the phrase is linked to a particular physiognomical correlate.
Evaluation
Rather than being a diagnostic in and of itself, decorticate and decerebrate posture are clinical diagnoses and should be viewed as a pathological indicator of neurological damage. Numerous studies could be necessary because of the range of etiologies that could lead to these results. As previously mentioned, early intracranial imaging, such as CT or MRI, is necessary because compressive lesions may benefit from surgical intervention, which is best done in a timely manner. Laboratory testing, such as serum and CSF collection, can be used to look at additional reasons, such as infection and metabolic disruption.
The diagnosis of decerebrate posture is made using the following technique.
Blood and urine tests to monitor blood levels, screen for drugs and other harmful substances, and measure body chemicals and minerals; CT scan or magnetic resonance imaging (MRI) of the head
Cerebral angiography: an x-ray and dye investigation of the brain’s blood arteries
Brain wave testing, or EEG
monitoring of intracranial pressure (ICP).
Treatment / Management
The goal of treatment is to address the underlying cause, such as curing infections and, where feasible, reversing metabolic abnormalities. Removing an extra-axial hematoma from a TBI can increase survival. Since some diseases, including hypoxic brain damage, may not be curable, supporting measures are used.
Direct treatment is not an option for decreasing posture. Treating the underlying disease that is causing it is the sole choice if that is at all feasible.
Individuals exhibiting decerebrate posture may also be unable to breathe on their own since they are most likely in a coma. It’s also possible that the patient will need supportive care, such as mechanical breathing or other therapies that support bodily systems during a coma.
Treatment strategies differ greatly since decerebrate posture can be caused by so many different illnesses. A medical expert is the ideal person to counsel you on possible remedies.
Physical Therapy Treatment:
Decerebrate posture is treated with physical therapy based on a postural examination, a linked condition’s diagnosis, and symptomatic care.
The objective of treatment with physical therapy:
- Regain control over your movements.
- decrease Spasticity versus rigidity.
- Keep your posture straight or slack.
- Enhance Balance when standing and sitting.
In order to reduce stiffness and spasticity:
To lessen stiffness and spasticity The best course of therapy is stretching exercises. Lower limb stretching exercises, particularly those targeting the hamstring, adductor, and calf muscles, are crucial. Calf muscle stretches and passive stretches that promote good posture are also useful.
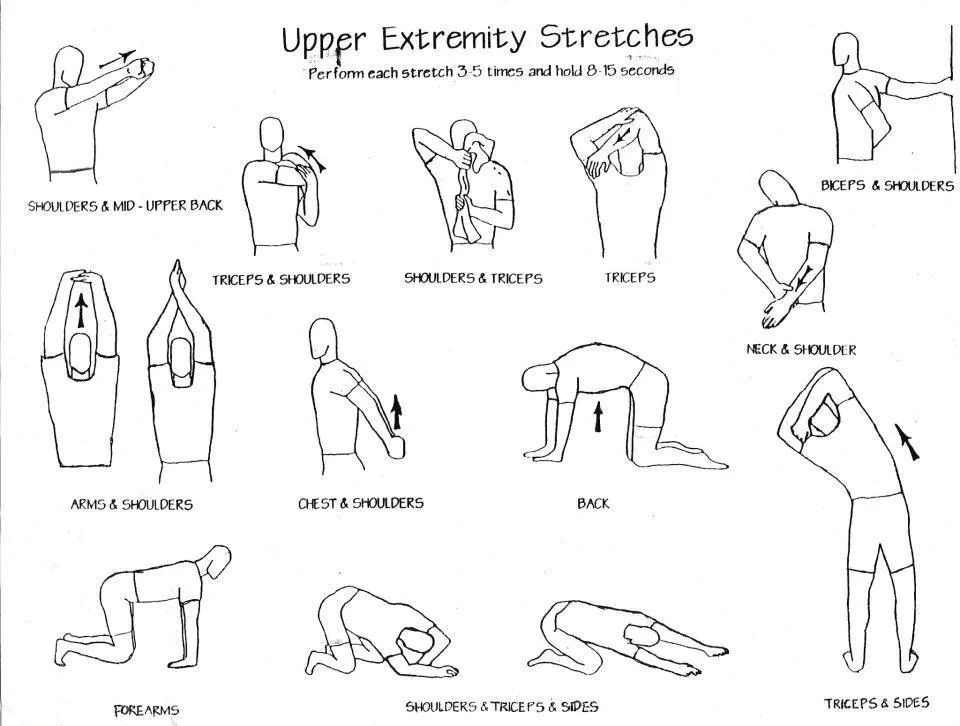
According to the results of the spasticity evaluation, stretching exercises are necessary for the upper limb. It is necessary to keep all joints in their range of motion and to move them passively and comfortably.
According to the assessment, balance exercises are useful in enhancing conditions for both sitting and standing balance.
Stretching exercise in Decerebrate Posture:
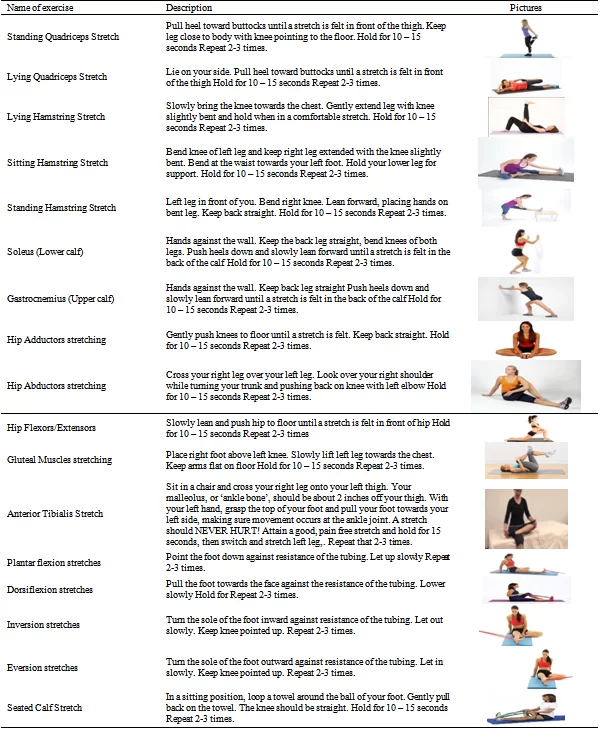
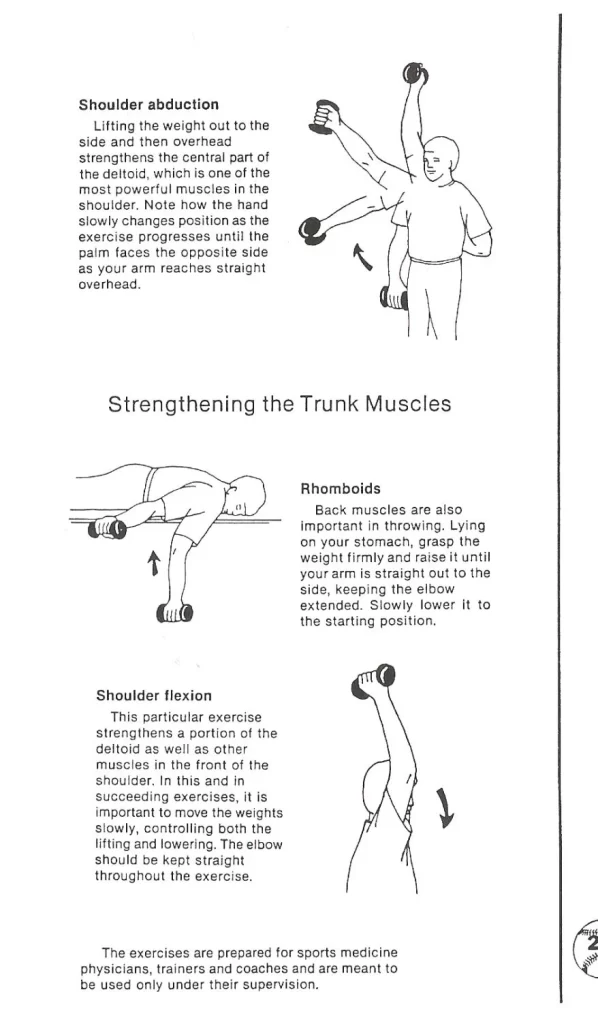
Strengthening exercise in Decerebrate Posture:
Prognosis
With just 37% of decorticated patients and 10% of decerebrate patients surviving after head injuries, abnormal posture is a concerning indicator. The death rate for children who require hospital admission owing to head injuries is generally between 10% and 13%; however, in severe instances with decerebrate posturing, the mortality rate rises to 71%.
Comparable death rates of 68% to 83% in TBI with decerebrate posture have been reported in other studies. Extradural hematoma, admission within 6 hours of damage, and younger patient age were factors that promote survival in TBI with decerebrate posture. Older age and acute subdural hematoma were associated with worse outcomes.
Results from 210 individuals with aberrant postures after hypoxic brain damage were examined. One day after the trauma, abnormal posture or a GCS motor score of less than 4 indicated that there was almost little possibility of independence returning. Individuals who displayed either decorticate or decerebrate stances after receiving a gunshot wound to the head had almost little chance of making a significant recovery. In grades 4 and 5, decerebrate posture is included in the Hunt and Hess subarachnoid hemorrhage severity grading system. They gave death rates of 42% and 77%, respectively.
Complications
Complications include poor neurological results and death, as covered under prognosis. Patients in a coma may also experience difficulties in the short term with breathing and managing their cardiorespiratory system.
Decerebrate posture is a sign of significant brain injury or a significant interruption in brain function. They could cause irreparable brain damage, which might cause the damaged brain areas to lose the abilities they formerly controlled. Conditions that might produce decerebrate posture can be fatal in the worst circumstances if left untreated.
Can you prevent decerebrate posturing?
Decerebrate posture is caused by a number of situations that might be avoided or at least lessened in likelihood. Among the things you can accomplish are:
- Take care of your long-term health issues. When it comes to treating chronic diseases such as diabetes, high blood pressure, and epilepsy, heed the advice of your healthcare practitioner.
- When necessary, put on protective gear. Decerebrate posture is frequently caused by head traumas, including concussions and traumatic brain injuries. Wearing seat belts and helmets will help prevent injuries to your brain.
- Consume a diet that is balanced. Nutrient deficits and electrolyte imbalances are frequently preventable, or at least less likely to occur. Controlling your diet can also help prevent the decerebrate posture that is linked to many disorders of the brain, particularly strokes.
- Maintain an exercise regimen and get to and stay at a healthy weight. Brain-related disorders can be prevented or delayed depending on your weight and level of activity. Your healthcare professional can offer guidance on achieving and sustaining a healthy weight for you.
- Refrain from using illegal and non-medical drugs, and consume alcohol sparingly. Decerebrate posture may have underlying causes, including substance use problems. Keep away from non-medical drugs and substance usage, and always take prescription drugs exactly as prescribed.
- Seek medical attention for infections. Numerous illnesses that impact the brain begin in the nose, ears, or eyes. Treating infections in these locations should not be put off. You may prevent the spread of diseases that cause disorders like decerebrate posturing by receiving therapy as soon as possible.
Conclusion:
Witnessing someone you love or know go through a symptom like decerebrate posturing can be frightening. This is a common sign of a brain injury or serious disease that puts the patient in a coma.
However, new developments in contemporary medicine have led to more options for both diagnosis and treatment of the underlying problems. Hope is offered to individuals who have a loved one impacted by decerebrate posturing as researchers continue to discover novel approaches to treating these illnesses.
FAQs
Is decerebrate or decorticate posturing more serious?
Both postures can be caused by brain injuries in several anatomical locations, however they generally include some degree of brainstem damage. Nonetheless, it is acknowledged that in order to decorticate, an injury must usually be more rostral than in a decerebrate posture.
How may decerebrate stiffness disappear?
Sections through the caudal tip of the pons, at the level of the vestibular nuclei, eliminate this stiffness. Therefore, the pontile tegmentum contains the structures whose activity is required to maintain decerebrate stiffness.
What consequences arise from decerebration?
Near the proper age, certain behaviors such as putting responses (including “tactile placing”), defensive reactions, auditory orienting, shivering, piloerection, reflexive feeding, and others were seen.
What differentiates decerebrate stiffness from decerebrate rigidity?
A mesencephalic lesion that causes a break between the cerebrum and the remainder of the brain and spinal cord is the cause of decerebrate stiffness. A rostral cerebellar lobe injury that results in a break between Purkinje cells and the remainder of the brain causes decerebrate stiffness.
Decerebrate preparation: what is it?
During standard (pharmacologic) general anesthesia, the cerebral cortex and thalamus of animals undergoing experimental decerebration are inactivated by surgery or other means. The animal is still alive when the pharmacologic anesthetic wears off, but it is not cognizant or experiencing pain.
What is the decerebrate posturing differential diagnosis?
Differential Diagnosis
Extensor posture accompanied by internal rotation of the upper and power limbs characterizes decerebrate posturing. This indicates that the injury has not damaged any area other than the vestibulospinal tract.
Can you withstand the posturing of decorticate?
Assistance and Continued Care. Decorticate posture is typically linked to a very poor likelihood of survival and is not frequently reversible. It is important that you talk to your loved one’s medical professionals about their prognosis if they have this physical symptom.
How may decerebrate stiffness disappear?
Sections through the caudal tip of the pons, at the level of the vestibular nuclei, eliminate this stiffness. Therefore, the pontile tegmentum contains the structures whose activity is required to maintain decerebrate stiffness.
Is it possible to undo decerebrate posturing?
When decerebrate posture is present together with hepatic encephalopathy, we should think of it as a possibly reversible finding that might leave the patient without any lasting harm, even though this finding usually prompts contemplation of irreversible problems.
Can you bounce again from a decerebrate?
What Is Decerebrate Posturing, Why It Happens, and How to Treat It Depending on the underlying reason, recovery from a disorder that results in decerebrate posturing could be achievable. Reversible or curable conditions or events are the most likely to result in recovery.
What makes decerebrate more serious?
Decerebrate posture often shows more severe damage at the rubrospinal tract; hence, the red nucleus is also affected, suggesting a lesion deeper in the brainstem. However, decorticate posturing is still indicative of serious brain injury.
Is posturing decerebrate a sign of brain death?
A person must not be able to pass any of the following tests in order to be deemed brain dead: No movement should occur on its own or in response to unpleasant stimuli (however spinal reflex movement is allowed). It is not acceptable to exhibit seizures, decerebrate or decorticate posture, or dyskinetic movements.
With decerebrate posture, whatever area of the brain is injured?
Decerebrate posture is caused by damage to deeper brain regions such as the midbrain, pons, and diencephalon.
Why does decerebrate posture occur?
Head traumas, such as concussions and serious brain damage, are the most common causes of decerebrate posture. Put on safety gear, such as seat belts, and helmets, to keep your brain safe.
What differentiates decorticate posturing from decerebrate posturing?
Whether or not the arms are bent at the elbows is the primary distinction between the two positions. A person with a decorticate posture bends their elbows and folds their arms up toward their chest. A decerebrate is someone whose limbs are all extended out from their head
References
- Physiotherapist, N. P. (2023, December 13). Decerebrate Posture: Cause, Symptoms, Diagnosis & Treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/decerebrate-posture/
- Knight, J., & Decker, L. C. (2023, July 31). Decerebrate and Decorticate Posturing. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK559135/
- Professional, C. C. M. (n.d.). Decerebrate Posturing. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/24968-decerebrate-posturing







2 Comments