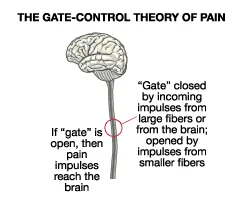
Gate Control Theory of Pain
The Gate Control Theory of Pain, proposed by Ronald Melzack and Patrick Wall in 1965, revolutionized our understanding of how pain is perceived in the human body.
This theory suggests that pain is not merely a direct result of physical injury or tissue damage, but rather is modulated by complex interactions between sensory signals, nerve fibers, and the central nervous system.
What is the nature of pain?
A number of things, such as illness, trauma, or mental discomfort, can cause pain, which is a complex and unique feeling. One of the numerous mechanisms influencing pain perception is the nervous system’s capacity to transfer information from peripheral nerves to the brain and spinal cord, where pain is finally experienced.
Ronald Melzack and Patrick Wall originally developed the gate-control theory of pain in 1965. The perspective postulates that a spinal cord gating mechanism, which permits or prohibits pain impulses from reaching the brain, regulates the amount of pain experienced. This theory has affected our understanding of the physiological processes behind pain and impacted the development of pain management strategies.
The structure of pain:
Gaining a solid comprehension of pain awareness is essential to fully comprehend the gate control theory of pain. Peripheral nerves, which are sensitive to unpleasant stimuli including pressure, severe temperatures, and tissue injury, are the source of pain signals. By using the dorsal root entry point, sensory neurons enter the spinal cord and transmit these electrical signals. After entering the spinal cord, several neurons filter the pain signals before sending them to the brain for interpretation and pain perception.
The gate control theory of pain:
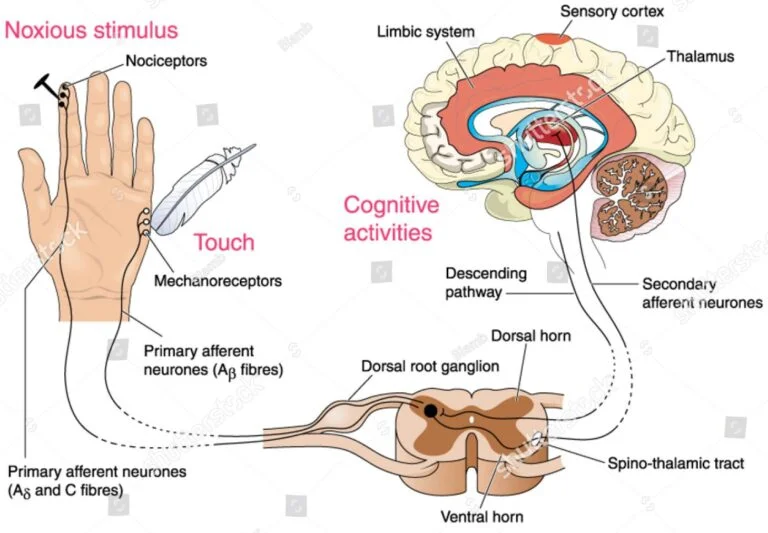
The Gate Control Theory of Pain contends that interactions between complicated processes occurring at different levels of the nervous system govern how pain is perceived, rather than just being a linear experience. The core principle of the Gate Control Theory of Pain is that nociceptive impulses can be facilitated or prevented from contacting the brain via a neural “gate” situated in the spinal cord.
Modulating this gate are both small-diameter unmyelinated C fibers and large-diameter myelinated A fibers. While the A fibers convey information about non-painful sensations like touch and pressure, the C fibers convey information about pain and other unpleasant sensations.
The neurological circuitry that controls the gate is housed in the horn of the spinal cord. Substance P, a neurotransmitter released by activated C fibers, opens the gate and activates these neurons, allowing nociceptive impulses to reach the brain. But when the A fibers are stimulated, they release glutamate, a separate neurotransmitter that triggers a distinct group of neurons to close the gate and block the passage of nociceptive impulses.
Apart from the aforementioned major fibers, various other factors can also influence the opening and closing of the gate. These factors include descending routes originating from the brainstem and higher centers in the brain, along with additional sensory data gathered from the body and surroundings. Anxiety and concentration, for instance, are examples of emotional and cognitive variables that can affect how pain is perceived by triggering descending pathways that either increase or decrease dorsal horn neuron activity.
Physiology:
Substituting the portion of substantia gelatinosa in the dorsal horn of the spinal column is the pain gate mechanism. When the substantia gelatinosa interneurons connect with primary afferent neurons, the gating mechanism occurs there. Consequently, the sensory data arriving from the primary afferent neurons is modulated by the substantia gelatinosa.
Three types of primary neurons exist:
Neural cues like light pressure, gentle touch, and hair transpiration stimulate the large diameter A-ß fibers. Because of their myelination, these fibers have a rapid impulse transmission rate.
Smaller in diameter A-d fibers are lightly myelinated and triggered by noxious stimuli, specifically sharp, strong, tingling sensations, pain, and warmth.
Because they are not myelinated, C fibers, like A-d fibers, transmit impulses at the slowest rate. Pain and temperature, specifically prolonged burning sensations, activate C neurons.
In this case, non-noxious diameter A-ß fibers stimulate the interneurons in the substantia gelatinosa, causing an inhibitory response and blocking the transmission of pain signals to the brain. This closes the “pain gate.”
Whenever the smaller-diameter A-d or C fibers stimulate the interneurons, an excitatory response is produced. Here, the brain receives pain signals that can be changed, transmitted back down through descending modulation, and experienced as different intensities of pain.
The small diameter A-d and C fibers’ ability to transmit can likewise be lessened and inhibited by activating the big diameter A-ß fibers.
Consequences for managing pain:
The theoretical idea of gate control of pain has significant benefits for pain treatment. One of the main ramifications is that non-pharmacological treatments including physical therapy, cognitive-behavioral therapy, and relaxation methods might influence how much pain is felt. These treatments may decrease pain signals and enhance the spinal cord’s gating system by promoting inhibitory pathways in the brain and spinal cord.
The spinal cord’s gate mechanism can also be changed via pharmacological means. In one instance, opioids such as morphine may reduce the transmission of pain signals by activating inhibitory circuits in the brain and spinal cord. Lowered excitatory neuron activity in the spinal cord is another way that non-opioid medications such as pregabalin and gabapentin can modify the gate mechanism.
How to attempt to minimize your suffering:
It separates the terminology used to describe bodily discomfort into two categories:
The sensational aspect of pain is linked to the intensity or kind of pain you’re experiencing. Words like “throbbing,” “aching,” “sharp,” “tingling,” or “burning” might be used to describe these sensations, which are processed in the somatosensory cortex region of your brain.
Pain’s affective dimension is linked to its psychological component, which includes factors like pain’s level of discomfort. The limbic system of your brain processes these emotions, which can be described by adjectives like “agonizing,” “torturous,” “miserable,” or “excruciating,” among others.
To keep those gates closed, the goal is to figure out how to keep that area of your brain dormant. These three factors affect your limbic system, which can reduce pain.
The diversion
Your brain is unable to give your discomfort its full attention when it is preoccupied with something else.
Has there ever been a case where a person with chronic pain disappears to pursue their hobby? That is the ability of diversion. For instance, crocheting, crossword puzzles, virtual reality, or even binge-watching your favorite TV show can help distract you from your discomfort while you’re healing from surgery.
Profound calm
Deep relaxation techniques are so effective that they have been demonstrated to assist patients limit, and in some cases even totally avoiding, the usage of opioids following surgery. Research indicates that individuals who engage in deep relaxation practices have a quicker healing rate following surgery.
Reflections
Your viewpoint on pain affects not only how much physical pain you endure but also how long it takes you to recuperate.
She suggests engaging in a method known as “thought-stopping,” which is precisely what it sounds like choosing to divert particular ideas when they arise.
Imagine yourself at a stop sign, watching as your mind wanders in that direction. Ultimately, the decision to follow that route is all yours. If you know the course will only make you feel worse, feel free to take an alternative one. However, you are welcome to continue on that one.
Conclusion:
In conclusion, there are significant therapy implications for the Gate Control Theory of Pain. It offers a framework for creating non-pharmacological pain management techniques including massage, acupuncture, and physical therapy.
It is believed that these methods work by reducing the number of nociceptive impulses that are transmitted to the brain by opening the gate and stimulating the A fibers. New pharmacological painkillers that target the neurotransmitters and receptors responsible for opening and closing the gate have also been developed as a result of the notion.
All things considered, the Gate Control Theory of Pain offers a thorough comprehension of the perception and management of pain. It has gained widespread acceptance and greatly advanced methods and therapies for pain control. It is crucial to remember that the hypothesis has drawbacks and that more investigation is required to completely comprehend the intricate interactions between the neurological system and pain perception.
FAQs
What is the theory of pain gait?
The central nervous system can record pain if the gate is open, allowing pain impulses to enter the system. By blocking the gate, pain signals are not going to be capable of entering the brain and the person will not feel pain.
Which quartet of pain theories exists?
The Specificity (also known as the Labeled Line), Intensity, Pattern, and Gate Control Theories of Pain are the four most prominent theories of pain perception.
Who first proposed the pain gate theory?
Ronald Melzack and Patrick Barriers devised the Gate Theory of Pain, published in Science in 1965. Its purpose was to offer a method for encoding the nociceptive aspect of cutaneous sensory input.
What is pain and the Neuromatrix theory?
Neuronal functions and impulse patterns are the source of pain, according to the neuromatrix theory. Each person has a unique neuro matrix that is shaped by their genetic makeup and altered over time by memories and sensory experiences.
What does the gate theory of pain look like in practice?
Another illustration of the gate control hypothesis of pain would be if someone were to stub their big toe. The nervous system’s spinal cord would get the pressure and touch sensation right away, and the projection neurons in the cord would subsequently send the signal to the brain.
References
- Clinic, C. (2024b, August 2). Pain and the Brain: What Is the Gate Control Theory? Cleveland Clinic. https://health.clevelandclinic.org/gate-control-theory-of-pain
- Vaghela, M. (2023, March 4). Gate control theory of pain – Samarpan Physio. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/gate-control-theory-of-pain/