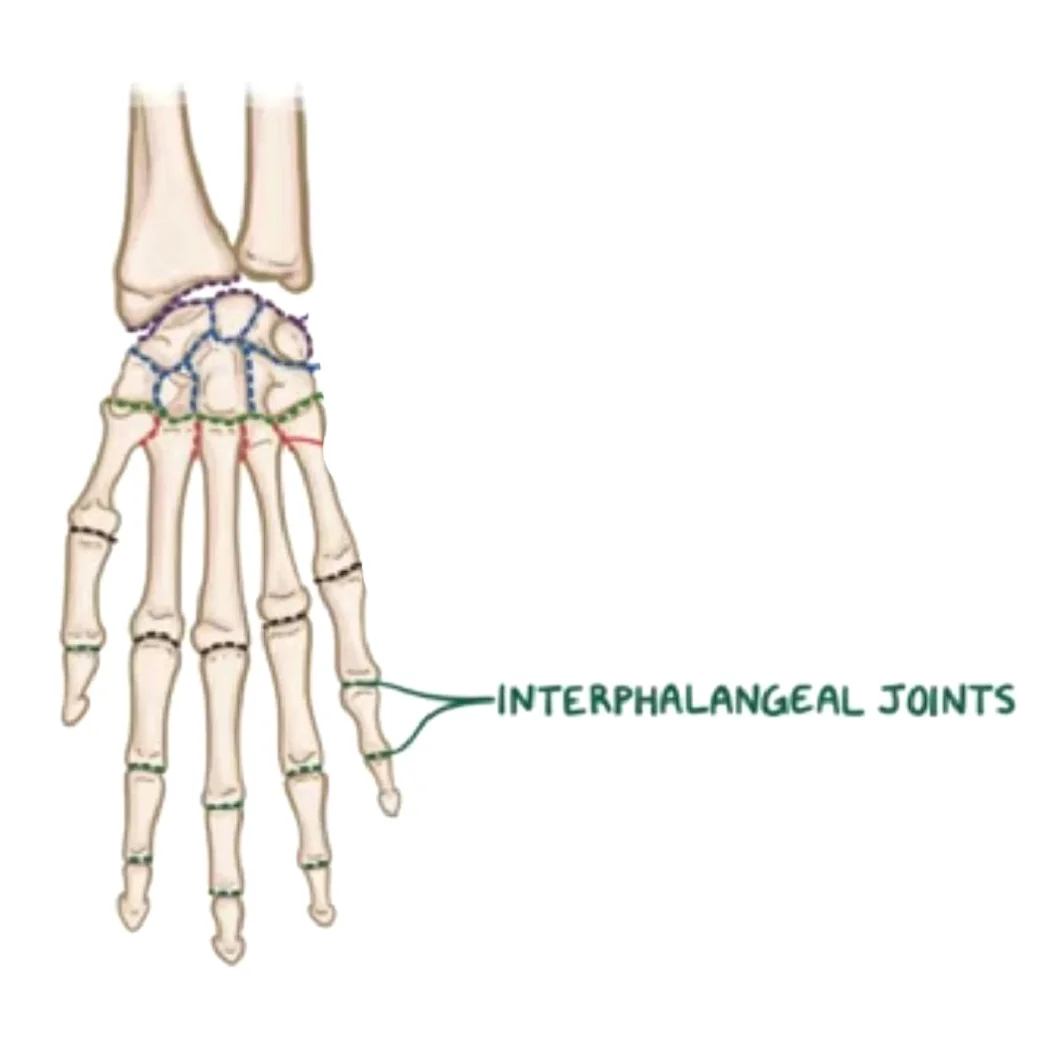
Interphalangeal Joints
The hand’s interphalangeal joints are the hinge joints that allow flexion in the direction of the palm between the finger phalanges.
Introduction
The hand’s interphalangeal joints are synovial hinge joints connecting the proximal, middle, and distal phalanges. These joints can be categorized into digits 2–5 according to the bones involved.
The middle and distal phalanges are separated by the distal interphalangeal joint (DIPJ or DIJ), and the proximal interphalangeal joint (PIPJ or PIJ) is situated between the proximal and middle phalanges. The thumb’s interphalangeal joint is simply called that because the first digit only has a proximal and distal phalanx.
The ability of the hand’s interphalangeal joints to support fine motor movements in the fingers. These joints enable movement in just one degree of freedom—flexion-extension—to achieve this.
Anatomy
Every finger (apart from the thumb, which has a single joint) has two sets.
- “Proximal interphalangeal joints” (PIJ or PIPJ), which are located between the first
- The distal interphalangeal joints (DIJ or DIPJ) are located between the third (distal) and second (intermediate) phalanges.
The proximal and distal interphalangeal joints share many anatomical similarities. The distal joint’s smaller size and decreased mobility are the main differences, with a few minor variations in the segmentation of the flexor tendon sheath and the proximal attachment of the palmar plates.
Joint structure
There is a lot of lateral stability in the PIP joint. Its thick collateral ligaments are tight in all positions during flexion, unlike those in the metacarpophalangeal joint, and its transverse diameter is larger than its anteroposterior diameter.
Dorsal structures
Due to the extremely thin and flexible capsule, extensor tendon, and skin dorsally, both phalanx bones can flex more than 100° until the base of the middle phalanx touches the proximal phalanx’s condylar notch.
Three bands separate the extensor mechanism at the PIP joint level. The dorsal tubercle of the middle phalanx, close to the PIP joint, is where the central slip is attached. After the PIP joint, the two lateral bands that support the extensor tendons continue dorsally to the joint axis. A transverse retinacular ligament, which connects the flexor sheath at joint level to the palmar border of the lateral band, holds these three bands together and stops the lateral band from dorsally shifting.
The oblique retinacular ligament [of Landsmeer] is located on the palmar side of the joint axis of motion and extends from the terminal extensor tendon to the flexor sheath across the proximal phalanx. In extension, the oblique ligament pulls and tightens the terminal extensor tendon proximally, preventing passive DIP flexion and PIP hyperextension.
Palmar structures
A thick ligament, on the other hand, stops hyperextension on the palmar side. With a fibrocartilaginous structure, the palmar plate, the distal portion of the palmar ligament, is 2 to 3 millimeters (0.079 to 0.118 inches) thick. For the dorsal and palmar plates to withstand compression forces against the proximal phalanx’s condyles, chondroitin, and keratan sulfate are essential. The tendons that run in front of and behind the joint are shielded by these structures working together. Collagen fibers in these tendons allow them to maintain traction forces.
Articulating Surfaces
The head of the more proximal phalanx and the base of its distal counterpart make up each interphalangeal joint. This implies that, for instance, the union of the head of the proximal phalanx with the base of the middle phalanx forms the proximal interphalangeal joint. The articulation of the middle phalanx’s head with the distal phalanx’s base forms the distal interphalangeal joint, which follows the same pattern.
Upon closer examination of the phalangeal head, two curved condylar processes with a shallow groove between them are visible. Two concavities of equal size and shape on the base of the distally lying phalanx receive these condyles.
A raised ridge of bone sits between these two concavities and slides into the phalangeal head’s groove, enhancing intraarticular stability. The proximal articular surface is larger than the distal surface because of the layer of hyaline cartilage covering these joint surfaces, which extends farther palmary than dorsally. There is less articular surface on the dorsal aspect, which results in less hyperextension than in the metacarpophalangeal joints.
The condylar processes’ inner sloping surfaces rather than their apex are where the point of articulation is located. The joint becomes noticeably out of alignment as a result of the radii of the phalangeal head’s condyles being larger than those of the phalangeal base’s convex surfaces. Most people have a small intercondylar joint space as a result of this incongruency.
Joint capsule and ligaments
Each interphalangeal joint has a fibrous joint capsule with a synovial membrane as its inner lining. Two collateral ligaments and a palmar ligament, sometimes referred to as a palmar/volar plate, strengthen each joint capsule. Dorsally, the extensor tendons broaden, strengthening the joint capsule. The phalangeal base’s articular surface is increased by this substantial ligamentous contribution to each joint capsule, enhancing joint congruence.
Collateral ligaments
The collateral ligaments originate from the head of the more proximal phalanx and extend to the palmar, or volar, aspect of its distal counterpart, running along either side of each interphalangeal joint. Each collateral ligament gives rise to an accessory ligament that attaches to the palmar ligament fibers by extending anteriorly. The excessive adduction-abduction movements of the interphalangeal joints are lessened by these ligaments.
Palmar ligament
Each interphalangeal joint’s palmar surface has a thick fibrocartilage plate called the palmar ligament, also known as the palmar or volar plate. The distal portion of this ligament, which blends with the accessory collateral ligaments, arches across the base of the distally lying phalanx, giving it the distinctive upside-down “U” shape. The periosteum of the body of the more proximally positioned phalanx incorporates the legs of the palmar ligament proximally. These ligaments, which are known as “check rein” ligaments, keep the joint from being overextended.
When flexion occurs, the proximal margin of the palmar plate and the accessory ligament fold back upon themselves because they are both flexible. At the PIP joint, the proximal fibers of the C1 ligament and the A3 pulley connect the flexor tendon sheaths to the mobile volar ligament, while the annular pulleys A2 and A4 securely fasten the sheaths to the proximal and middle phalanges. This configuration creates a gap at the proximal phalanx’s neck during flexion, which the folding palmar plate fills.
The collateral ligaments, which support the palmar plate, are located on either side of the joint and stop it from deviating from its normal position. The finger can be forced backward into hyperextension, causing the ligaments to tear partially or completely and avulse with a small fragment of fracture. A “palmar plate, or volar plate injury” is what this is known as.
Together with the distal portion of the joint, the palmar plate creates a semi-rigid floor, and the collateral ligaments form the walls of a mobile box that stabilizes the joint throughout its full range of motion. The palmar plate also increases the moment of flexor action because it attaches to the flexor digitorum superficialis close to the muscle’s distal attachment. The two so-called check-rein ligaments that connect the palmar plate to the proximal phalanx in the PIP joint restrict its range of motion.
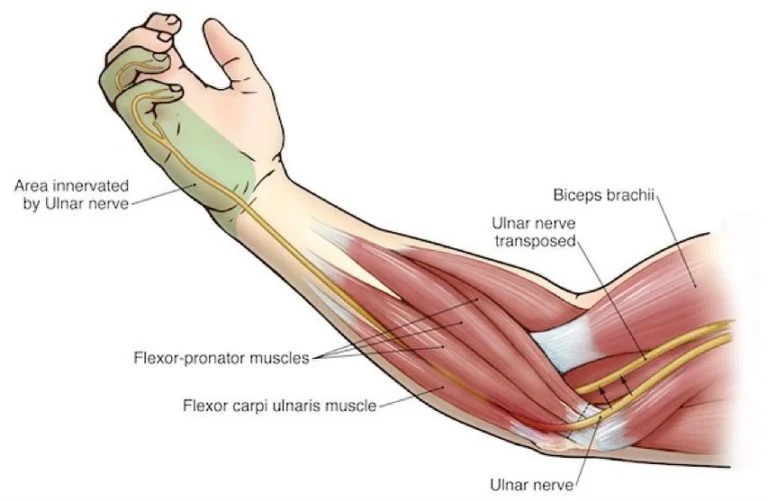
Innervation
The proper palmar digital nerves, which originate from the median and ulnar nerves, innervate the hand’s interphalangeal joints. The median nerve innervates the digits 1–3 and the lateral half of digit 4, whereas the ulnar nerve innervates the medial half of digit 4 and the entire fifth digit.
Blood supply
It is the distal extensions of the superficial palmar arch that supply oxygenated blood to each interphalangeal joint through the proper palmar digital arteries.
Movements
The hand’s interphalangeal joints’ morphology allows for only flexion and extension as active movements. Nonetheless, passive accessory movements to a limited extent are permitted, mostly at the distal interphalangeal joints of fingers 2–5.
The thumb can flex and extend around a transverse axis that passes through the center of the proximal phalanx’s neck. The range of motion is up to roughly 90° flexion and 10° extension, with the possibility of passive hyperextension when the distal phalanx is subjected to significant force. The thumb’s interphalangeal joint is incapable of passive accessory rotation or lateral movement due to strong collateral ligaments.
The entire flexion and extension of digit 2, also known as the index finger, takes place in the sagittal plane. However, the flexion and extension of more medially lying digits occur more obliquely to better oppose the thumb.
The proximal interphalangeal joints’ degree of flexion increases slightly from digits 2 to 5, but it is generally considered to be between 100° and 110°. The digits 3 and 5 have the most and the least amount of flexion, respectively, in the distal interphalangeal joints (80° and 70°).
The wrist joint’s location affects how strongly the hand’s interphalangeal joints can flex each other. The flexor muscles in the fingers lengthen when the wrist is extended, which increases the amount of tension that can be created in them and strengthens the grip. These finger flexors, on the other hand, become slackened and less able to produce tension when the wrist is flexed. This shows up as a weakened grip.
The range of active extension for digits 2–5 is much smaller, reaching up to 2° in the proximal and 5° in the distal interphalangeal joints.
The interphalangeal joints of every hand digit are in the closed-packed position of full extension and the open-packed (resting) position of slight flexion. These joints are more restricted in flexion than in extension due to their capsular pattern.
Passive accessory movements, such as abduction-adduction, rotation, and anteroposterior gliding, are restricted to digits 2–5. The fingers can adjust to objects of different sizes and shapes while gripping thanks to these subtle movements.
Muscles acting on the interphalangeal joints
Many muscles can act on the fingers, which reflects their exceptional dexterity. The flexion-extension movements at the hand’s interphalangeal joints are produced by both intrinsic and extrinsic hand muscles.
The flexor pollicis longus muscle is responsible for contracting the thumb’s interphalangeal joint. While the flexor digitorum profundus and flexor digitorum superficialis flex the proximal interphalangeal joints of digits 2–5, the latter also flexes the distal phalanx, making it the only muscle that can flex the distal interphalangeal joints.
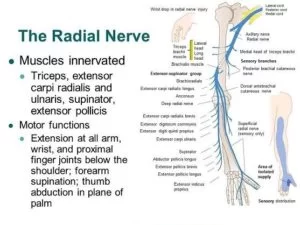
The extensor pollicis longus is responsible for extending the thumb’s interphalangeal joint. The extensor digitorum, lumbricals, and dorsal interossei all work together to extend the proximal and distal interphalangeal joints of digits 2–5. The palmar interossei aid in the extension of digits 2, 4, and 5, while the extensor indicis provides an extra extension for digit 2, the index finger.
Through their tendinous aponeurotic insertion into the extensor expansion, the muscles that extend digits two through five do so. Anchored on both sides by the palmar ligament, this hood-like expansion stretches down the length of digits 2–5. In the middle of each finger, it serves to keep the extensor tendons pulling in the same direction.
Clinical significance
The distal interphalangeal joints are typically unaffected by rheumatoid arthritis. Therefore, osteoarthritis or psoriatic arthritis is strongly suggested when distal interphalangeal joint arthritis occurs.
- Heberden’s nodes in the distal interphalangeal joint are one example of the degenerative joint disease known as osteoarthritis (OA), which affects IP joints and causes pain, stiffness, and deformity.
- An autoimmune disease that causes inflammation and joint abnormalities, such as boutonnière and swan-neck deformities, is rheumatoid arthritis (RA).
- Trauma-related fractures and dislocations are frequent (e.g., sports injuries, crush injuries).
- The inability to extend the fingertip due to damage to the distal interphalangeal (DIP) joint is known as a mallet finger.
- The condition known as trigger finger (stenosing tendinitis) is characterized by inflammation of the flexor tendons, which results in excruciating finger locking.
- Nail changes and “sausage fingers” (dactylitis) are symptoms of psoriatic arthritis.
FAQs
Interphalangeal joints: what are they?
The hand’s interphalangeal joints (green) The hinge joints between the finger phalanges that allow flexion in the direction of the palm are known as the hand’s interphalangeal joints.
What is the finger’s IP joint?
The interphalangeal joints are located between the middle and distal phalanges (distal interphalangeal joint, or DIP) and proximal and middle phalanges (proximal interphalangeal joint, or PIP) in each finger (except the thumb, which only has one interphalangeal joint and proximal and distal phalanges).
What category do the interphalangeal IP joints fall under?
The hand’s proximal, middle, and distal phalanges are separated by the interphalangeal joints, which are synovial hinge joints.
What is the thumb’s interphalangeal IP?
The tiny joints that connect the fingers and thumb are called interphalangeal (IP) joints. These are the joints that connect the fingers. The proximal interphalangeal joint (PIPjt) and the distal interphalangeal joint (DIPjt) are the two interphalangeal (IP) joints found in each finger.
On the other hand, how many IP joints are there?
The thumb only has two phalanges and one interphalangeal joint, whereas every other finger has three phalanges separated by two interphalangeal joints. The proximal interphalangeal joint (PIP joint) is the first joint near the knuckle joint.
What is the thumb IP joint’s range?
The average IPJ range of motion was 12 ± 9.2 ° (range 0–45 °) for extension and 88 ± 2.3 ° (range 80–90 °) for flexion.
Which hand interphalangeal joint is the first one?
The hand’s interphalangeal (IP) joints are hinge-style synovial joints that connect neighboring phalanges. The second to fifth fingers each have a proximal and distal interphalangeal joint, while the thumb has a single interphalangeal joint.
What is IP arthritis?
Arthritis of the fingers is known as interphalangeal joint arthritis. Every finger on your hand, except the thumb, is made up of three phalanges, or finger bones, which are divided by two joints called interphalangeal joints.
References
- Wikipedia contributors. (2025b, January 20). Interphalangeal joints of the hand. Wikipedia. https://en.wikipedia.org/wiki/Interphalangeal_joints_of_the_hand
- Interphalangeal joints of the hand. (2023, October 30). Kenhub. https://www.kenhub.com/en/library/anatomy/interphalangeal-joints-of-the-hand


One Comment