Obturator Nerve
Introduction
The obturator nerve is a peripheral nerve that arises from the lumbar plexus (L2-L4) and primarily supplies the medial thigh. It provides motor innervation to the adductor muscles (adductor longus, adductor brevis, adductor magnus, gracilis, and obturator externus) and sensory innervation to the skin of the medial thigh.
In several pathologic disorders and operations affecting the hip and knee, the obturator nerve has clinical significance. Additionally, the obturator nerve is a crucial anatomic feature in several clinical scenarios due to its origin in the lumbar plexus and its position in the pelvis and upper thigh.
Structure
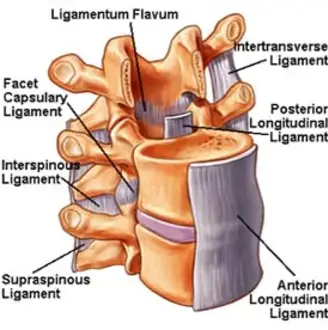
The second through fourth lumbar plexus nerve roots give birth to the obturator nerve. The obturator nerve, which descends via the psoas major muscle fibeRs and follows the iliopectineal line, is formed from these roots. The nerve arises close to the pelvic brim from the medial margin of the psoas major.
Then, along the distal portion of the ureter, the lateral side of the internal iliac artery, and posterior to the common iliac arteries, the obturator nerve descends in the direction of the obturator canal. It runs in front of the obturator vessels in the lower pelvis. Through the obturator canal, the nerve leaves the pelvis on its way to the medial thigh.
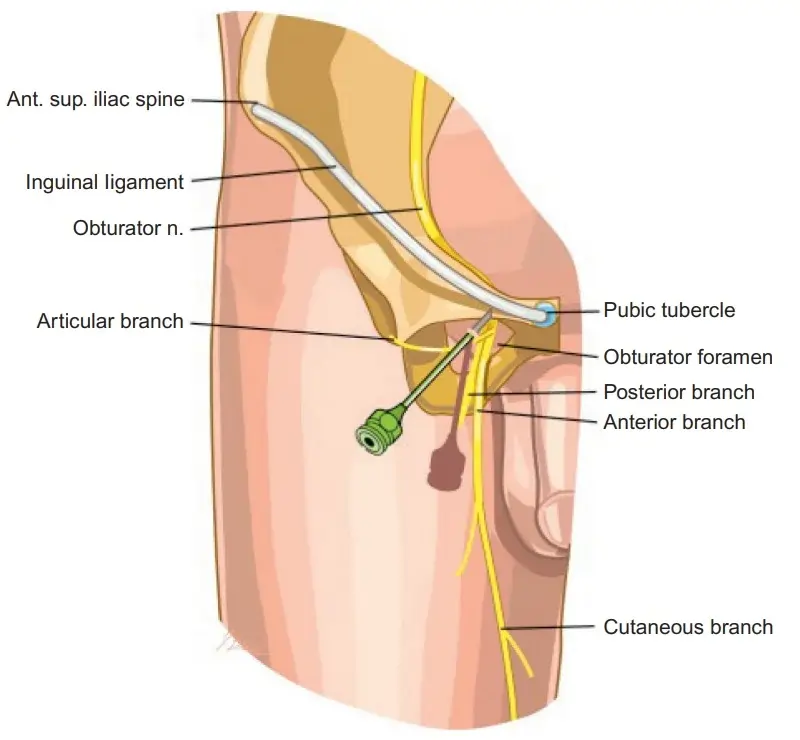
Near the obturator canal, it divides into anterior and posterior divisions. Between the adductor longus and adductor brevis, the anterior branch of the obturator nerve continues its journey until coming to an end as the cutaneous branch. The posterior branch runs between the adductor brevis and the adductor magnus.
The obturator nerve innervates the skin of the medial region of the upper thigh through the terminal branch of the anterior division. It also provides motor innervation to the adductor muscles of the lower leg, including the external obturator, gracilis, adductor longus, adductor magnus, and adductor brevis.
Function
The Anterior branch provides
- Motor innervation is received via the gracilis, adductor brevis, adductor longus, and, in rare instances, the pectineus.
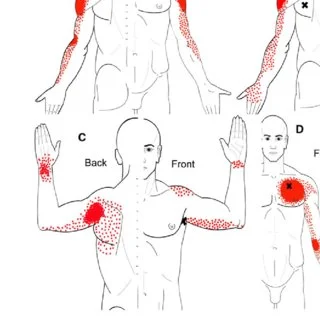
- The medial thigh and the area just above the medial knee are cutaneously innervated by the anterior branch of the obturator nerve.
The obturator nerve’s posterior branch
- Provides innervation to the adductor longus, adductor brevis, adductor magnus, and obturator externus.
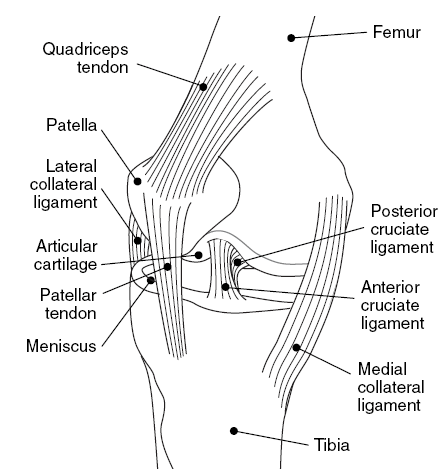
- The obturator nerve also sends articular branches to the knee and hip joints.
Course
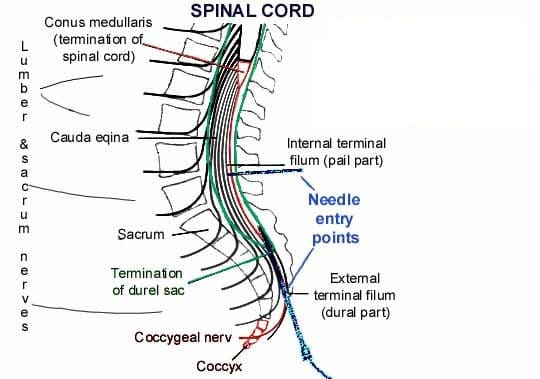
The obturator nerve is formed by the union of the anterior roots of spinal nerves L2, L3, and L4 close to the iliac crest. Through the fibers of the psoas’ major muscle and out of its medial border at the pelvic brim, the nerve enters the smaller pelvis.
In this case, the nerve travels along the pelvic wall posterior to the common iliac artery and lateral to the internal iliac arteries. After that, it leaves the pelvis by going via the obturator canal and into the thigh’s medial compartment.
Through the obturator canal, which is created by the obturator membrane within the obturator foramen, the obturator nerve reaches the medial thigh. It splits into anterior and posterior branches after that.
Anterior division (anterior to the adductor brevis):
- Descends towards the femoral artery in a plane between the adductor longus and adductor brevis.
- Here, it supplies motor fibers to the adductor brevis, adductor longus, and gracilis. The pectineus muscle may also receive its nourishment from it.
- After that, it becomes the cutaneous branch of the obturator nerve by penetrating the fascia lata.
Posterior division (posterior to the adductor brevis):
- Descends in a plane between the adductor brevis and adductor magnus after piercing the obturator externus muscle.
- Innervates the obturator externus and adductor magnus.
Branches
Both of the obturator nerve’s branches emerge in the thigh shortly after the nerve passes through the obturator canal.
The obturator nerve’s anterior branch (or division) crosses the adductor brevis muscle’s surface and extends deep to the adductor longus. It is located in between these two muscles in cadavers. Along with muscular and cutaneous branches, this nerve ramifies into an articular branch that leads to the hip joint. While the muscular branches feed the adductor longus, adductor brevis, and gracilis muscles (and sometimes the pectineus muscle), the cutaneous branches innervate the medial thigh’s overlaying skin.
After puncturing the obturator externus, the posterior branch (division) of the obturator nerve crosses the adductor magnus. In addition to providing articular branches that feed the knee joint capsule, it serves both of these muscles. Keep in mind that the tibial division of the sciatic nerve provides the adductor magnus’s ischiocondylar (hamstring) portion, but the obturator nerve simply supplies the pubofemoral (adductor) portion.
In conclusion, the adductor longus, adductor brevis, gracilis, obturator externus, and ischiocondylar portion of the adductor magnus muscle are all motorly innervated by the obturator nerve. In addition to providing articular branches to the hip and knee joints, its cutaneous distribution encompasses the skin of the proximal portion of the medial thigh.
Anatomical Variations
The medial thigh, obturator canal, or pelvic cavity are the three different locations where the obturator nerve bifurcates. After going through the obturator canal, the obturator nerve normally splits into anterior and posterior divisions before entering the thigh. Nonetheless, the obturator nerve may bifurcate in the thigh (25%), intrapelvic (23.22%), or obturator canal (51.78%).
Furthermore, the anterior branch may develop two, three, or four branches, with three being the most common. The posterior branch, on the other hand, might divide into one to four subdivisions, with two divisions being the most common kind. Nine distinct branching patterns were seen in the obturator nerve’s articular branches. Though it has been demonstrated to offer no cutaneous innervation in over 50% of instances, studies have indicated that the obturator nerve innervates the skin surface of the medial thigh.
Embryology
Neuroepithelial cells give birth to the peripheral nervous system. After migrating from the pia mater to the periphery, these neuroepithelial cells undergo differentiation into glioblasts, ependymal cells, and neurons. These cells aid in the development of future obturator nerves and the lumbar plexus.
Clinical Importance
The thigh adductor muscles are innervated by the obturator nerve, hence blocking it has therapeutic value. During surgery, the obturator nerve block (ONB), as previously mentioned, can aid in immobilizing the adductor muscle. Moreover, ONB can alleviate chronic groin/thigh discomfort, relieve adductor spasticity, and offer analgesia for hip and knee operations because of the articular branches of the obturator nerve to the hip and knee.
Therefore, ONB may be beneficial for illnesses including multiple sclerosis, traumatic brain damage, hip fractures, and total knee replacement. Percutaneous radiofrequency lesioning of the articular branches of the obturator nerve has been proposed as a useful treatment for hip joint discomfort if a basic ONB is unable to provide analgesia.
Numerous pathologic disorders involve the obturator nerve. Obturator hernias usually affect old, thin women or people who have high intra-abdominal pressure because of COPD, ascites, or a persistent cough. The small bowel becomes obstructed in an obturator hernia when the hernia sac passes through the obturator foramen and the obturator canal. Acute small intestine obstruction and discomfort in the medial portion of the upper thigh from obturator nerve compression are hallmarks of the clinical course.
The most sensitive and accurate imaging technique for quickly diagnosing an obturator hernia is computed tomography (CT). In the meantime, surgically fixing the hernia is the final therapy. Depending on the intraoperative results, bowel resection and/or a colostomy may be necessary if the intestine is ischaemic. Because the pelvic peritoneum relaxes and a broader, more horizontal obturator canal develops during pregnancy, obturator hernias can also happen in older women.
In the same way that a hernia can compress the obturator nerve, fascia or other pelvic tissue can also compress the nerve. In particular, the nerve may become caught by fascia farther away or near the obturator canal’s outlet. Exercise-induced medial thigh discomfort is usually experienced by athletes due to obturator nerve entrapment. While resisted adduction does not cause discomfort, hip abduction and extension make it worse. Although there hasn’t been much study on conservative treatment, manual therapy, neural gliding, cognitive behavioral education, and stretching and strengthening exercises may help reduce symptoms. If symptoms are not improving with therapy, neurolysis or neurectomy can be worth considering.
Damage to the Obturator Nerve
Surgery on the abdomen or pelvis may cause injury to the obturator nerve.
Among the symptoms are weakness in thigh adduction numbness and paraesthesia on the medial part of the thigh. Alternatively, the lack of adduction may cause the patient to have issues with posture and gait.
Block of the Obturator Nerve
Obturator nerve blocks are used to treat persistent hip discomfort or pain following lower limb surgery. The anesthetic is administered lateral to the adductor longus muscle tendon and inferior to the pubic tubercle. It is also possible to do this surgery under ultrasound supervision.
Obturator Neuropathy
Signs and symptoms
- Along the medial part of the thigh, pain and paresthesias may radiate from hip to knee.
- Pain may worsen with lateral leg movement or extension.
- Walking difficulties or leg weakness might result from issues adducting the ipsilateral hip.
Indications
- Hip adductor weakness on the affected side
- Medial thigh wastage
- abnormal hip abduction when walking, which causes a wide-based, circumduction gait
- The mid and lower part of the medial thigh is an area of sensory loss or change that occasionally extends below the knee.
- Ipsilateral lack of the hip adductor tendon reflex (which is not always present in healthy populations; check against an asymptomatic leg)
Examination
- Needle EMG can verify acute or chronic hip adductor denervation while ruling out other lower extremity muscles such the quadriceps or iliopsoas
- When intra-pelvic mass lesions are suspected of entrapping the nerve, ultrasonic imaging, CT, or MRI may be performed.
Surgical Importance
Surgery involving pelvic dissection and access put the obturator nerve at risk for damage. Regardless of the surgical technique used to treat pelvic organ prolapse, the obturator nerve and ureter are more vulnerable to harm. Laparoscopic pelvic operations, such as laparoscopic lymphadenectomy, can potentially cause damage to the obturator nerve. Furthermore, transvaginal mid-urethral sling deployments may cause damage to the obturator nerve.
When it comes to transurethral resection of bladder tumors (TURBT), which is frequently used to treat bladder wall tumors, the obturator nerve is very helpful. Due to the close closeness of the obturator nerve to the prostatic urethra, bladder neck, and inferolateral wall of the bladder, electrical stimulation caused by tumor removal may result in “adductor jerk,” or abrupt adductor contraction. This abrupt thigh movement may result in extravesical tumor seeding and bladder perforation. The obturator artery may also sustain injury as a result of the adductor jerk. The adductor jerk can be removed and a safe and efficient TURBT is made possible by conducting an obturator nerve block with a local anesthetic.
FAQs
Which muscle is innervated by the obturator nerve?
In conclusion, the adductor brevis, gracilis, obturator externus, ischiocondylar portion of the adductor magnus muscle, and adductor longus all receive motor innervation from the obturator nerve.
What are the symptoms of obturator nerve damage?
Depending on the extent of the damage to the obturator nerve, different symptoms may appear. Numbness, tingling, burning, or discomfort in the inner thigh or groin are typical symptoms. reduced feeling in the thigh, which can occasionally spread to the calf.
What is the primary function of the obturator?
To offer hip movement, the obturator muscles cooperate with the surrounding muscles. The external rotation of the hip is their main purpose. Furthermore, the flexed hip can be adducted with the help of the obturator externus and abducted with the help of the obturator internus.
How to test the obturator nerve?
Needlestick electromyography (EMG) is perhaps the most effective diagnostic for confirming obturator neuropathy. According to Bradshaw et al., athletes who have persistent groin discomfort due to obturator neuropathy exhibit chronic denervation in their short and long adductor muscles.
Where is the obturator muscle located?
pelvis
The inner surface of the pelvic anterolateral wall is where the internal obturator muscle originates. It surrounds the obturator foramen.It is connected to the ischium and inferior pubic ramus, as well as to the inside surface of the hip bone behind and under the pelvic brim.
References
- TeachMeAnatomy. (2023, October 15). The Obturator Nerve – course – motor – sensory – TeachMeAnatomy. https://teachmeanatomy.info/lower-limb/nerves/obturator-nerve/
- Obturator nerve. (2023, November 3). Kenhub. https://www.kenhub.com/en/library/anatomy/obturator-nerve
- Obturator nerve.(2023, July 24).StatPearls.https://www.ncbi.nlm.nih.gov/books/NBK551640/

One Comment