Posterior Cruciate Ligament Injury
What is Posterior Cruciate Ligament Injury?
The posterior cruciate ligament (PCL) prevents the tibia from shifting rearward concerning the femur is the PCL’s function. PCL injuries rarely happen alone, although they frequently coexist with other knee components (meniscus, ligaments). Every year, there are about two PCL injuries for every 100,000 people.
A stretch to a complete tear or rupture of the posterior cruciate ligament (PCL) is the possible forms of injury. These injuries are not very prevalent. Due to the PCL’s greater strength and width, they are less common than anterior cruciate ligament (ACL) injuries.
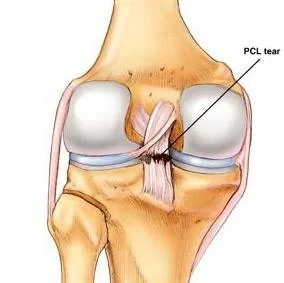
One of the four main ligaments of the knee joint, the posterior cruciate ligament (PCL), serves to support the tibia on the femur. It attaches to the posterior aspect of the tibial plateau after emerging from the anterolateral aspect of the medial femoral condyle near the intercondylar notch. Its purpose is to stop the tibia from posteriorly translating onto the femur. The PCL resists external rotation forces, varus, and valgus to a lesser degree. It is less likely to sustain damage since it is roughly 1.3 to 2 times as thick and almost twice as robust as the anterior cruciate ligament (ACL).
Compared to injuries to the anterior cruciate ligament (ACL), the knee’s more vulnerable counterpart, the posterior cruciate ligament injuries (PCL injuries) occur much less frequently. Your thigh bone (femur) and shinbone (tibia) are joined by the ACL and posterior cruciate ligament. One may experience pain, swelling, and a sense of instability if either ligament is torn.
Strong tissue bands called ligaments connect one bone to another. The thighbone (femur) and shinbone (tibia) are joined by the cruciate ligaments (KROO-she-ate). An “X” is formed in the middle of the knee by the anterior and posterior cruciate ligaments.
A posterior cruciate ligament injury can keep you out of commission for weeks or months, but it usually results in less pain, disability, and knee instability than an ACL tear.
The lateral femoral condyle has been removed to expose the PCL’s anatomy in this medial view of the flexed knee. Tensile tension, seen in red, on the PCL’s anterolateral bundle results from excessive flexion, or hyperflexion, which causes PCL damage because the anterolateral bundle is stretched and the posteromedial bundle relaxes during flexion.
The PCL’s role in this position is to stop the tibia from moving posteriorly and to stop the patella from tilting or changing. Nevertheless, the PCL is vulnerable to damage from hyperflexion, hyperextension, and a process called a dashboard injury due to the relative flexibility of the two portions. Ligaments can only withstand greater stress when the load is gradually increased due to their viscoelastic nature.
The PCL stretches or tears when this elastic characteristic is combined with abrupt hyperflexion and hyperextension. The third and most frequent mechanism, known as the dashboard injury mechanism, occurs when the knee flexes toward the area above the tibia and is struck posteriorly. These mechanisms take place when the knee is flexed or when there is excessive external tibial rotation. They also happen after falls that cause varus-extension stress, which is a mix of tibial extension and adduction.
Anatomy of Posterior Cruciate Ligament Injury:
It begins at the internal surface of the medial femoral condyle and ends 1 centimeter below the tibia’s articular surface at the center of the posterior portion of the tibial plateau. With the anterior cruciate ligament in front and the posterior cruciate ligament in the rear, they cross one another to create a “X.” The cruciate ligaments regulate your knee’s back-and-forth movement.
The large anterolateral (AL) bundle and the smaller posteromedial (PM) bundle are the two inseparable bundles that make up the PCL. The PM bundle is most taut during deep flexion and extension of the knee, whereas the AL bundle is most taut during internal rotation and mid-flexion. Each bundle has a different fiber orientation. In extension, the AL bundle is more horizontally oriented, and as the knee flexes past 30°, it becomes more vertical. During knee extension, the PM bundle is oriented vertically; across a comparable range of motion, it becomes increasingly horizontal.
One of the knee’s two cruciate ligaments is the PCL. It serves as the knee’s main stabilizing ligament. It keeps the tibia from moving too far posteriorly concerning the femur. Additionally, it reduces internal rotation, adduction, and abduction at the knee joint and prevents hyperextension. Due to its robust nature, the PCL sustains fewer injuries than the ACL since it is twice as thick. PCL injuries are, therefore, less frequent than ACL injuries.
Epidemiology:
People with acute PCL injuries are often in their 20s to 30s. While PCL injuries can happen on their own, primarily from sports, they typically happen in combination with other ligamentous injuries caused by auto accidents. Posterolateral corner injuries are the most common presentation of PCL injuries, which make up 44% of acute knee injuries. Prominent collegiate football players are thought to have a 2-3% incidence of chronic, asymptomatic PCL insufficiency.
Car crashes (45%) and sports injuries (40%) were the two most frequent causes of PCL injuries. In particular, injuries from soccer-related incidents (25%) and motorbike accidents (28%) are the two most frequent causes. Dashboard injuries accounted for 35% of all injuries, while falls on a flexed knee with the foot in plantar flexion accounted for 24%.
Pathophysiology:
The PCL inserts extra-articularly onto the posterior aspect of the tibial plateau after emerging from the anterolateral aspect of the medial femoral condyle near the intercondylar notch. It is almost twice as strong and 1.3 to 2 times thicker than the ACL. It can be further divided into bundles that are posteromedial and anterolateral.
The PCL’s anterolateral and posteromedial bands make up 35% and 65% of its body, respectively. Whereas the posteromedial bundle is strict in knee extension and loose in knee flexion, the anterolateral bundle is taught in knee flexion and loose in knee extension.
The PCL’s work is to stop the tibia from posteriorly translating onto the femur. The anterolateral region is more frequently harmed because most injuries happen during knee flexion. The main restriction on posterior tibial translation between 30 and 90 degrees is the PCL. 95% of posterior translational forces are accepted by the PCL at 90 degrees. With the help of the posterior oblique ligament, popliteus, medial collateral ligament, and posterolateral joint capsule, it resists posterior translation. The middle geniculate artery supplies blood to the posterior cruciate ligament, which is innervated by the tibial nerve.
Mechanism of Injury:
A direct strike to the anterior aspect of the proximal tibia on a flexed knee with the ankle in plantarflexion is the most common mechanism of injury. This frequently manifests as dashboard injuries sustained in auto accidents, which causes the tibia to translate posteriorly. PCL tears may also result from hyperextension and rotational or varus/valgus stress mechanisms.
The majority of these injuries happen while playing sports like football, soccer, and skiing. Athletes frequently report isolated PCL injuries, with hyper-flexion being the most common mechanism of injury. Rarely do athletes claim to hear a pop, and they might be able to resume playing right away following an injury. A quick change of direction, a simple misstep, or poor jump landings are other mechanisms of PCL damage.
Causes of Posterior Cruciate Ligament Injury:
A blow to the knee while it is suddenly bent is frequently the cause of PCL injuries.
Both high-energy and low-energy injuries can result in PCL damage. The most frequent cause of injury to the PCL alone is a direct hit to the front of the knee when it is bent. The PCL can rupture if the tibia goes too far rearward in reference to the femur because it regulates this movement.
Occasionally, the PCL sustains injuries in a car collision. When someone slides forward after a sharp stop or collision, their knee may strike the dashboard just behind their kneecap. The PCL is injured in this scenario because the tibia is pushed backward beneath the femur. A person who falls on a bent knee may experience the same issue. Once more, the PCL may be stressed and even torn if the tibia is pulled backward.
When the knee is abruptly hyperextended, other ligaments are typically injured before the PCL, however, other components of the knee may also sustain damage. When the foot is planted on the ground, the knee may be impacted from the front, resulting in this kind of injury.
An excessive anterior force applied to the proximal tibia of the flexed knee results in PCL injuries. Dashboard injuries, which occur when the knee is pushed against the dashboard after a motor vehicle crash, are among the frequent causes. Falling forward onto a flexed knee can potentially cause damage to the PCL. PCL injuries are most frequently seen in baseball, football, soccer, and skiing. Less frequently, a rotational hyperextension injury to the knee joint might cause harm.
Typical reasons include:
- In a car accident, striking the knee on the dashboard
- Tripping and falling on a bent knee,
PCL injuries are frequently caused by sports. These injuries are particularly prevalent in:
- Football
- Soccer
- Baseball
- Skiing.
Symptoms of Posterior cruciate ligament injury:
A PCL rupture can cause a variety of symptoms. Unlike the ACL, the PCL is not truly encased inside the knee joint. Therefore, PCL injuries do not cause as much knee swelling as an ACL rupture, which causes the joint to swell with blood. The majority of PCL-damaged patients experience some edema and stiffness. Additionally, some individuals may have knee instability and give way, particularly while attempting to change direction. It could seem like the knee wants to slip.
After two to four weeks, the initial injury’s pain and mild swelling should go away, but the knee may remain unsteady. What has to be treated are the symptoms of instability and the incapacity to rely on the knee for support. Orthopedic doctors’ increasing recognition that chronic instability causes early knee arthritis is also crucial when making treatment decisions.
Typical signs of a posterior cruciate ligament damage include the following:
- Knee pain and edema that develop gradually and rapidly following the injury
- Swelling that stiffens the knee and could result in a limp
- Having difficulty walking
- The knee feels unstable, as if it would “give out.”
Acute PCL injury:
Isolated injury:
Patients frequently have limited and hazy symptoms, and they may not even be aware of or feel the damage. There is a nearly normal gait pattern, little pain, edema, instability, and full range of motion.
Combination with other ligamentous injuries:
Symptoms vary depending on how severe the knee injury is. This includes edema, pain, a sense of unsteadiness, restricted mobility, and trouble mobilizing. There may also be bruises.
Chronic PCL injury:
Common complaints include knee pain while walking long distances and pain when bearing weight in a semi-flexed position (such as when crouching or ascending stairs). Instability complaints are also common, primarily when walking on uneven terrain. There may also be pain in the medial compartment of the knee and retropatellar pain. The extent of related chondral injury determines potential stiffness and edema.
Grading of Posterior cruciate ligament injury:
- Grade I: There is a little tear in the PCL.
- Grade II: The PCL ligament is loose and just slightly damaged.
- Grade III: The knee can now be classified as unstable because the PCL has been totally torn.
- Grade IV: both the ligament and another knee ligament are injured.
Differential diagnosis:
- ACL injury
- Medial collateral ligament injury
- Talofibular ligament injury
- Menisci injuries
- Patellofemoral joint injuries
- Posterolateral knee injury and associated varus instability
- Multiligament knee injury
- Femoral condyle fracture
- Tibial plateau fracture.
Diagnosis:
Your doctor may apply pressure to your knee during the physical examination to check for damage, looseness, or bleeding fluid in the joint. He or she may ask you to stand and walk while moving your foot, leg, or knee in various directions. In order to check for any sagging or unusual movement in the knee or shinbone, your doctor will compare your affected leg with the healthy one.
Your physician might recommend one or more of the following imaging tests for specific conditions:
X-ray: An X-ray can show bone fractures, but cannot identify ligament injury. Avulsion fractures, in which a tiny piece of bone linked to the ligament tears away from the main bone, can occur in people who have suffered injuries to the posterior cruciate ligament.
MRI scan: This painless process creates computer images of your body’s soft tissues by using radio waves and a powerful magnetic field. A posterior cruciate ligament tear can be seen clearly on an MRI scan, which can also reveal any further injuries to the knee’s ligaments or cartilage.
Physical examination:
To differentiate between various presentations, a thorough history is taken in order to understand the nature of the symptoms and the process of injury. The usual presentation is a limited range of motion and difficulties bearing weight. Symptoms and the mechanism of damage will determine whether to rule out fracture and dislocation.
Patients frequently complain of instability, edema, and acute-onset posterior knee pain when they first arrive. The mechanism of injury, such as trauma from falling onto a flexed knee or a recent car accident, is part of a comprehensive history. Similar to what is commonly described with ACL tears, there may or may not be a “pop” complaint with PCL tears.
A comprehensive knee examination should be carried out, encompassing gait analysis and overall limb alignment. It is also necessary to evaluate the lower extremity’s neurovascular integrity distal to the injury. When distal pulses are feeble or the Ankle-Brachial Index is less than 0.8, an intimal tear to the popliteal artery should be considered and further investigated using arteriography. If there is an obvious vascular deficiency, angiography shouldn’t postpone treatment.
Evaluation:
Plain X-rays should be the only imaging method used initially. To check for related fractures, arthritis, and joint effusion, compare the contralateral views of the ipsilateral standing AP, 45-degree flexion weight-bearing, and merchant patellar views. The 45-degree flexion image may also reveal a positive sag in comparison to the contralateral knee.
The gold standard for assessing a PCL injury is MRI. According to reports, its accuracy ranges from 96% to 100%. Additionally, it can evaluate for concurrent injuries such as popliteus, medial collateral ligament, meniscal, ligamentous, posterolateral joint capsule, and posterior oblique ligament injuries. Acute damage is suggested by an increase in signal within the PCL substance or a disruption in the continuity of the ligament fibers on T1- and T2-weighted sagittal MRI images. The posterior tibial translation is a sign of chronic PCL injury. When ligament continuity is restored on MRI, posterior translation less than 8 mm may be recovered.
Special Test:
Posterior Drawer Test:
The most reliable test for determining PCL integrity is this one. The patient is in a supine posture during the procedure, with the knee and hip flexed to 90 and 45 degrees, respectively. While the femur is stabilized, a posterior force is delivered to the proximal tibia. Reduction to the neutral position is typically required prior to posterior force delivery because the tibia will be posteriorly translated in relation to the femur in PCL damage. As supplementary restrictions on posterior tibial translation, internal rotation reduces it by tightening the superficial medial collateral ligament and posterior oblique ligaments. Therefore, the tibia translates >10-12 mm in neutral and 6-8 mm in internal rotation in isolated PCL injuries, whereas the tibia translates >15 mm in neutral and >10 mm in internal rotation in combined ligamentous injuries.
Posterior sag sign:
The patient is asked to lie in the supine position with both knees and hips flexed to 90 degrees. Both legs and heels are held by the examiner. A damaged or inadequate PCL is indicated by posterior tibial translation.
The quadriceps active test:
Useful in the diagnosis of a full PCL injury. The patient is in a supine position with their knee fully extended. After stabilizing the patient’s foot, the examiner asks them to try extending their knee, which causes their quadriceps to contract isometrically. A posteriorly translated tibia will decrease in relation to the femur in cases of full PCL injury.
Dial test or external rotation test:
The combined PCL and PLC injuries are diagnosed using this test. The patient may be placed in a supine or prone position. The examiner compares both sides after externally rotating both feet at 30° and 90° of knee flexion. Asymmetry that is 10° or greater is deemed abnormal. A combined PCL and PLC injury is suggested by increased external rotation at both 30° and 90°, whereas an isolated PLC injury is suggested by increased external rotation at only 30°.
Varus/Valgus stress:
This evaluates collateral ligament injury alone against combined PCL and collateral ligament injury. A combination injury, either MCL or LCL and PCL, is suggested by laxity at 0°. However, laxity at 30° by itself may indicate MCL or LCL damage.
Treatment of Posterior cruciate ligament injury:
Medical Treatment:
- NSAID painkillers, including naproxen sodium (Aleve) or ibuprofen (Advil, Motrin IB, and others), can help lower swelling and ease pain.
- Keep the knee immobile within its range of motion. extension of the brace locked in for two to three weeks
- Weight-bearing assistance (partial to full) for two weeks.
Surgical Treatment:
Rebuilding the ligament: Rebuilding a ruptured posterior cruciate ligament is necessary since the ligament ends typically do not heal when sewn back together. Your physician will use a tissue graft to restore your injured ligament. This graft is taken from a cadaver or another human donor, or from another region of your body. The graft’s integration into your bone may take several months.
Procedure: Using an arthroscope and tiny incisions, surgery is performed to repair a posterior cruciate ligament. A less intrusive procedure is arthroscopic surgery. reduced intrusive procedures have the advantages of shorter recovery periods, reduced hospital stays, and less surgical pain.
Physical Therapy Treatment:
Techniques for reducing pain that apply the RICE Principle.
- Rest
- Ice: 10-20 minutes every 2-4 hours
- Elevation
- Compression
- Hydrotherapy
- Transcutaneous electrical nerve stimulation (TENS).
Exercise in Posterior Cruciate Ligament Injury:
Static Quad sets of Exercise:
- With one leg bent and the injured leg straight, sit on the floor.
- Tighten the muscles on the top of your thigh to press the rear of your affected leg’s knee into the floor.
- Hold this posture for ten seconds.
- Perform two sets of fifteen.
Seated quadriceps strengthening exercise:
- With your damaged knee bent at a 90-degree angle, take a seat in a straight-back chair.
- Without moving your leg, try to contract the muscles at the top of your thighs.
- Hold for ten seconds.
- Perform two sets of fifteen.
Straight leg raise (SLR):

- Place your legs straight out in front of you while lying on your back.
- Place the foot flat on the floor and bend the knee on the side that is not hurt.
- Raise your leg about 8 inches off the ground while contracting the thigh muscle on the side that is affected.
- Maintain a straight leg and taut thigh muscles.
- Return your leg to the floor gradually.
- Perform two sets of fifteen.
Wall squat with a ball:

- Hold yourself against a wall with your head, shoulders, and back.
- Look directly forward.
- Maintain a comfortable posture with your feet shoulder-width apart and three feet (90 cm) from the wall.
- Put a basketball or soccer-sized ball behind your back.
- Slowly stoop down to a 45-degree angle while maintaining your back against the wall.
- At this point, your thighs won’t be parallel to the ground.
- After ten seconds of holding this posture, carefully slide back up the wall.
- Do this ten times. Reach two sets of fifteen.
Side leg raises:
- With your legs stacked, lie on one side.
- For support, bend the bottom leg. Raise the upper leg to a 45-degree angle and straighten it. Repeat ten to fifteen times after holding for five seconds, lowering, and briefly relaxing.
- Change sides and begin anew.
- As you elevate your upper leg, point its toe slightly toward the floor.
Heel Slides:
- Sit with your legs straight out in front of you to begin.
- Put a belt around the foot’s affected end.
- With your leg pointing straight up, slide your heel as close to your buttocks as you can.
- To help with the movement, use the belt.
- Hold as instructed, then slowly go back to the beginning position and do it again.
Hamstring Set:
- Rest on your back.
- As directed by your clinician, bend the affected knee at an angle.
- Draw your toes up to you.
- Push your heel into the bed gently.
- As directed, maintain this posture.
Ankle Circles:

- Before you straighten your leg to perform the ankle circles, sit up straight and support your back.
- For the necessary amount of repetitions, raise your leg and start moving your foot in big, slow circles in a single direction.
- Change your legs and move your other ankle in circles in the same direction.
- Reverse the direction of the action and switch legs once more.
- Complete the necessary number of repetitions with one ankle first, then the other.
- As you feel the strain in your ankle, foot, and lower leg, try to stretch them as much as you can.
For individuals with isolated grade I or II PCL injuries or those with grade III injuries who only engage in low-demand activities or have moderate symptoms, nonsurgical therapy has been recommended. The severity of the injury and the patient’s presentation determine how well the patient progresses through the phases of the rehabilitation program, which have broad time limits.
Phase I (Protective Phase) Week 1-6:
Effusion control, knee range of motion within recommended bounds, normalization of gait, and quadriceps muscle reactivation should be the main objectives of treatment during the initial weeks. During this first stage, it is best to avoid hyperextension of the knee and posterior tibial translation.
It is typical to have loss of motion, edema, and widespread knee pain right after an injury. It has been demonstrated that joint effusion inhibits the quadriceps, leading to muscle loss and consequent “knee buckling.”
Cryotherapy, elevation, joint compression, transcutaneous electrical stimulation, and manual therapy techniques are among the treatment approaches used to treat effusion. The patient can start moving away from crutches after the effusion is under control and they are able to elevate their legs straight without experiencing a quadriceps lag. Depending on the severity of the injury, weight bearing may be restricted to either partial weight bearing (PWB) or weight bearing as tolerated (WBAT) during the first two weeks.
Phase II (Transitional Phase) Week 6-12:
Phase II aims to strengthen the lower extremities and improve proprioception so that light, low-impact exercises can be performed painlessly and without effusion. Full knee range of motion should be attained by patients who are fully weight bearing. It is nevertheless important to avoid posterior tibial translation and knee hyperextension.
Squats and leg presses are examples of closed kinetic chain workouts that are used for strengthening and are restricted to flexion ranges of 0 to 70°. The patient and therapist must make sure that compensatory movements, including genu valgus and shifting away from the damaged limb (leg dominance), are avoided when performing squats. Leg dominance may put both limbs at risk because it is related to side-to-side symmetry, balance, and muscular strength. As a result, the stronger limb will experience high forces due to increasing dependency and excessive loading, while the weaker limb’s capacity to dissipate forces will be weakened. Proprioceptive exercises are progressed on different unstable surfaces and from double to single limb.
Phase III (Functional Phase) Week 12-16:
The objective of phase III is to resume light activities, such as a jogging program, and to stop any bracing. Based on strength and movement quality, closed-chain workouts can develop past 70° and to single-limb activities. Exercises for the hamstrings can be done alone and progressed as tolerated. To reestablish dynamic stabilization of the knee joint, proprioception, neuromuscular control, and core strengthening are advanced. The patient must be pain-free and free from obstructions during functional exercises, as well as have adequate strength and stability on one limb, before progressing to running. Focusing on coordination and movement quality unique to the patient’s sport or aspirations may be the first step in agility training.
Return to Play Phase: Week 16-24:
A full-strength foundation for advanced motions and functional exercises, endurance, sports-specific agility, neuromuscular control, and ensuring movement quality to prevent re-injury are the focus of subsequent stages. In order to prevent future injuries and re-injuries, compensatory motions should be evaluated and treated. Plyometric exercises and dynamic stabilization drills are progressed from double-limb to single-limb. Explosive plyometric exercises are designed to increase strength, speed, and power. Jumping, landing, and cutting maneuvers in different planes of motion and intensities are all part of these sports.
How to Prevent Posterior Cruciate Ligament Injury:
Completely avoiding PCL injuries might be challenging. Nonetheless, you can lower your risk in several ways:
- To maintain the health of your knee joints, stretch before engaging in any physical activity.
- When you’re running or walking, use the right form.
- When participating in sports, remain vigilant and exercise prudence.
Knee injury:
Athletes and other physically active persons frequently sustain knee injuries, which are always avoidable. More than 40% of knee injuries are caused by ligament tears, with the posterior cruciate ligament being one of the less frequent injuries. Even though this kind of knee injury is less frequent, there are still crucial precautions that may be taken. To prevent injuries, it is essential to maintain appropriate exercise and sport technique, which includes warming up and cooling down appropriately and avoiding overdoing it or going beyond the knee’s natural range of motion.
Quadriceps and hamstring ratio:
Because they aid in knee stabilization, having strong quadriceps and hamstrings is another crucial component of keeping a knee injury-free. Knee injuries are linked to a poor hamstring-to-quadriceps ratio, which should be about 80%. Exercises like leg curls, leg lifts, prone knee flexion with a resistance band, and knee extensions can help build stronger quadriceps and hamstrings. Stretching the hamstring muscles by extending the legs, toes pointing up, bending forward until the stretch is felt, and holding for a few seconds are some ways to assist in preventing injury to the posterior cruciate ligament.
Exercises and stretches:
Furthermore, balancing exercises have gained popularity because it has been demonstrated that those with poor balance are more likely to sustain knee injuries than those with strong balance. When used by qualified professionals, wobble boards and Bosu balls are popular tools for improving balance and reducing the risk of knee problems. Wearing knee straps to assist in stabilizing and protecting the knee, particularly during intense sports like football, is another potential preventive approach.
Complications:
- Intraoperative and Postoperative Complications of PCL Surgery,
- Neurovascular injury (e.g, Popliteal artery injury).
- Fracture.
- Residual instability.
- Osteoarthritic progression (Patellofemoral and medial tibiofemoral).
- Osteonecrosis.
- Stiffness.
- Failure of associated ligament reconstructions or meniscal repairs.
- Revision of PCL reconstruction.
- Chronic Knee Instability: If left untreated, a full PCL tear can cause chronic knee instability that interferes with everyday activities and movement.
- Post-Traumatic Arthritis: Osteoarthritis can develop as a result of PCL injuries, which over time can increase knee joint wear and tear.
- Pain and edema: Following physical exercise, some patients may report persistent knee pain, edema, and stiffness.
- Limited Range of Motion: Knee movement may be limited as a result of severe injuries or inadequate recovery.
- Weakness in the Hamstrings and Quadriceps: Changes in knee mechanics following an injury can lead to muscle imbalances.
- Increased Risk of More Injuries: A person who has an unstable knee may be more vulnerable to further damage to their ligaments, meniscus, or cartilage.
- Surgery-related complications (if necessary): Reconstruction surgery entails risks of infection, graft failure, or stiffness from the creation of scar tissue.
Prognosis:
You might recover without any problems if your PCL damage is minimal. However, unless you have surgery, your knee may become weak and prone to re-injury if the ligament is severely damaged.
After recovering from PCL surgery, most patients report increased stability and mobility. However, keep in mind that to safeguard your joint, you might still need to wear a knee brace when engaging in vigorous activities.
The severity of an injury to the posterior cruciate ligament (PCL) and the treatment strategy selected will determine the prognosis. Most people can return to normal knee function in three to six months with non-surgical treatment for mild to moderate (Grades I and II) PCL injuries, which includes bracing and physical therapy. Many patients can still operate well after rehabilitation, even if complete PCL tears (Grade III) may cause some knee instability. Surgical reconstruction is frequently necessary in cases with multi-ligament injuries (Grade IV), resulting in a longer recovery period of nine to twelve months. Knee osteoarthritis risk may be elevated by severe or chronic PCL injuries that go untreated. Nonetheless, the majority of patients experience positive functional results when treated appropriately.
Conclusion:
Even while PCL injuries can be severe and painful, they can be effectively managed with the right care. Completing physical therapy and paying attention to your doctor’s advice might hasten your recovery and allow you to resume your regular activities.
In conclusion, the degree of PCL injuries varies, but most people may regain good knee function with the right care, whether it be non-surgical rehabilitation or surgical restoration. While severe or multi-ligament injuries may necessitate surgery for stabilization, mild to moderate injuries frequently recover adequately with bracing and physical therapy. On the other hand, chronic instability and an elevated risk of osteoarthritis may arise if treatment is not received. For the best recovery and long-term knee health, early diagnosis, appropriate treatment, and a planned rehabilitation program are crucial.
FAQs:
How is non-surgical PCL treated?
Guidelines for Treatment
Use ice, a cryotherapy cuff, and elevation to lessen pain and swelling. Do not overextend yourself (12 weeks). Stop the tibial posterior translation (12 weeks). For 12 weeks, you should refrain from doing isolated hamstring exercises.
What is the healing time for PCL?
Depending on the extent of the injury, recovery from a PCL sprain or tear varies. Ten days to two weeks are needed for the healing of mild (Grade 1) sprains. It takes three to four weeks for moderate (Grade 2) sprains to heal completely. When deciding when to resume their sport, athletes should consult with their doctor.
Where is the location of PCL pain?
A PCL injury manifests as the following symptoms:
pain and soreness in the popliteal fossa, the area behind the knee instability of the knee joint.
Can PCL grow back?
Your PCL may be torn by a sports injury or a fall that hits the front of your knee. Although the ligament can heal, it might re-grow improperly, which could cause your knee to give way.
Does walking help with PCL tears?
Excessive walking during the early stages of recovery can impede your progress and worse knee pain. Applying ice packs to your knee will help reduce swelling.
How can someone who has a PCL injury sleep?
To brace your knee and lessen swelling, elevate your leg with pillows. However, keep your leg slightly above your heart; overdoing it could backfire. Additionally, a knee brace can help keep your knee stable while you sleep, as your doctor has advised.
What are some natural ways to heal a ruptured knee ligament?
The RICE approach (Rest, Ice, Compression, Elevation) is a natural way to treat a torn knee ligament. Physical therapy, painkillers, and mild workouts can also help with healing.
Can someone with a torn PCL flex their knee?
An inability to bend the knee might cause a limp or make it difficult to climb or descend stairs. Weight bearing is difficult. Standing or walking on an injured knee can be challenging or uncomfortable, especially for extended periods of time.
When I have a PCL tear, which exercises should I avoid?
Precautions: For the first six weeks following an injury, avoid knee flexions greater than 90°. To avoid posterior subluxation, an anterior drawer force MUST be used when performing knee flexions larger than 90 degrees. Pain in the posterior knee may indicate that the patient is making too much improvement.
How can I do a home PCL tear test?
“The bent knee test” is another test used to diagnose PCL tears. This entails bending one knee while lying on your back, then applying pressure to the knee while monitoring whether it moves out of its natural position. An excessive amount of movement may indicate a PCL tear.
Is ACL superior to PCL?
Pain, edema, and instability in the knee are the hallmarks of both ACL and PCL injuries. The degree of the injury and the intensity of the symptoms are where they typically diverge. The ACL is more vulnerable to a full tear because it is weaker and smaller than the PCL.
Does non-surgical PCL healing occur?
Treatment Without Surgery
Surgery is not necessary to repair isolated full tear or partial PCL tears. Only a skilled medical professional can ascertain this during an examination. You should be aware of and take into account the immediate and long-term effects of your choices.
With a ruptured PCL, is it still possible to walk?
Your knee might feel better in a few days or weeks if you have a small PCL damage. It may take six months to a year to fully recover from surgery if you have a large PCL tear. You could find it difficult to walk or perform other foot-based tasks during that period.
Is it possible for the posterior cruciate ligament to heal itself?
In sports like baseball, soccer, football, and skiing, PCL injuries are frequent. As long as the knee is protected during the healing process and there are no further knee joint injuries, PCL injuries which are typically partial ligament tears usually heal on their own without producing stability problems.
How much time does it take to heal after an injury to the posterior cruciate ligament?
Depending on the extent of the injury, recovery from a PCL sprain or tear varies. Ten days to two weeks are needed for the healing of mild (Grade 1) sprains. It takes three to four weeks for moderate (Grade 2) sprains to heal completely. When deciding when to resume their sport, athletes should consult with their doctor.
References
- Dhameliya, N. (2023b, October 21). Posterior cruciate ligament injury (PCL), Physiotherapy treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/posterior-cruciate-ligament-injury/
- Dhameliya, N. (2023b, October 21). Posterior cruciate ligament – anatomy, function, injury. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/posterior-cruciate-ligament/
- Posterior cruciate ligament (PCL) injury. (2025, March 19). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21793-pcl-posterior-cruciate-ligament-tears
- What is Posterior Cruciate Ligament(PCL) Injury? Symptoms, Causes, Diagnosis & Physiotherapy Treatment of Posterior Cruciate Ligament(PCL) Injury. . … (n.d.). Cbphysiotherapy. https://cbphysiotherapy.in/condition/posterior-cruciate-ligament-pcl-injury