Plantar Fasciitis
What is Planter Fasciitis?
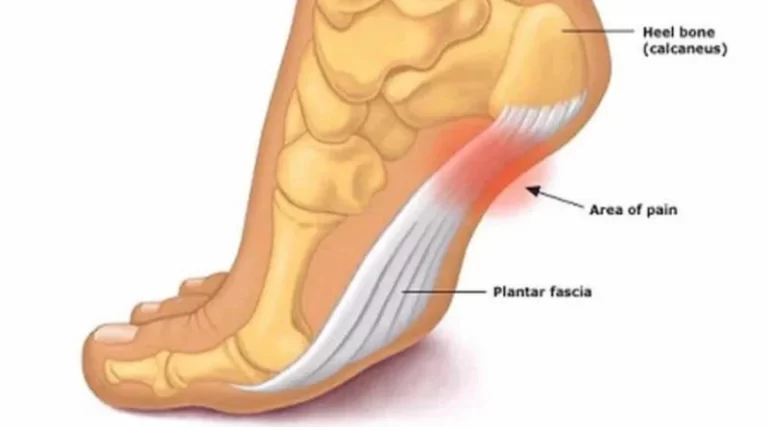
Plantar fasciitis is a common foot condition that causes heel pain at the bottom of the foot. It occurs when the plantar fascia—a thick band of tissue that runs along the sole—becomes inflamed or irritated. This tissue supports the arch of the foot and absorbs shock during movement.
Repeated strain or excessive stress can lead to small tears, resulting in inflammation and discomfort. Plantar fasciitis is often associated with long periods of standing, improper footwear, or activities like running. The pain is typically worse in the morning or after prolonged inactivity.
It causes pain in the heel and ball of the foot, which is often worse during the first few steps of the day or just after rest. Bending the foot and toes up towards the shin also often results in pain.
Anatomy of Plantar Fasciitis
It is a thick white band made up of collagen fibers that are stretched lengthwise. It splits into five distinct bands as it moves toward the toes, ending at the proximal phalanges, or the toe bones that are nearest to the foot. On each proximal phalanx, the deeper layer reaches to include the digital flexor tendons.
Three parts of Plantar Fascia:
- The medial part
- The central part
- The lateral part
Between the comparatively thinner and less noticeable medial and lateral sections lies the biggest and thickest region, which is called the center part.
The plantar fascia of young adults is also connected to the tendinous extension of the lower leg muscles, known as the calf muscle, or the Achilles tendon. It attaches to the posterior surface of the heel bone (calcaneum) after passing behind the ankle.
These two anatomical components are not directly impacted by one another since they have different, specialized attachments on the heel bone. Nonetheless, the Achilles tendon is indirectly tightened by the upward movement of the toes. Plantar fasciitis, a painful inflammation of the plantar fascia, is treated using this link.
Pathophysiology
The medial process of the calcaneal tuberosity gives rise to the thick, fibrous band of connective tissue known as the plantar fascia. It inserts at each proximal phalange as it continues toward the forefoot.
According to current thought, microtears in the plantar fascia develop, indicating a structural breakdown that is not just the result of inflammation. People may be more susceptible to the illness due to the foot’s anatomical makeup.
Any structural irregularity to the foot might result in an asymmetric stress on the plantar fascia, which can cause chronic, recurring injury.
Causes of Plantar Fasciitis:
The most frequent cause of plantar fasciitis is an injury to the foot’s sole ligament from repetitive tension. Inadequate footwear, excessive running or walking, and landing injuries from leaping can all result in strain injuries.
Sign & Symptoms of Plantar Fasciitis:
- severe heel pain
- sneaky heel pain that typically appears right after getting out of bed and makes you want to walk on your toes at first
- worse at the end of the day following extended standing and eased by walking Symptoms are frequently bilateral.
- restricted ankle dorsiflexion owing to a tight Achilles tendon tenderness at the origin of abductor hallucis sensitivity to palpation at the medial tuberosity of the calcaneus pain with palpation rises
- a tiny percentage of individuals with symptoms suggestive of irritation or entrapment of the first branch of the lateral plantar nerve (Baxter’s nerve).
Risk factors
- Age: 40 to 60 years old
- Certain types of exercise: Exercises that put a lot of strain on the heel and attached tissue, like long-distance running, ballistic jumping, ballet dancing, and aerobic dance, can cause plantar fasciitis to develop earlier.
- Foot mechanics: A high arch, flat feet, or even an unusual gait style might change how your weight is distributed when standing and increase strain on your plantar fascia.
- Obesity.
- Occupations that keep you on your feet:- People in manufacturing, education, and other professions who spend most of their working hours on hard surfaces may suffer plantar fascia injury.
Differential Diagnosis:
- Achilles tendonitis
- Morton neuroma
- Calcaneal stress fracture
- Inflammatory arthropathy.
Diagnosis:
Radiographs
- Although infracalcaneal spurring is more commonly an accidental finding and is not necessary for diagnosis, radiographs may reveal it.
- When there are radiographic or clinical indications of rheumatoid arthritis, laboratory testing for rheumatoid factor is advised.
- If there is any indication of a spondyloarthropathy (e.g., ankylosing spondylitis, Reiter disease), laboratory testing for HLA-B27 is advised.
- If radiographs are not definitive in the diagnosis of stress fractures or if the patient is not improving with conservative therapy, technetium bone scans may be recommended.
- When heel pain is resistant (pain persists for more than a year) or when soft tissue or osseous masses are palpable or visible in previous imaging examinations, an MRI is advised.
- For the identical indications as MRI, ultrasound is a newer research that may be utilized instead. In patients with plantar fasciitis, ultrasound testing shows a thickness of the plantar fascia of at least 4 mm. Enthesopathy and hypoechogenicity have also been shown by ultrasound studies.
Treatment of Plantar Fascitis:
Medical Treatment
- Pain relievers, primarily NSAIDs, such as Aleve (naproxen) and Advil or Motrin (ibuprofen), can help lessen the pain and swelling associated with plantar fasciitis.
- Side effects: especially if used for an extended length of time. The most prevalent problems are related to the digestive system, such as nausea and heartburn. Hypertension, liver or renal damage, and allergic responses are less frequent but nevertheless dangerous adverse effects.
- For severe pain and inflammation that do not improve with nonsteroidal medicine, cortisone injections are used for plantar fasciitis.
adverse effect: The fat pad protecting the heel bone may decrease or the plantar fascia may tear as a result of repeated injections.
Surgical Treatment
- As a last option, plantar fasciotomy is frequently used after six months of conservative therapy has not resolved the problem. There are endoscopic and less invasive methods for plantar fasciotomy, but they need to be performed by a professional with experience using specific equipment.
- These surgical methods are not widely available at this time. According to a 2012 research, 76% of patients who had endoscopic plantar
- Fasciotomy resulted in few complications and total symptom alleviation. There is no evidence that removing the heel spur during a plantar fasciotomy improves the surgical result.
- There are several causes of plantar heel pain, and in certain situations, a lateral plantar nerve branch release may be carried out in addition to a plantar fasciotomy. Plantar fasciotomy may result in nerve damage, instability of the foot’s medial longitudinal arch, calcaneus fracture, extended recuperation period, infection, rupture of the plantar fascia, and inability to relieve pain. Recently, a different surgical strategy for treating plantar fasciitis that is resistant to therapy has been suggested: coagulation surgery.
Physical therapy Treatment
Ice is a quick and easy way to lessen pain and swelling. During the first phase, or if you feel that your injury is heated or hot, please apply for 20 to 30 minutes every two to four hours. You may use a frozen water bottle as an ice foot roller and get a little massage for your plantar fascia at the same time.
Treatment Approaches for Plantar Fasciitis:
- Iontophoresis
- Ultrasound therapy
- Deep friction massage
- Contrast bath
- TENS
- Shoe wear Modification (Running shoes): Running shoe modifications include a flared, sturdy heel to aid with heel stability management. The heel is softly cushioned and raised 12–15 mm above the sole. Achilles pad that is well-molded. Steer clear of stiff leather dress shoes since they put more strain on the Achilles tendon.
- Viscoheels: Cushioned Heel Inserts for Plantar Fasciitis Treatment. Soft cushions are inserted and removed from the patient’s footwear. Eventually, patients with aberrant lower extremity biomechanics, such as pes cavus or pes planus, may find relief by wearing specially cushioned orthotics.
- Taping for plantar fasciitis: Taping is another helpful pain-reduction method. By lowering the strain on your plantar fascia, this method lessens your pain. You will get immediate pain reduction after using this tape procedure.
Exercise of Plantar Fascitis:
- Standing calf stretch:

As though you were pigeon-toed, turn your rear foot slightly inward. Go back to where you were before. Do this three times. Perform this workout many times per day.
- Seated plantar fascia stretch:

Cross your wounded foot over your other leg’s knee while seated in a chair. Hold for 15 seconds, then do it three times.
- Plantar fascia massage:
Cross your wounded foot over your other leg’s knee while seated in a chair. Massage the bottom of your foot with your other hand, working your way from the heel to the toes. Spend three to five minutes doing this. Begin slowly. As your tolerance for pressure increases, apply additional pressure to the bottom of your foot.

- Achilles stretch:
On a stair, stand with one foot on the ball. Using your heel, reach toward the step below until your foot’s arch feels stretched. After 15 to 30 seconds of holding this position, release your tension. Do this three times.
- Towel pickup:
Let go. Do this ten to twenty times. Once this becomes simple, place a book or small weight on the towel to increase the resistance.
- Heel raise:
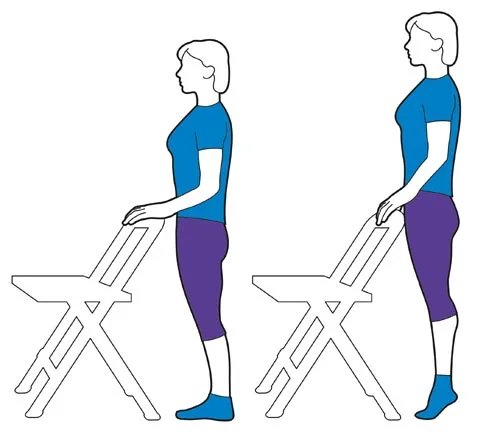
Get up on your toes and hold for five seconds while using the chair or counter as support. Then, without clinging to the support, gently descend. (Retaining the assistance if necessary is OK.) Try doing this exercise while standing just on the affected leg if it starts to feel less uncomfortable. Do this fifteen times. Perform two sets of fifteen.
How to prevent Plantar Fascitis?
- Rest: Take a break from your routine if you begin to experience foot pain.
- Ice and elevation: To lessen swelling, it’s crucial to freeze your foot often and elevate it if you continue to perform activities that put weight on it, such as walking.
- Don’t try to ignore the pain.
- Avoid going barefoot.
Complications
Chronic heel pain that interferes with daily activities can be caused by ignoring plantar fasciitis. In order to prevent plantar fasciitis pain, which can result in issues with your feet, knees, hips, or back, you need probably alter the way you walk.
Prognosis
As soon as you begin treating your plantar fasciitis symptoms, you should see an improvement. However, it may take a few weeks to many months for your plantar fascia to recover.
Try your previous at-home remedies if you feel better but your symptoms come back. If your symptoms seem different or worse than they used to be, speak with your healthcare professional.
Conclusion
If you experience heel or foot pain that doesn’t go away after a week, consult a healthcare professional. They will assist you in locating at-home remedies to lessen your foot’s pain and swelling.
Being informed that you must miss a week or more of your favorite sport or hobby is always inconvenient. However, take your time returning to the court or field. If you overstress your foot before it heals, you might re-injure your plantar fascia.
FAQs
What is plantar fasciitis’ primary cause?
When the fascia, a thick band of tissue on the bottom of your foot, is overstretched or under severe strain from recurrent tension from activities like standing or jogging, plantar fasciitis develops. Significant weight gain, especially during pregnancy, may also result in it.
Is plantar fasciitis reversible?
With conservative therapy, which includes stretching, icing the affected region, and avoiding or reducing uncomfortable activities, the majority of patients with plantar fasciitis heal in a few months.
Does walking help people with plantar fasciitis?
Walking may actually exacerbate plantar fascia inflammation, necessitating a longer course of therapy. Although walking by itself won’t cause the ligament to worsen, choosing inappropriate footwear or overexerting oneself might cause plantar fasciitis to worsen.
How bad is plantar fasciitis?
In most cases, plantar fasciitis is treatable and not a chronic or permanent ailment. After a few months of conservative therapy, the majority of patients fully recover. Conservative treatment methods are effective in many plantar fasciitis instances.
How can someone who has plantar fasciitis sleep?
Avoid sleeping in a prone posture (face or belly down) if you have plantar fasciitis in order to avoid contracturing your calf muscle and Achilles tendon. Rather, choose to sleep on your side or back, with a cushion between your legs or beneath your knees, accordingly.
Is it natural for plantar fasciitis to heal?
The good news is that basic home remedies may typically be used to cure this ailment. Surgery is only recommended for around 5% of patients with plantar fasciitis, and only after conservative measures have failed.
How is plantar fasciitis massaged?
Pull each toe gently away from the foot, beginning with the big toe. Finally, give the heel a last circular massage.
Can someone with plantar fasciitis lead a normal life?
You frequently feel pain after working out, but rarely while doing it. In order to prevent hip or knee issues from developing as a result of changing your stride due to pain, it is imperative that you get treatment for plantar fasciitis.
Does plantar fasciitis last a lifetime?
Although it normally goes away on its own, plantar fasciitis may be excruciating. In most cases, it might take up to two years to settle. A tiny percentage of individuals with really severe plantar fasciitis may experience the ailment for years at a time.
Why did I develop plantar fasciitis so quickly?
People between the ages of 40 and 60 are most likely to suffer from plantar fasciitis. specific forms of physical activity. Plantar fasciitis can develop as a result of activities that put a lot of strain on your heel and surrounding tissue, such as aerobic dancing, ballet dancing, and long-distance jogging.
How can plantar fasciitis be verified?
In order to diagnose plantar fasciitis, the clinical history and physical examination are crucial. Morning stiffness and increased pain while bending the foot upward (dorsiflexion), which happens during activities like standing on your toes or climbing stairs, are the most significant aspects of the clinical history.
How can plantar fasciitis be healed the quickest?
In order to cure plantar fasciitis on your own, you should stretch your plantar fascia many times a day, ice your foot, take NSAIDs, rest your foot, use orthotics to support your arch and heel, and limit the amount of time you spend doing painful activities like jogging or walking.
Can plantar fasciitis be alleviated by drinking water?
Plantar fasciitis. The inflammation of the band of tissue that connects the heel bone to the toes is known as plantar fasciitis. Water consumption can help control the pain and inflammation associated with plantar fasciitis. pain in the nerves.
Does plantar fasciitis benefit from heat?
Since heat doesn’t reduce pain and can exacerbate swelling, it is generally not advised to utilize heat therapy alone to treat plantar fasciitis. It can, however, be used in conjunction with cold and ice treatments; this is known as contrast therapy.
What is frequently confused with plantar fasciitis?
Summary: Compression of the posterior tibial nerve during its passage through the tarsal tunnel, which is situated close to the inner ankle, results in tarsal tunnel syndrome. This disorder can cause heel and arch pain and sensory abnormalities, which frequently resemble plantar fasciitis.
Who is most affected by plantar fasciitis?
About 10% of runner-related injuries and 11% to 15% of all foot complaints that call for expert medical attention are caused by this ailment. Approximately 10% of the general population suffers from plantar fasciitis, and 83% of those affected are active, working people between the ages of 25 and 65.
References
- Plantar fasciitis – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/plantar-fasciitis/symptoms-causes/syc-20354846
- Plantar Fasciitis. (2024, September 9). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/14709-plantar-fasciitis
- Dhameliya, N. (2022d, August 5). Plantar Fasciitis – Cause, Symptoms, Treatment, Exercise. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/plantar-fasciitis/






4 Comments