Waddling Gait
Introduction
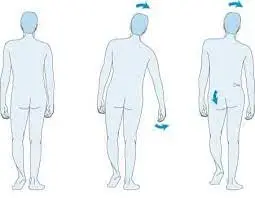
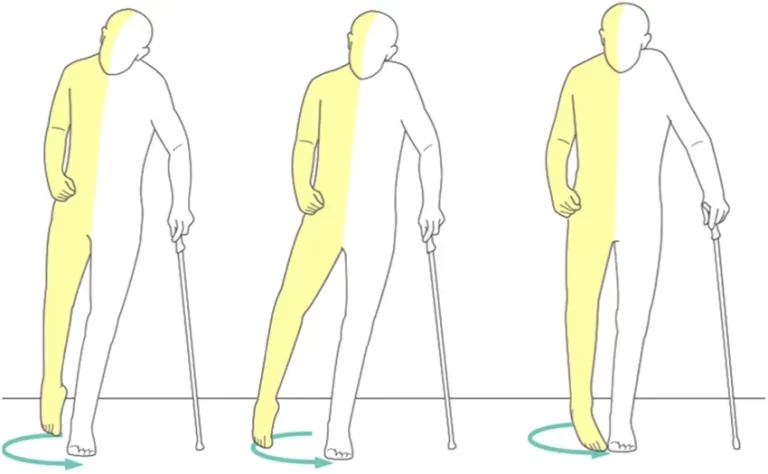
Waddling gait, also known as myopathic gait, is one example of an inappropriate gait. The reason for the waddling is a weakening of the pelvic girdle’s proximal muscles. For instance, in myopathies, weakness in the muscles of the upper thighs and hip region results in pelvic instability during standing as well as walking. When the hip joint’s extending muscles are weakened, the hip joint’s posture flexes and lumbar lordosis worsens.
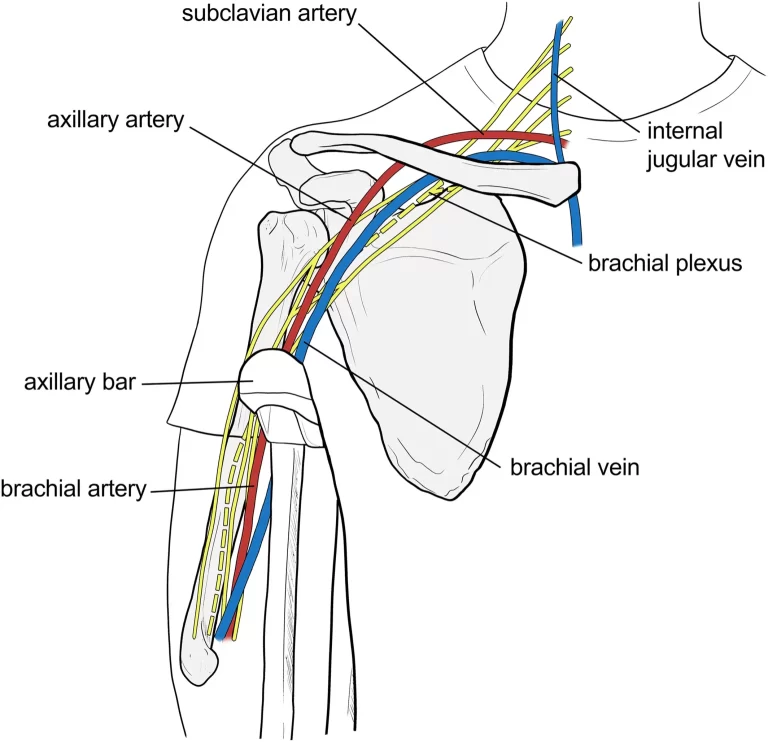
Patients typically struggle to get to their feet after sitting down. The hip on the side of the swinging leg falls with every stride because of weakening in the gluteus medius muscle (also known as the Trendelenburg sign).
Pregnancy, congenital hip dysplasia, muscular dystrophies, and spinal muscular atrophy are conditions linked to a myopathic gait. Waddling is the apparent gait. Patients often try to prevent the hip from falling on the swinging side by bending their trunk towards the side that is in the stance phase (this is known as the Duchenne sign in German literature).
When the origin and insertion point of the gluteus medius muscle are closer than normal due to orthopedic difficulties, such as posttraumatic elevation of the femoral neck’s trochanter or pseudoarthrosis.
What is the Waddling gait?
Waddling gait is another name for mayopathic gait, which is a walking form. A bowl-shaped framework of bones and muscles that connects your upper body to your hips and legs, the pelvic girdle is responsible for those muscles that are weak.
It is also in charge of assisting with your balance. A weak pelvic girdle makes walking tougher. Your body therefore sways side to side to prevent you from falling. As you walk, your hips could also sag to one side. To find out more about the reasons behind a waddling gait in kids as well as adults, continue reading.
What causes the Waddling gait?
Pregnancy
Pregnant women frequently exhibit waddling gaits, particularly in the third trimester. This might be impacted by different reasons.
- During the second trimester, your body begins to create relaxin, which relaxes and expands the ligaments and joints of your pelvis.
- A broader pelvis can change how you walk, but it also makes labor and delivery safer and easier.
- Your pelvis could widen in addition to relaxing due to the downward pressure of the growing fetus. Your stomach starts expanding greatly in the later weeks of pregnancy, which can cause your center of gravity to shift and make it more difficult to balance, particularly when walking.
- You may also begin to lean back a little when standing or walking as your spine and pelvis begin to curve in to support your expanding tummy. A waddling gait might also result from both of these conditions.
- Waddling while pregnant is common, so don’t freak out. Indeed, it may even lower your chance of falling. After delivery, waddling gaits usually come to an end, however they could persist for a few months.
Age
The majority of young children, particularly toddlers, do not walk like adults do. Perfecting balance and walking mechanics takes time. Waddling and taking little steps are common in youngsters under the age of two. But if a waddling gait persists until the age of three, it could indicate a more serious problem, particularly if it’s associated with:
- Walking on the balls of your feet.
- An enlarged stomach.
- Tripping or falling.
- Low endurance.
Kids older than three who waddle may be showing signs of:
- Muscular dystrophy.
- cerebral palsy.
- congenital hip dysplasia.
- lumbar lordosis.
Lumbar lordosis is one of these disorders that frequently resolves on its own. Others, on the other hand, need to be treated, therefore it’s ideal to collaborate with your child’s pediatrician to identify the root reason. In certain situations, your child might only require physical therapy.
Muscular Dystrophy (MD)
A class of rare disorders known as muscular dystrophy (MD) weakens muscles and eventually causes them to break down. A waddling gait is suggestive of some MDs, including:
- Duchenne Muscular Dystrophy: Boys are almost entirely affected by Duchenne muscular dystrophy, a disorder that affects the arms, legs, and pelvis. One of the first indications is difficulty crawling or getting off the ground.
- Becker Muscular Dystrophy: This disorder, which is a milder version of Duchenne MD, is likewise more prevalent in boys. It affects the shoulder, hip, pelvic, and thigh musculature. In late childhood or early adolescence, Becker MD is frequently diagnosed.
Although MD cannot be cured, there are ways to improve mobility and decrease the disease’s progression. Such therapies include assistive devices, physical therapy, medication surgery, and gait training.
Hip dysplasia in infants
The hip joints of some infants do not develop normally. As a result, hip dislocation is considerably more likely due to shallow hip sockets. Instability can occasionally result from loose ligaments holding the hip joint in place. Hip dysplasia in infants can develop during the first year of life or be present from birth. In certain cases, newborn hip dysplasia can also result from overly tight swaddling.
Additional indicators of neonatal hip dysplasia include:
- Different lengths of legs.
- Walking on tiptoe or with a limp.
- Reduced range of motion or flexibility in one leg or a particular side of the body.
- Uneven folds of skin on the thighs.
Hip dysplasia in infants is often screened and diagnosed by pediatricians at birth and during the first year of routine examinations. It can typically be addressed with supportive aids, like a brace or harness, if detected early. Older babies may need a body cast or surgery for the right treatment.
Spinal muscular atrophy (SMA)
SMA, or spinal muscular atrophy, is a neurological condition that is acquired. This weakness in the muscles and other problems have been triggered by the degeneration of your spinal cord’s motor neurons. Thigh muscle weakness and loss are symptoms of autosomal dominant spinal muscular atrophy with lower extremity predominance, a kind of SMA. Occasionally, infancy is when this kind of SMA typically initially appears.
Autosomal dominant spinal muscular atrophy with lower extremity predominance can also result in a waddling gait, as well as:
- Foot abnormalities.
- Muscular tone (high or low).
- Excessive curvature of the lower back.
- Respiratory issues.
- The head is small in size.
Although there isn’t a cure for SMA, symptoms can be managed with medicine, physical therapy, and surgery.
How is Waddling Gait diagnosed?
There are multiple ways to identify the cause of a waddling gait. Along with a physical examination, your doctor will discuss your symptoms with you. They might additionally verify:
- Coordination, tone, and strength of muscles.
- Check for any irregularities in your neck and spine.
- To figure out your vulnerability to falls.
- Blood pressure readings when standing and sleeping.
- Your outlook.
- Regarding neurological conditions like muscular dystrophy.
- For arthritis.
Based on the findings, more testing or imaging investigations might be required.
- Using genetic testing to find particular disease indicators.
- Muscle biopsy for confirmation of muscle disorders.
- An enzyme blood test to look for signs of MD, such as increased creatine kinase levels.
- Using ultrasonography to detect hip dysplasia.
What’s the Treatment for Waddling Gait?
The etiology of the waddling gait will determine the course of treatment. Several circumstances may improve on their own. Additional alternatives for treatment include:
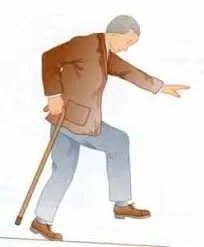
- Walkers and canes for equilibrium.
- Physical therapy to support flexibility, balance, and strength.
- Fall safety precautions
- Splints or leg braces to assist in foot alignment
- Health Care
- Prosthetics or surgery
Physical therapy for Waddling Gait
Physical therapy is a common and effective therapy for the waddling gait. Its main goals are to increase overall coordination, increase flexibility, and strengthen the weaker muscles.
- Strengthening exercises: Exercises that target strengthen the gluteus medius and other hip abductor muscles. This can involve hip bridges, clamshells, and side-lying hip abduction.
- Stretching exercises: Exercises that increase the flexibility of the back, legs, and hips.
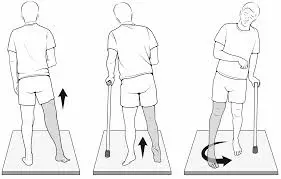
- Balance exercises: Exercises for balance include using a balancing board, walking in pairs, and standing on one leg. They also improve balance and stability. Enhancing balance and reducing the risk of falling can be achieved through particular balancing exercises and activities.
- Correcting Posture: To increase efficiency and lessen muscle strain, physical therapists can assist people with waddling gait in learning appropriate posture and body alignment.
- Proprioception training: Activities like walking on uneven terrain or closing your eyes while standing that improve coordination and body awareness.
- Assistive equipment: To offer assistance and enhance mobility, it may occasionally be advised to use assistive equipment like canes or braces.
- Aquatic Therapy: Water-based workouts can provide a low-impact means of enhancing coordination, strength, and flexibility. This is known as aquatic therapy.
Exercises for Improving Waddling Gait
The following exercises may be beneficial in building muscle strength in the areas required for keeping a stable gait:

Side Lying Hip Abduction:
- With your legs positioned on top of one other and your knees slightly arched, rest on your side.
- Make sure your top foot is flat on the ground and maintain a hip-shoulder alignment.
- Gently elevate your upper leg in the direction of the roof while keeping it in line with your body.
- After a few seconds of holding the highest position, carefully lower your leg back down.
- Keep performing ten to twelve times on each of the sides.

Clamshell:
- Lying on your side, hold your feet and flex your knees.
- Hold your feet together and open your knees like a clamshell.
- Use theraband for resistance.
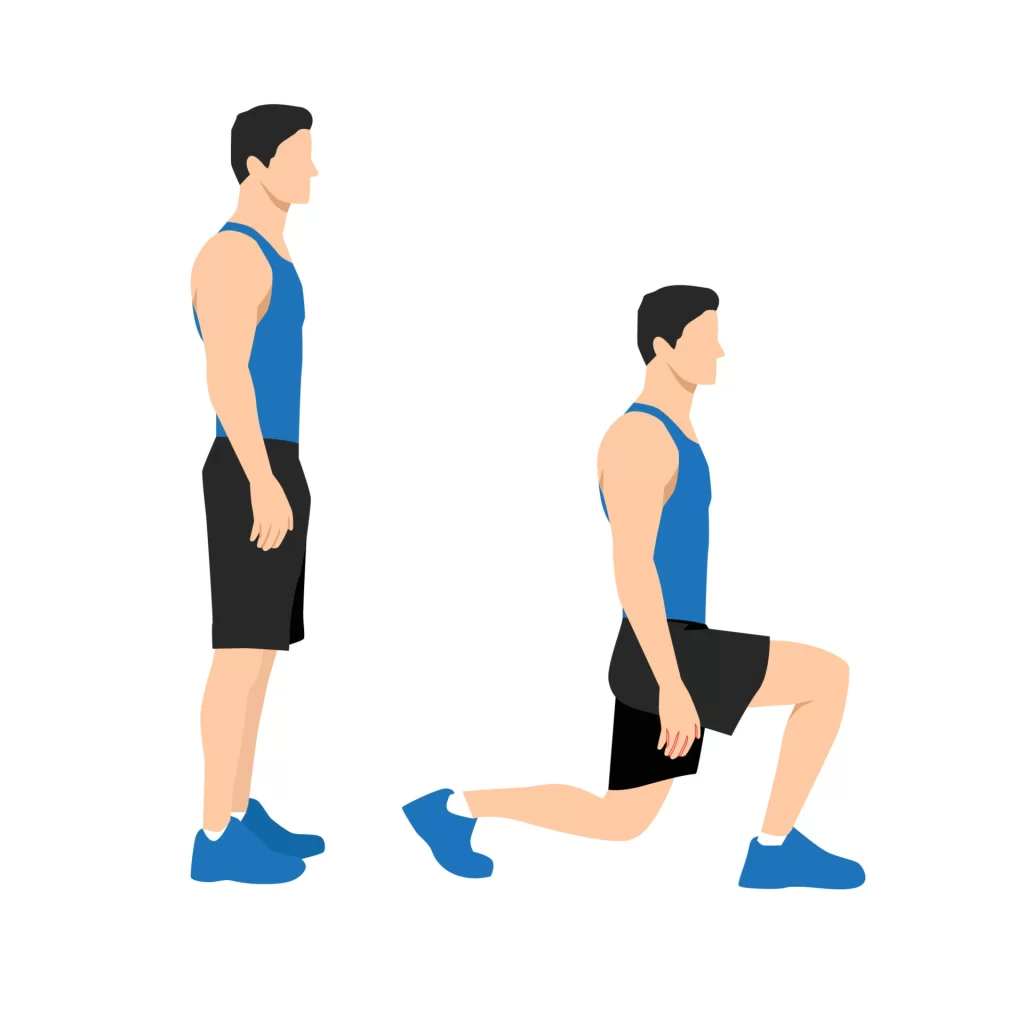
Lunges:
- Step forward on one leg and lower yourself until your knees are 90 degrees bent.
- Preserving an erect back is essential when performing lunge movements.

Bridge:
- Flex your knees and place both feet gently on the carpet while you lie on your backside.
- Raise your hips away towards the ceiling so that your knees and shoulders line up.

One-Leg Stand:
- Assume a standing posture with your feet together, arms by your sides, or grasping the chair.
- Preservation of an erect knee, carefully lift one leg off the base.
- To retain your balance, stand on one leg for as long as you can. With another leg, repeat the process.
Tandem Stance:
- Bringing both feet together, step one foot directly behind the other to balance on a narrow base.
Summary
Pregnant women frequently experience waddling gait, which usually goes away a few months or soon after the baby is born. It also frequently goes away on its own in kids under the age of two. If not, it can be a sign of a more serious illness like MD or baby hip dysplasia.
FAQs
What is the waddling gait?
A waddling stride, which resembles the walk of a duck, is produced by overdoing the movement of your upper body. Waddling gait can result from either hip dislocation or a slow, inherited muscle deterioration.
What sort of waddling gait occurs by muscle weakness?
Myopathic gait is another name for waddling gait, which is a walking manner. Your muscle weakness comes from the pelvic girdle, a structure composed of bones and muscles that form a bowl and join your torso to your hips and legs. It is also responsible for helping you maintain that sense of balance
What is the appearance of a waddling gait?
Waddling down to the river were the ducks. A chubby, short waiter approached. The penguins swam in their pool and waddled on their rocks. An old female customer waddled in as the door jangled.
Can the waddling gait be cured?
Early intervention and focused therapies, including physical therapy, can often address the root reasons for a waddling gait and help improve function and mobility.
How can one stop their walking waddling?
Strengthening Your Hamstrings: During walking, your hamstring muscles, which are located in the rear of your thighs, are essential for stability and balance. Waddling lessens the chance of developing a waddling gait by strengthening these muscles with workouts like leg curls and bridges.
References
- Kahn, A. (2018, September 29). Walking Abnormalities. Healthline. https://www.healthline.com/health/walking-abnormalities#diagnosis
- Wikipedia contributors. (2023, April 12). Myopathic gait. Wikipedia. https://en.wikipedia.org/wiki/Myopathic_gait
- What to Know About Waddling Gait. (2024, February 15). WebMD. https://www.webmd.com/a-to-z-guides/what-to-know-waddling-gait