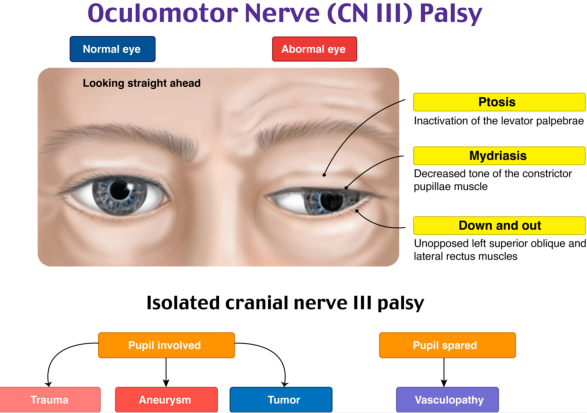
Oculomotor Nerve Palsy
What is an Oculomotor Nerve Palsy?
An eye condition called oculomotor nerve palsy or oculomotor neuropathy is caused by injury to the third cranial nerve or one of its branches. As the name indicates, the oculomotor nerve provides the majority of the muscles regulating eye movements (four of the six extraocular muscles, excluding only the lateral rectus and superior oblique).
The eye cannot move normally if damage is done to this nerve. The parasympathetic fibers that innervate the muscles responsible for pupil constriction (sphincter pupillae) accompany the nerve, which also feeds the levator palpebrae superioris, the muscle that lifts the top eyelid.
Patients often have double vision (diplopia) due to strabismus, which is caused by severe limits in eye movement that make it difficult for them to maintain proper eye alignment when looking straight ahead.
What is The Oculomotor Nerve?
One of the key nerves you utilize to control eye movements is the oculomotor nerve. Its branches attach to muscles on both sides of your eyes, sending movement signals from your brain to those muscles. Although the name suggests that it is for a single nerve, it is a matched set, one for each eyeball.
The third of the 12 cranial nerve pairs is the oculomotor pair, so named because it attaches directly to your brain (pronounced “OCK-yoo-lo-mo-tor”). Experts also refer to this nerve by the Roman numeral combination “CN III,” which is a combination of letters.
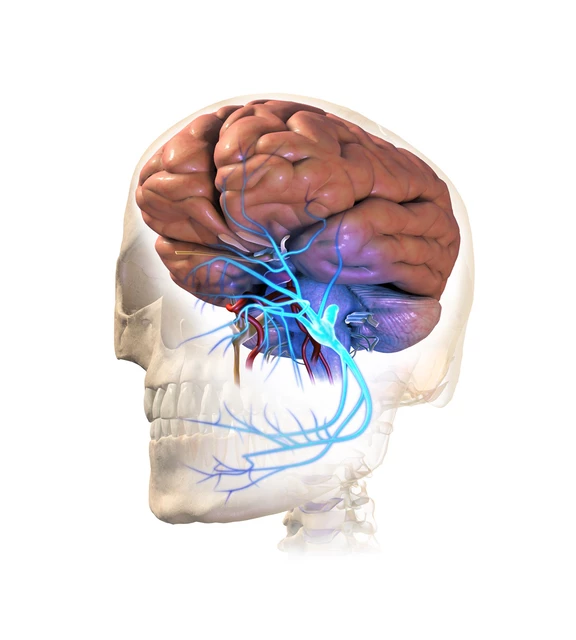
Anatomy of Oculomotor Nerve
The oculomotor nucleus, which is situated ventral to the cerebral aqueduct in the brainstem’s midbrain, is the oculomotor nerve’s source. The anterior portion of the midbrain is where it arises, and it passes superiorly to the superior cerebellar artery and inferiorly to the posterior cerebral artery.
The nerve enters the cavernous sinus lateral aspect after passing through the dura mater. The internal carotid plexus sends sympathetic branches to the cavernous sinus. These fibers only move inside the oculomotor nerve’s sheath; they do not merge with it.
Through the superior orbital fissure, the nerve exits the cranial cavity. It splits into superior and inferior branches at this point:
- The superior branch supplies motor innervation to the levator palpabrae superioris and superior rectus. The superior tarsal muscle is innervated by sympathetic fibers that travel with the superior branch.
- The inferior branch supplies motor innervation to the inferior rectus, inferior oblique, and medial rectus. Additionally provides the ciliary ganglion, which in turn innervates the ciliary muscles and sphincter pupillae, with pre-ganglionic parasympathetic fibers.
Function Oculomotor Nerve
Motor Function
Many of the extraocular muscles are innervated by the oculomotor nerve. These muscles are responsible for moving the eyeball and top eyelid.
Superior Branch
- The superior rectus raises the eye.
- The upper eyelid is raised by the levator palpabrae superioris.
- In addition, the superior branch of the oculomotor nerve is carried by sympathetic fibers. Once the levator palpabrae superioris has raised the eyelid, it innervates the superior tarsal muscle, which functions to maintain it high.
Inferior Branches:
- The inferior rectus, which depresses the eyeball, is the inferior branch.
- The medial rectus adducts the eyeball.
- The inferior oblique raises abducts, and rotates the eyeball laterally.
Parasympathetic Mechanisms
- The oculomotor nerve supplies parasympathetic innervation to two structures in the eye:
- The pupil’s sphincter pupillae constricts, letting less light penetrate the eye.
- When the ciliary muscles contract, the lens becomes more spherical and better suited for short-range vision.
- The inferior branch of the oculomotor nerve is where the pre-ganglionic parasympathetic fibers travel. They split off and synapse in the ciliary ganglion within the orbit. The short ciliary nerves transport the post-ganglionic fibers to the eye.
The role of oculomotor nerves in other abilities
Your oculomotor nerves must function in perfect harmony with several other systems since vision is a vital component of many skills and functions. When they do, you are capable of the following:
- Make accommodations. This is the capacity to keep your attention fixed on an object as it moves in your direction or away from it.
- Scanning the movements of the eyes. Short saccades back-and-forth eye movements that aid in field-of-view scanning, are pronounced “sa-KODZ.”
- Fluid chase. This enables your eyes to follow moving objects with ease.
- Reflex vestibulo-ocular. This reaction maintains your eye and head muscles still during sudden movements or changes in direction by utilizing your vestibular system, which regulates balance, in conjunction with head and eye movements.
What is the Oculomotor Nerve Palsy?
- Oculomotor nerve palsy is a type of nerve condition that can impair your vision. Double vision and trouble combining both eyes may result from it. This illness is caused by a weakening of the oculomotor nerves, which impair control over key eye muscles.
- There are cases of oculomotor nerve motor palsy in newborns. In other cases, a sickness or injury is the cause of the disorder. Depending on the underlying problem, treatment options may include vision rehabilitation, corrective lenses, or surgery.
Clinical Significance for Oculomotor Nerve Palsy
- The levator palpabrae superioris is paralyzed, and the orbicularis oculi muscle contracts without resistance, resulting in ptosis (drooping upper eyelid) in cases of oculomotor nerve palsy.
- Paralysis of the superior, inferior, medial, and inferior rectus, as well as the inferior oblique (and consequently the unopposed activity of the lateral rectus and superior oblique), is responsible for the “down and out” position of the eye during rest.
- Elevate, depress, or adduct the eye as needed by the patient.
- A dilated pupil results from the dilator pupillae muscle acting without resistance.
Conditions that may impact the oculomotor nerve
The same problems that affect other nerves can also affect your oculomotor nerve. Additionally, this nerve might be impacted by specific brain diseases because it passes through different parts of the brain.
Oculomotor nerve palsy (sometimes “third nerve” substitutes for “oculomotor”) or dysfunction is the term used to describe when the oculomotor nerve isn’t functioning properly. The oculomotor nerve can malfunction for a variety of reasons. As an example, consider:
- Physiological conditions. High blood pressure and type 2 diabetes can obstruct blood flow and result in ischemia, or “iss-KEE-me-uh,” which is a malfunctioning and dying nerve. This may result in a lifelong loss of control of the oculomotor nerve’s associated muscles. Similar disturbances in circulation can also be brought on by hemorrhages, or bleeding.
- Accidents. The oculomotor nerve can be damaged by trauma to the head, face, or brain, which prevents it from transmitting signals properly.
- Infections. Pathogens such as viruses and bacteria can induce neurological diseases. HIV and the germs that cause Lyme disease are two examples.
- Disorders of the nervous system and brain. Your oculomotor nerve may be impacted by conditions that impair brain function. These include less serious illnesses like strokes and transient ischemic attacks (TIAs) as well as more serious ones like migraines and seizures.
- Inflammation. The oculomotor nerve may be compressed by swelling from inflammatory tissues, impairing its ability to transmit signals. Inflammatory diseases, including autoimmune diseases where your immune system damages nerve tissues, can be caused by a variety of circumstances. An example would be a disease such as multiple sclerosis (MS).
- Tumors, such as benign growths and malignancy. These have the potential to squeeze the oculomotor nerve, harming it and interfering with signal transmission.
- Birth defects. These are the conditions you are born with. This usually indicates that the oculomotor nerve’s ability to transmit signals was disrupted due to improper development of the nerve or a structure around it. A few of these might be manageable.
- Idiopathic reasons. Experts may be unable to determine the cause of oculomotor nerve problems. “Idiopathic” refers to a situation in which the cause is uncertain.
Symptoms of Oculomotor Nerve
The intensity and number of damaged muscles can impact the symptoms of oculomotor nerve palsy. The majority of symptoms are also signs of other nerve or ocular health issues.
However, if you experience any symptoms that impair your vision, it’s always a good idea to see a doctor. Many disorders that affect your vision can get worse, so getting treatment as soon as possible can be crucial.
The following are typical signs of ocular nerve palsy:
- Double vision. Oculomotor nerve palsy impairs the function of your eyes as a unit. Double vision can result from improper eye coordination.
- Crossed eyes and a loss of focus. Oculomotor nerve palsy can make it difficult to concentrate your eyes or regulate the direction of your eye movement. People who suffer from this illness frequently have trouble shifting their eyes simultaneously in the same direction.
- Unusual head movements. Oculomotor nerve palsy patients frequently lift their heads to make up for their weaker eye muscles. This may result in uncomfortable or distracting head movements and postures.
Diagnosis for the Oculomotor nerve palsy
Third cranial nerve palsy may require imaging, laboratory testing, a thorough neurological examination, and an eye exam. A physician may request imaging studies if the pupil is affected to identify the source of compression to the CN III’s outer nerve fibers. Among these tests are:
- MRI stands for magnetic resonance imaging, which creates three-dimensional brain scans.
- Computed tomography angiography, or CT angiography, generates pictures of blood arteries and tissues when an aneurysm is suspected.
If the pupil is not affected, the following tests could be prescribed by a physician to rule out the presence of an inflammatory disease or an underlying condition like diabetes or hypertension:
HbA1C: Determines the three-month average blood sugar levels.
The Complete Blood Count, or CBC, offers a broad assessment of general health.
Erythrocyte sedimentation rate, or ESR, is a measure of the body’s inflammation.
BP stands for blood pressure measurement.
Treatment for the Oculomotor nerve palsy
- The underlying cause and severity of oculomotor nerve palsy will determine how the condition is treated. It is crucial to evaluate the patient’s systemic involvement before choosing a course of treatment. This can be done by conducting a thorough investigation that calls for a multidisciplinary team that includes an oncologist, radiologist, endocrinologist, and/or neurologist. The choice of treatment can be made after the cause has been determined.
Conservative Treatment
Treatment for paralysis that occurs during the acute phase (the first six months) needs to be conservative and involve a range of therapeutic approaches.
- Observation.
- Closing one’s eyes (ideally alternately) will prevent double vision.
- Anti-inflammatory non-steroid medications if they hurt.
- Injection of botulinum toxin to reduce antagonistic muscle contraction (the muscle that acts in opposition to the paralyzed muscle).
We discuss the chronic phase when the clinical picture has been present for six months. Depending on the severity of the patient’s residual deviation, there are various options if the patient makes a partial recovery.
- Glasses with permanent prisms. To avoid double vision, prisms are added to your glasses if the divergence is slight. Prism glasses can be worn regularly to help with double vision.
- Clear lenses or adhesive patches for the eyes. Managing double vision can be aided by these visual aids. These could be worn for six months to a year. This may be sufficient in certain cases for the oculomotor nerve palsy to recover naturally.
- Vision therapy. A technique called vision therapy helps build strengthened eye muscles to help lessen or perhaps eliminate symptoms.
Surgery is recommended if the deviation is too significant to be tolerated by the prism. The injured muscle will determine which technique is best.
Surgical Treatment
- Surgery to release the nerve’s pressure. When a patient has a tumor, aneurysm, or noncancerous development, doctors frequently operate.
- Surgery on the muscles of the eyes. The surgical treatment of strabismus might help straighten the eyes.
The injured muscle will determine which technique is best. Since there isn’t a single method that works for every situation, each patient’s procedure will be unique. The goal is to achieve the greatest feasible field of vision in both eyes, eliminate diplopia, treat torticollis, and maximize eye parallelism in the primary gaze position (looking from the right to the front). It’s crucial to keep in mind that surgery alone cannot restore function to a paralyzed nerve and that multiple procedures may occasionally be required.
Prognosis
It’s hard to predict how long healing will take for oculomotor nerve palsy because there are so many possible reasons. After a few months, many people do fully recover from this disease; however, your success will be dependent upon the severity and the presence of any underlying conditions.
For instance, a person with diabetes may require medical attention to treat their illness before their oculomotor nerve palsy improves, making recovery more challenging. On the other hand, a patient recuperating from an accident can benefit from vision treatment after a month or two.
Prevention for Oculomotor Nerve
Taking good care of your oculomotor nerves is similar to taking care of your entire body. Among the actions you can do are:
- Get annual physicals and routine eye exams; these can frequently detect health and vision issues before symptoms appear.
- Give up using nicotine-containing products, such as smoking cigarettes, smoking, and smokeless tobacco, or refrain from starting them. Request support in quitting from your provider.
- To prevent head injuries, wear safety equipment like seatbelts and helmets.
- Control long-term health issues such as high blood pressure, Type 2 diabetes, etc.
Summary
The oculomotor nerve pair is responsible for transmitting signals from your brain to the muscles surrounding your eyes. It is simple to ignore when the oculomotor nerve functions properly. However, it makes sense to experience uncertainty or fear when it malfunctions.
Speak with an eye care professional if you believe you may have issues with the oculomotor nerve or eye movement control. They can check for conditions that might be causing your symptoms, do tests, and recommend a course of action.
FAQs
What signs and symptoms are present in oculomotor nerve palsy?
When the unaffected eye looks straight ahead, the affected eye turns slightly outward and downward, resulting in double vision. When gazing inward, the damaged eye may turn very slowly and move just to the middle.
What is the course of third nerve palsy?
Pupil: The paralysis of the sphincter pupillae causes the pupil to become fixed and dilated in compressive third-nerve palsy. Accommodation loss is also a result of paralysis of the ciliary muscles. At the same time, there is no loss of accommodation in ischemic lesions because the pupil is spared.
What is the most frequent reason for paralysis of the oculomotor nerve?
Microvascular infarction, which is pupil-sparing and results from disorders such as diabetes mellitus, hypertension, atherosclerosis, and collagen vascular disease, is the most common cause of solitary oculomotor nerve palsy.
How is oculomotor nerve palsy diagnosed?
Many etiologies can have acquired oculomotor nerve palsy as a subsequent condition. Nonetheless, if cerebral pathology is suspected, neuroimaging is typically conducted. When a cognizant patient presents with ptosis, mydriasis, and ophthalmoplegia, it is necessary to rule out compressive causes such as a cerebral aneurysm.
How can third nerve palsy be managed?
There are nonsurgical and surgical options for treatment. Surgery continues to be the primary form of treatment because nonsurgical methods are not very helpful. Different surgical techniques are used for third nerve palsy, whether total or partial. Resection of the rectum through a supramaximal retraction is one surgical procedure for full third nerve palsy.
What is the duration of third cranial nerve palsy?
Maximum improvement can happen up to 18 months following the onset of symptoms, however, it usually happens within the first six months. It is doubtful that congenital third nerve palsy will go away on its own.
References
- Rubin, M. (2023, November 10). Third cranial nerve (Oculomotor nerve) palsy. MSD Manual Consumer Version. https://www.msdmanuals.com/en-in/home/brain,-spinal-cord,-and-nerve-disorders/cranial-nerve-disorders/third-cranial-nerve-oculomotor-nerve-palsy
- The causes of acquired 3rd nerve palsy Mayo Clinic. (2020, April 23). https://www.mayoclinic.org/medical-professionals/ophthalmology/news/the-causes-of-acquired-third-nerve-palsy/mac-20431238
- Third-Nerve Palsy. (2018, January 22). American Academy of Ophthalmology. https://www.aao.org/education/disease-review/third-nerve-palsy-2
- Ms, S. K. O. (2023, April 11). Third nerve palsy (oculomotor nerve palsy). All About Vision. https://www.allaboutvision.com/conditions/related/third-nerve-palsy/
- Srakocic, S. (2022, September 16). What is oculomotor nerve palsy? Healthline. https://www.healthline.com/health/oculomotor-nerve-palsy
- Professional, C. C. M. (n.d.-g). Oculomotor nerve (CN III). Cleveland Clinic. https://my.clevelandclinic.org/health/body/21708-oculomotor-nerve