Perthes Disease
What is a Perthes Disease?
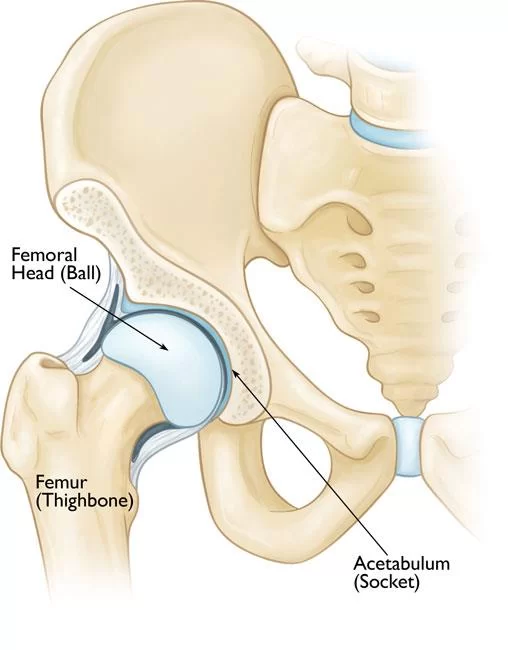
Perthes disease is a rare childhood condition affecting the hip joint, specifically the femoral head, which is the rounded end of the thigh bone. It occurs when the blood supply to this part of the bone is temporarily disrupted, causing the bone tissue to die, a process known as avascular necrosis.
Perthes is actually a multi-stage, intricate process that might take years to fully develop, even though the word “disease” is still often used. The femur’s head gradually regains its blood supply, and the bone starts to regenerate.
The goal of Perthes treatment is to encourage the bone to reshape into a more rounded form that yet allows it to fit into the hip joint’s socket. By doing this, hip issues in adulthood can be avoided and the hip joint can move more naturally. In most circumstances, children with Perthes have an excellent long-term prognosis. Most youngsters return to their regular activities without significant limits after receiving therapy for 18 months to 2 years.
- The illness affects kids between the ages of two and fourteen. Both early osteoarthritis and lifelong deformity may result from the illness. Though it affects males five times more frequently than girls, it is most likely to cause more serious bone injury in the former. 10% to 15% of instances involve damage to both hips.
- The dead bone starts to be removed by new blood vessels as the healing process progresses.
- As a result, the femoral head becomes weaker and bone mass decreases. As new bone and tissue replace the necrotic bone, it may also result in bone deformities.
- The ball experiences a fracture of the supporting bone as bone death manifests. This fracture marks the beginning of the body’s reabsorption of bone.
Pathology
The femoral head weakens and bone mass is lost as a result of new blood vessels penetrating the dead bone and eliminating the necrotic bone over time.
Adults who have osteoarthritis are more likely to have a persistent malformation of the femoral head as a result of Perthes.
Causes of Perthes disease
- Although LCPD is an idiopathic condition, since its discovery more than a century ago, several ideas on its underlying causes from congenital to environmental, from traumatic to socioeconomic have been put up. Abnormal bone development patterns, fibrinolysis, and thrombosis have all been linked to LCPD.
- Additionally, it’s linked to anomalies in the Insulin-like Growth Factor-1 Pathway, recurrent microtrauma, mechanical overloading caused by the child’s hyperactivity, extremely low birth weight, or short stature at birth.
- A type II collagen mutation is one genetic cause that some research proposes, whereas other studies indicate mother smoking during pregnancy along with other prenatal and postnatal risk factors.
- It’s possible that any or all of the previously listed reasons are necessary for LCPD.
Clinical Features of Perthes Disease
- Limp: These youngsters usually have a psoatic limp as a result of psoas major weakening. The limp gets worse during physical activity and gets better after taking breaks. Late in the day, after extended walking, the limp becomes more apparent.
- Pain: During the acute phases, the kid frequently experiences pain. Usually, the pain gets worse later in the day and when one is more active. Pains during the night are common.
- ROM: The child’s active ranges of motion in abduction and extension will be reduced.
- Unusual high activity level: Children with LCPD typically exhibit high levels of physical activity, and a notable proportion of them suffer from attention deficit disorder or real hyperactivity.
- Abnormal growth patterns: In relation to the upper arm, the hands and forearms are comparatively short. In relation to the tibia, the feet are rather short.
Stages of Perthes disease
Early in the 20th century, Waldenström divided the progression of LCPD into four stages. Joseph et al. then further divided each of the first three stages into early (A) and late (B) substages to further categorize the disease’s evolution and pinpoint specific changes that occurred at different points.
Stage I: Initial stage or avascular necrosis (± 1 year)
IA: Early
- Head of the femur radiolucency.
IB: Late
- flattening of the femoral head’s summit
IIA: Early
- There is early fragmentation.
IIB: Late
- There is more fragmentation when a dead bone is resorbed.
- The femoral head has an uneven contour and seems more flattened.
- might seem to subluxate.
- Reossification stage III (two to three years)
IIIA: Early
- Along the femoral head’s outside perimeter, new porous bone grows.
- Increases in density IIIB: Late
- Towards the center, the freshly produced bone progressively fills up.
- The femoral head’s contours and form become more distinct.
Stage IV: Healed
- The final shape (the extent of flattening or deformity) and fit of the femoral head into the socket at this point largely dictate the long-term outcome.
Diagnosis of Perthes disease
- MRIs are typically ordered to confirm the diagnosis, however, x-rays can also be used to see where the femoral head is positioned.
- An imaging method that can forecast the outcome in the early stage of the illness, before considerable deformity has arisen, is preferable because the outcome of LCPD is varied.
- At the early stages of LCPD, there was no association between the degree of femoral head involvement seen by non-contrast and contrast MRI, suggesting that they are evaluating two distinct aspects of the disease process. Contrast MRI gave a more accurate picture of the affected region during the early stages of LCPD.
- Novel three-dimensional (3D) magnetic resonance imaging (MRI) reconstruction and volume-based analysis can be utilized to measure femoral head deformity in individuals with LCPD.
- The femoral head distortion in LCPD may be accurately quantified and modest alterations (less than 10 percent) can be shown using the 3D MRI volume ratio approach. This technique might be helpful in assessing how a therapy affects the morphology of the femur head.
Treatment
Medical Treatment of Perthes Disease
- The treatment plan is a contentious one. The prognosis for the condition must be clearly understood before determining if surgery is required.
- Psychological aspects are also taken into account. Compared to their counterparts, those with a history of LCPD had a 1.5-fold increased risk of developing attention deficit problems.
Physical therapy management of Perthes disease
- Regarding the potential advantages of physical therapy for individuals with learning disabilities or the optimal stage at which to use it, there is a lack of agreement.
- While some studies discuss physical therapy as a pre-and/or postoperative intervention, others view it as a conservative measure used in conjunction with other therapies including plaster casts, orthoses, and skeletal traction.
- Children with a mild course of the condition received physical therapy in trials comparing various therapies. The following were the patients’ characteristics:
- Children in Caterall groups 1 or 2 who have less than 50% femoral head necrosis
- Children under six years old with excellent (>80%) femoral head covering but more than 50% femoral head necrosis
- Herring class A or B
- Type A Salter Thompson
- Physical therapy can enhance muscle strength, articular dysfunction, and articular range of motion in people with mild cases. Among the physical therapeutic interventions were passive mobilizations to extend the hip’s muscle.
- Exercises including straight leg raises are useful for strengthening the hip muscles involved in flexion, extension, abduction, and adduction.
- After eight sessions, they moved on to isotonic exercises from isometric ones.
Conservative management of Perthes diseases:
Active Assisted Hip Knee Flexion
- It has been demonstrated that physical therapy therapies increase this patient population’s strength and range of motion.
- Compared to people who get either a home exercise program or no training at all, individuals who engage in supervised clinic visits show better progress in muscular strength, functional mobility, gait speed, and quality of exercise performance.
- People who get encouraging comments from their physical therapist on a daily basis are more likely to stick with an additional at-home exercise regimen.
Improve ROM in Perthes disease:
- Moving ROM
- To preserve a newly achieved range of motion, do AROM and AAROM (active assistive range of motion) after passive stretching.
- Increase your strength
- Start with isometric exercise, work your way up to isotonic activities in a posture that lessens your gravity, and then go on to isotonic workouts that defy gravity. Both concentric and eccentric contractions are acceptable.
- Start each exercise with two sets of ten to fifteen repetitions, then proceed to three sets of the same exercise.
- When a kid has LCPD, it is best to prevent the hip overloading pattern.
- When LCPD first manifests between the ages of 6 and 8 with Herring B involvement, brace-based non-surgical therapy is a dependable substitute for surgical treatment. They were unable to determine, nevertheless, if the positive outcomes were due to the brace or to the patients’ favorable prognosis.
Post-operative management of Perthes disease
The many phases of rehabilitation are mentioned while describing the rehabilitation.
Initial Phase (0-2 weeks post-cast removal)
Goals of the Initial Phase
- Minimize pain
- hot pack to relieve pain
- Cryotherapy
- Medication for pain
- Moving ROM
- After passive stretching, perform AAROM and AROM to keep the newly acquired ROM.
- Boost your strength in the knee, ankle, and hip flexion, abduction, and extension.
- Start with hip-level isometric exercises and work your way up to isotonic workouts while reducing your gravitational force.
- Start with isometric workouts for the knee and ankle, then go on to isotonic exercises while reducing your gravitational force. Eventually, you can advance to isotonic exercises that defy gravity.
- Start each exercise with two sets of ten to fifteen repetitions, then work your way up to three sets of each exercise.
- improve functional mobility and gait
- Observe the WB status.
- ADL’s Gait training with the proper assistive device, emphasizing safety and independence, includes transfer training and bed mobility to optimize independence.
- enhancing the integrity of the skin
- If possible, a warm bath to restore skin integrity after cast removal in a home setting.
- With your arms immersed, start slowly strolling in the chest-deep pool of water.
- Enhancing the Integrity of the Skin
- Continue massaging and desensitizing scars.
- Swimming is allowed if the referring physician gives the okay.
Advanced Phase(6-12 weeks post-cast removal) :
Goals
- Reduce pain (refer to “initial phase”)
- Isotonic hip, knee, and ankle movements, involving concentric and eccentric contractions, performed in postures that reduce gravity and defy gravity
- Start functional dynamic single-limb movements supported by the upper extremities (e.g. step-ups, side steps)
- If your WB status permits, go to single-limb closed-chain exercises with minimal resistance after finishing double-limb closed-chain exercises with resistance.
- Using a stationary bike while upright or reclined and maintaining a hip flexion angle of less than ninety degrees
- Use a step-to-pattern to independently negotiate stairs while receiving upper extremity (UE) help.
- Enhance balance to at least 69% of the maximum Pediatric Balance Score (39/56) or to the unaffected side’s single-limb stance.
- enhancing functional mobility and gait.
FAQs
What are Perthes disease exercises?
Activities to improve balance and coordination. How to incorporate regular low-impact activities into your child’s routine, such as walking and stationary cycling.
Is Perthes illness inherited?
Sometimes mutations in the COL2A1 gene cause the characteristic bone abnormalities associated with Legg-Calvé-Perthes disease.
What should you stay away from when it comes to Perthes disease?
Runs, jumps, and other high-impact sports that might hasten hip deterioration should be avoided by kids with Perthes disease. crutches. Your youngster may occasionally need to refrain from putting weight on the injured hip.
Perthes disease affects which gender?
The majority of individuals with Legg-Calve-Perthes disease are men; the male to female ratio ranges from 4:1 to 5:1. Ten to twenty percent of afflicted instances are bilateral. Bilateral cases are typically asymmetrical and identified at separate phases of the illness.
For kids with Perthes disease, what kinds of activities are beneficial?
While riding and swimming are still permitted, the majority of doctors advise limiting some activities, such as impact sports like running and leaping. Physical therapy is occasionally advised to reduce muscular weakness and assist with stretching.
References
- Physiotherapist, B. (2023c, December 13). Perthes Disease: Cause, Symptoms, Physiotherapy management. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/perthes-dieases-and-physiotherapy-management/#google_vignette
- Legg-Calve-Perthes Disease. (2024, September 10). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/legg-calve-perthes-disease



One Comment