Electroconvulsive Therapy (ECT)
What is ECT?
Electroconvulsive treatment (ECT) is a method used to treat severe symptoms of some mental health issues. To induce of detailed seizure, an electric current is applied to the brain. ECT is performed under general anesthesia, ensuring the patient is not conscious during the procedure.
What can ECT treat?
Physicians are advised by the National Institute for Health and Care Excellence (NICE) to contemplate electroconvulsive therapy (ECT) only in certain situations.
This may involve using ECT to address severe depression if:
- You have a history of positive experiences with ECT and prefer it as a treatment option
- You need immediate medical attention, for example, if you are in danger of starvation.
- Other treatments like medication and talking therapies have not been effective
The guidelines also suggest that ECT should only be used as a short-term treatment if you are experiencing:
- A severe or prolonged episode of mania
- Catatonia is characterized by being immobile or displaying repetitive movements
Repeated ECT for mania and catatonia is only recommended if you have responded well to the treatment previously, or if all other treatment options have been exhausted.
According to the NICE guidelines, ECT is not recommended for the ongoing management of schizophrenia. Additionally, it is not recommended as a standard treatment for mild depression.
The whole set of recommendations for electroconvulsive therapy (ECT) treatment of severe depression and treatment of catatonia, mania, or schizophrenia may be seen on the NICE website.
Who needs to have this treatment?
ECT is appropriate for treating patients with serious mental illnesses and is appropriate for a wide age range. It is an option for children (with specific restrictions in some states), teenagers, and adults of all ages. The most significant advantages of ECT are typically observed in individuals aged 60 and above.
Why is ECT used?
When traditional medications are ineffective, ECT may be considered.
ECT may be used when an individual experiences a severe shutdown of function known as catatonia.
In cases where a person poses a danger to themselves or others, and traditional medications take days or weeks to take effect, ECT may be an option.
What conditions are treated with ECT?
Several disorders can be treated with electroconvulsive treatment (ECT), including:
- Depression, especially in those above sixty years old.
- Schizophrenia (which includes psychotic disorders as well as other conditions that fall within the spectrum of schizophrenia).
- Bipolar disorder as well as other mania-producing disorders.
How common is ECT?
ECT is not frequently used as an initial treatment for depression, even though it is both safe and effective. Numerous newer medications can be used to treat this condition. The availability of ECT is limited, as fewer hospitals provide this treatment for inpatients and outpatients.
Procedure Details
What happens before this procedure?
Your healthcare provider will explain ECT and how it works before you begin the treatment or someone who can make healthcare decisions for you. They will also ensure that you do not have any underlying health conditions or reasons that might prevent you from receiving ECT.
Before ECT, various tests may be conducted, including (but not limited to):
- Blood and urine tests, such as complete blood count, metabolic panel (basic or comprehensive), thyroid function, kidney function, and more.
- Imaging tests on your skull, brain, and spine, which may include X-rays and computerized tomography (CT) scans.
- An electrocardiogram (ECG or EKG) helps to check your heart function and detects any unusual changes or problems with your heart’s electrical system.
“Contraindications” refer to the conditions and factors that may prevent you from receiving ECT. These are evaluated individually, and even in cases where there are contraindications, medical professionals may frequently evaluate the course of therapy to allow for the continuation of ECT. Contraindications include:
- Myocardial infarction, recent heart attack, or other unstable cardiac diseases.
- disorders such as intracranial hypertension or brain tumors that raise the pressure within your skull.
- Aneurysm, stroke, or other recent brain hemorrhage causes.
- severe respiratory ailments, such as chronic obstructive pulmonary disease, or COPD.
- other potentially lethal conditions or those meeting the requirements for physical classification levels 4 or 5 of the American Society of Anesthesiologists.
Stopping fluids and food intake
Because the ECT process requires general anesthesia, your healthcare practitioner may advise you to fast before the operation. This implies that you have to fast for eight hours beforehand the procedure and not drink anything for two hours before the procedure.
What you should take off or remove
Because the ECT process requires general anesthesia, your healthcare professional will ask you to fast before the operation. Typical instances include removing your eyeglasses, contact lenses, hearing aids, false teeth, dental prostheses, etc. This precaution is taken to prevent any potential harm or choking hazards associated with these items.
Medication stoppage
Certain drugs may alter how ECT impacts you, potentially influencing the effectiveness of the treatment. Your healthcare professional might recommend discontinuing or lowering the dosage of specific medications. It’s crucial to follow your provider’s instructions while making adjustments to your medicines, though.
What happens during this procedure?
Many medical professionals, such as psychiatrists, anesthesiologists, and other qualified staff, are involved in ECT.
Anesthesia and other preparations
The ECT procedure begins with general anesthesia, which induces deep sleep and prevents any sensation of pain, discomfort, or anxiety during the procedure. A muscle relaxant is also administered to prevent potential injuries or strain during the seizure.
A bite guard is placed in the mouth to safeguard the teeth, and an intravenous (IV) needle is inserted into a vein, typically in the arm. The IV provides rapid access to medication administration for anesthesia and to counteract any potential side effects.
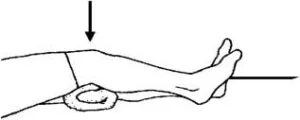
Electrode placement
Electrodes will be placed by a healthcare provider on the skin of your head to serve as contact points for the electric current. Your unique demands will dictate where the electrodes are placed, and the providers will choose a location that reduces the possibility of serious consequences. Providers have three different options for electrode placement.
Right unilateral: In this configuration, both electrodes are positioned on the right side of your head. One electrode is placed between your temple and the end of your eyebrow, while the other is positioned near the top of your head, directly above your right ear.
Bifrontal: Electrodes are placed on contradictory sides of your forehead, just above the end of your eyebrow.
Bitemporal
A healthcare provider will cover the electrodes with a conductive gel to prevent skin irritation and burns. Despite the very low level of electrical current used, there is still a risk of skin irritation and burns.
Electricity requirements
A modest electrical current, usually up to 0.4 amps, is used in ECT. To put this into perspective, a 9-volt alkaline battery can supply approximately 0.6 amps of current for one hour before depleting. Providers will gradually increase the current from low levels until the desired effect is achieved.
An ECT’s electrical current is only there for a very brief period. The brain is usually given short electrical current treatments most of the time.
Induced seizure
ECT induces a seizure by using an electrical current, which triggers a burst of electrical activity in the brain, causing affected brain cells to fire rapidly. This leads to improvements in that particular brain area’s functioning through electrical and chemical changes.
Seizures brought on by ECT usually last thirty to ninety seconds. If seizures persist longer, medical professionals can terminate the seizure by administering injectable medications.
What happens after this procedure?
After the seizure ends, medical professionals will observe you as you come out of anesthesia. They will also monitor your vital signs to detect any potential side effects or anesthesia-related issues.
After the treatment, most people regain full awareness in 10 to 15 minutes, and they may up and move around in 30 minutes.
Indications
Patients with treatment-resistant depression or severe major depression that impairs daily activities may be candidates for ECT. Depression that does not improve after taking antidepressants for many trials is referred to as treatment-resistant depression. ECT is also thought to be a therapy for catatonia, severe psychosis, depression-related food refusal, and self-harm.
Patients with bipolar illness can get ECT treatment throughout both their manic and depressive periods. In patients who are old, disabled, pregnant, or nursing, ECT may have a superior safety profile than antidepressants or antipsychotics. Suicidal thoughts can be rapidly distracted by ECT, with complete resolution observed in 38% of patients after one week, 61% after two weeks, and 81% after the completion of ECT.
Contraindications
Blood pressure, heart rate, and intracranial pressure may also momentarily increase as a verdict of using ECT. It is important to be cautious when treating patients with cardiovascular, pulmonary, or central nervous system conditions.
For people who have a pheochromocytoma or high intracranial pressure that puts pressure on the brain, ECT is not advised. Conditions such as high intracranial pressure without pressure on the brain, cardiovascular conduction issues, high-risk pregnancies, and aortic and cerebral aneurysms are considered relative contraindications for ECT.
Complications
Although this impact is temporary, bitemporal or bilateral ECT impairs cognition more than unilateral ECT. Three days following treatment, global cognition, verbal memory, and autobiographical memory were all poorer with bilateral therapy, according to a meta-analysis of 1415 depressed individuals receiving ECT.
According to the American Psychiatric Association, patients receiving ECT are more at risk if they have a history of acute cerebral hemorrhage or stroke, unstable vascular aneurysm, severe pulmonary disease, American Society of Anesthesiologists (ASA) Class 4 or 5 status, space-occupying intracranial lesion with evidence of high increased intracranial pressure, and another condition.
Throughout the tonic phase of the seizure, there is a physiological parasympathetic discharge that lasts for 15–20 seconds. This can result in bradyarrhythmias such as asystole, atrioventricular block, and premature atrial and ventricular contractions. Individuals who experience subconvulsive seizures are more susceptible to asystole.
Ironically, asystole is less common in individuals with underlying arrhythmias or heart blocks. A catecholamine rush that results in tachycardia and hypertension during the clonic phase of a seizure is correlated with the seizure’s length. After the seizure, tachycardia and hypertension usually go away in 10 to 20 minutes, while some individuals continue to have persistent hypertension that has to be treated by a doctor.
While ejection fraction can drop in healthy people after ECT, those with baseline cardiac illness are more vulnerable after therapy.
Of the 53 people who had ECT, seven experienced new global left ventricular (LV) systolic dysfunction, and eight experienced anomalies related to the movement of their regional walls.
LV dysfunction patients did not experience any negative consequences from this group of individuals. Eight patients had elevated cardiac troponin levels in a prospective cohort study including 100 people undergoing ECT; only two of these patients had further signs of myocardial ischemia or infarction. Cerebral blood flow as well as intracranial pressure both rise while the ECT therapy is done.
In a clinical setting, patients may show signs of memory loss, delirium, confusion, and disorientation. The AHA-ACC guidelines classify electrocardiography (ECT) as a low-risk procedure because of its excellent tolerance, transient hemodynamic lability, and low death rate.
Clinical Significance
ECT, an inter-professional procedure, is relatively safe and low-risk and is beneficial for the treatment of conditions such as depression, suicidality, severe psychosis, food refusal secondary to depression, and catatonia. Anesthesiologists, psychiatrists, nurses, and other para-medics need to coordinate care for this treatment.
Multiple sessions are usually required for a lasting effect. The stigma around ECT is mainly due to the lack of anesthesia in early treatments, which led to significant injury and severe memory loss. The effects of antidepressants usually take effect quickly and might linger for several years. When ECT is used under strict supervision, the death rate is extremely low, although, over time, moderate memory loss may result. ECT is frequently used in pregnant patients and the elderly due to the avoidance of side effects from psychotropic medications. Despite having a complex mechanism of action, ECT does alter regional metabolism along with cerebral blood flow.
Benefits of ECT vs. other therapies
ECT can be effective for many individuals when medications or psychotherapy are not successful. In general, it has less negative effects than prescription drugs.
ECT also works as a rapid relief of psychiatric symptoms. It can lead to the resolution of depression or mania after just one or two treatments, whereas many medications take weeks to show effects. As a result, ECT can be particularly advantageous for individuals who:
- suicidal
- psychotic
- catatonic
However, certain individuals might need ongoing ECT sessions or medication to sustain the positive effects of ECT. Your physician will have to closely track your improvement to decide on the most suitable post-treatment care for you.
ECT can be safely placed and used for pregnant women and individuals with heart conditions.
Side effects of ECT
The side effects of ECT are uncommon and usually accurate. They may include:
- Headache or muscle soreness in the hours following the treatment
- Momentary confusion after the treatment
- Nausea, typically shortly after a treatment
- Short-term or long-term memory impairment
- Rarely, irregular heart rate
ECT can potentially be fatal, but deaths are exceedingly rare.
Approximately 1 in 10,000 persons die from ECT. This ratio is lower than the anticipated 12 suicides per 100,000 people throughout the United States.
Overview
ECT, also known as electroconvulsive therapy, involves the administration of small electric currents to the brain under general anesthesia, intentionally causing a brief seizure. Such electrical currents appear to change brain chemistry in a way that alleviates some mental disorder symptoms immediately.
ECT is often effective when other treatments have failed, provided that the full course of treatment is completed, although it may not be effective for everyone. The early uses of ECT, which required giving huge amounts of electricity without anesthetic and led to memory loss, broken bones, and other serious side effects, are mostly to blame for the treatment’s negative reputation.
Today, ECT is much safer. Although it can still result in some side effects, it now delivers electric currents in a controlled environment to achieve the greatest advantages with the fewest possible risks.
FAQs
What is electro-compulsive therapy used for?
Electroconvulsive therapy (ECT) is a typically secure, low-risk treatment for depression, suicidality, severe psychosis, depression-related food refusal, and catatonia. Interprofessional care coordination between nurses, psychiatrists, and anesthesiologists is necessary.
Is electroshock therapy still used today?
In the United States, the standard protocol for electroconvulsive treatment (ECT) involves two to three weekly sessions over three to four weeks. On weekdays, some physicians do right unilateral ultra-brief pulse electroconvulsive treatment, a more recent method.
How does ECT work on the brain?
During an unconscious patient’s ECT session, a small quantity of electrical current is applied to the brain. The whole brain is affected by this current, including the areas that regulate mood, hunger, and sleep. It also induces a seizure.
What to expect after ECT treatment?
After being transferred to the recovery room, patients stay there until their respiration, heart rate, and blood pressure are almost back to how they were before treatment. This usually takes twenty to twenty-five minutes. Headaches, pains in the muscles, and nausea are the most frequent adverse effects that patients encounter.
Can you live a normal life after ECT?
In conclusion, after two and four weeks following treatment, ECT is linked to improvements in anterograde memory, mood, quality of life, and overall cognitive status. The majority of patients saw improvements in their function and quality of life.