Dermatomes
Dermatomes: What are they?
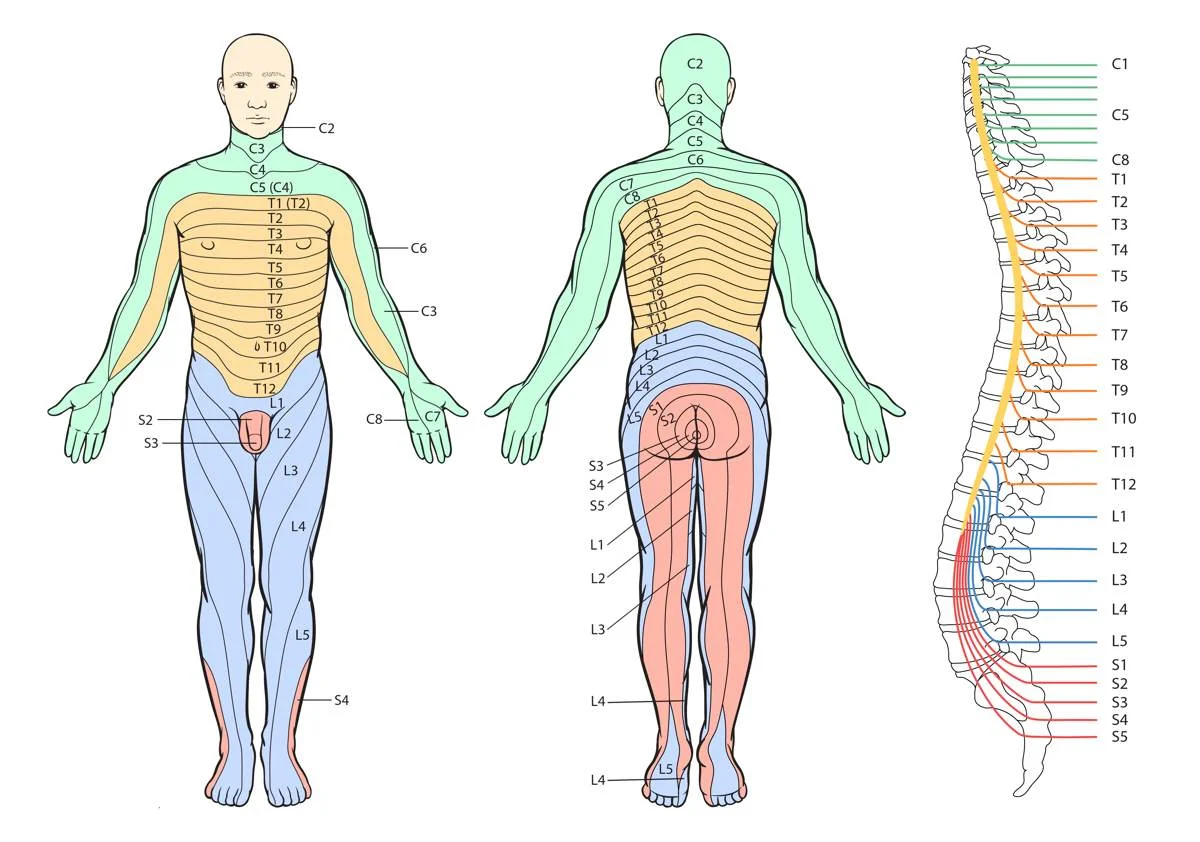
Dermatomes are skin sites that receive sensory information from the Afferent nerve fibers that emerge from a certain spinal nerve root’s dorsal root. An external portion of a nerve that “communicates” with the spinal cord is known as a vertebral nerve root.
The entire spinal cord is made up of nerve roots (like C3 and C4), and many, but not all, of these individuals come together to create a plexus (brachial, lumbar, or lumbosacral), which, as mentioned before, divides peripheral nerves. This configuration permits a single nerve root to supply several peripheral nerves.
Overall, thirty individual dermatomes—eight cervical nerves, twelve thoracic nerves, five lumbar nerves, and five sacral nerves—transmit sensation from one part of the skin’s outer layer to the brain’s centers and one cervical nerve. (Notice how C1 lacks a matching dermatomal region).
History:
Dermatomes arose as an early attempt to link the anatomy and physiology of feeling. Dermatomes are defined in several ways, and different maps are frequently used. Dermatomes are useful, although they can vary across maps and even between persons. An appropriate amount of evidence implies that the present dermatome maps are untrustworthy and based on questionable research.
Medical professionals were typically familiar with two primary dermatome maps. As discussed in the next section, the dermatomes in the Keegan and Garret Map (1948) symbolize the early stages of limb development. More importantly, the 1933 authors of Foerster Map depict the pattern of pain transportation following a myocardial infarction or angina by emphasizing the medial region of the upper limb transmitted by T1-3.
In their comprehensive research, Lee et al. examined the variations among dermatome maps and created an “evidence-based” map by combining components from prior maps.
Although the phrase “evidence-based” may raise some eyebrows, their suggested map is an organized effort to compile the most reliable data currently accessible.
Anatomy:
The dermatomes—where are they?
Skin regions known as dermatomes depend on nerves that attach to your spinal cord. That means that your entire body is covered in dermatomes except for your face. Because they do not have connections that pass through your spinal cord, the nerves in your face are an exception.
The neural connections at the spinal column’s base allow for significant overlap between dermatomes. Thus, feelings originating from a particular dermatome pass via several spinal nerves simultaneously.
A single vertebra, or set of interlocking bones, makes up your spine, commonly called your backbone.
There are five portions to your spine:
- The cervical vertebral column is located in this specific area of the neck.
- Thoracic vertebrae form the middle decades and upper back.
- lumbar spine: lower region of the back.
- The sacral spine has five pairs of spinal nerves and five vertebrae, which normally fuse by the time you’re an adult. The pelvic bones are located in the sacral spine, which has a butterfly-like shape. Your pelvic bones would act as the butterfly’s wings, and your sacral spine as its primary body.
- “coccygeal spine” is the coccyx or tailbone. It consists of one pair of spinal nerves and four vertebrae, which normally fuse when you’re an adult.
Workers in the medical field utilize a letter-number combination to refer to the spinal nerves.
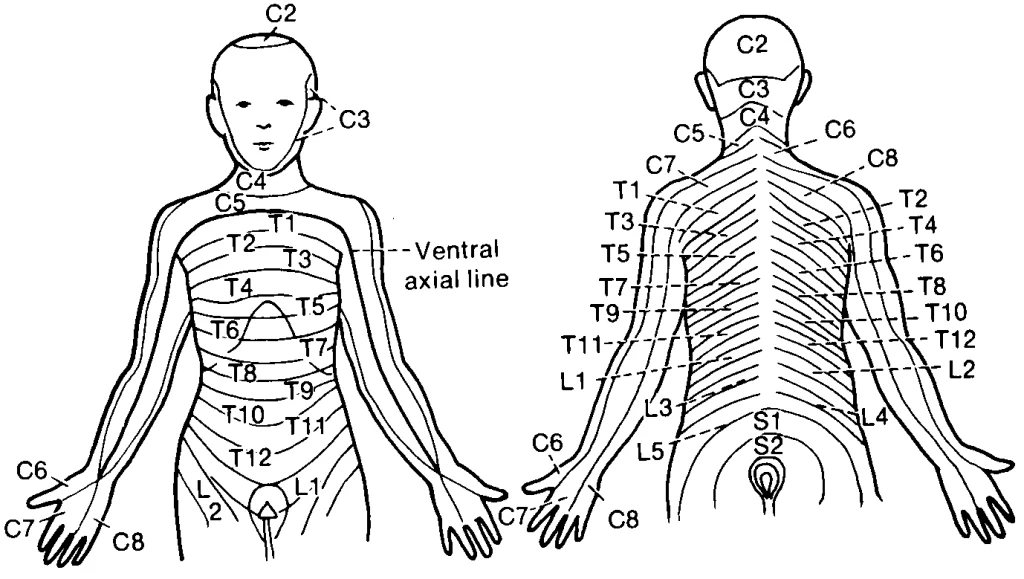
Cervical spine-related dermatomes:
head, neck, shoulders, arms, and hands are connected Dermatomes in the cervical region of your spine. The prevalence of cervical vertebral column nerves is categorized into numerous dermatomes, which are listed below:
- C1: This dermatome is located in the center of the back of the head for people with it.
- C2 to C3: Back of the head, upper neck, and jaw beneath each ear.
- C3-C4: Located between the neck’s back, chest, and lower portion.
- C4 to C5: Shoulders and upper arms
- The thumb, upper arm, and thumb make up the forearm region (C5–C6).
- C6-C7: forearm, index, and middle fingers.
- C6-C8 depicts a ring on your finger, lower forearm, and wrist.
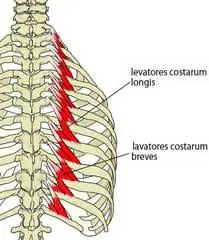
Thoracic spine-related dermatomes:
Most of your thoracic spine’s dermatomes are located on your trunk, which comprises your back, abdomen, and chest. The dermatomes of T1 (wholly on your arms) and T2 (on your arms and trunk) are the only thoracic-connected dermatomes not on your trunk. The dermatomes, which are T3–T12 in number, surround your body’s trunk in rings.
The dermatomes are located where:
- T1: the upper chest, armpit, and arm.
- T2 (upper chest and back)
- T3 (upper chest and back)
- T4: upper chest (nipples) and back
- T5: mid-chest, back
- T6: middle chest and back
- T7: middle chest and back
- T8: Upper abdomen and mid-back.
- T9 refers to the upper abdomen and middle back
- T10: abdominal (belly button) and mid-back
- T11: abdominal and mid-back.
- The mid-back and lower abdomen are represented by T12.
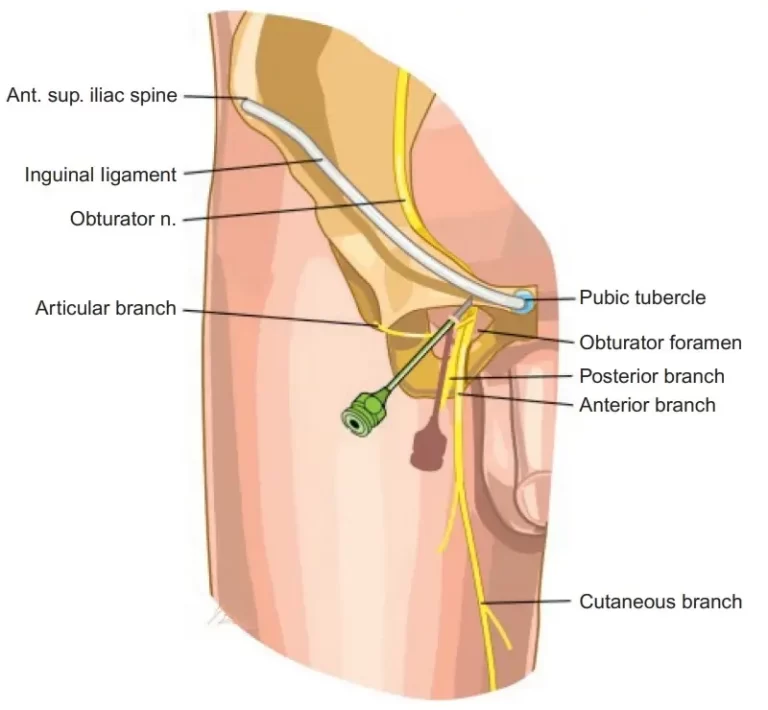
Lumbar spine-related dermatomes:
Your hips, legs, and feet are connected to the lumbar spine’s dermatomes. The dermatomes throughout can be discovered wherever they are:
- L1–L2: the lower back( vagina, penis, and testicles ).
- L2-L3 includes the lower extremities, groin muscles, and back.
- L3-L4: kneecap, lower back, leg, and front-thigh quadriceps muscles.
- L4-L5 calf muscles, front of the lower leg, kneecap, and inside surfaces of the foot, including big, second, and third toes.
The sacral and coccygeal spine’s dermatomes:
Your rear legs and the region surrounding your buttocks are among the dermatomes of your sacral spine. In the coccygeal region of your spine, there is only one spinal nerve and one associated dermatome.
- S1 to S2: The outer side of your ankles, your fourth and fifth toes, the middle and outer portions of the back of your thighs, and calf muscles.
- S2 to S3: A vertical region in the center of your buttocks that passes across the upper-middle and inner-middle portions of your calf muscles and the back of your thigh.
- S3 and below: the genitalia, anus, and the skin region between them (referred to as the perineum) are all connected to every spinal neuron from S3 down, including the coccygeal spinal nerve.
Which prevalent ailments and illnesses impact the dermatomes?
Although dermatomes are skin regions, the disorders that affect them are usually caused by deeper problems within your body. The dermatomes are impacted by problems that affect specific spinal nerves or the spinal cord in that region. For this reason, symptoms affecting dermatomes might arise from any illness affecting your spinal cord or spinal nerves. In certain instances, the harm is highly confined, although the consequences can be extensive based on the impacted dermatomes.
The following conditions might cause this type of injury or effect:
Injuries. These kinds of injuries are most frequently caused by vehicle accidents, penetrating trauma (such as gunshot or knife wounds), and spinal fractures from falls. Injuries received during childbirth or in the first few weeks of life may also cause this (cerebral palsy is one example).
Tumors of the spine. including malignancies. This can include cancer that begins elsewhere in your body and spreads to your spine, or it can comprise cancer that grows on or near your spinal cord.
cysts, or cavities filled with fluid. They are referred to as syringomyelia when they develop around your spinal cord.
infections. These may induce edema and inflammation or directly target your nerve roots and spinal cord. It can place too much pressure on your spinal nerves or the spinal cord itself because there isn’t much area for that swelling surrounding your spinal cord.
Blood flow is absent (ischemia). Blood flow is essential for many physiological systems, including the spinal cord and spinal neurons.
birth defects. myelomeningocele and spina bifida.
Shingles.
The virus that gives rise to becomes active and causes shingles, is most commonly referred to as herpes zoster. The virus may go dormant following chickenpox recovery and subsequently reactivate as shingles.
Before the rash, sometimes there may be localized discomfort, burning, or tingling.
symptoms that may appear are:
- a headache and light sensitivity
- a generalized sensation of illness
- A shingles rash that covers three or more trusted Source dermatomes may appear more widely distributed in an individual with a compromised immune system.
- Physicians call this widespread zoster.
Pinched nerves.
This compression typically affects the lumbar, or lower, part of the spine, however, it can occur elsewhere along the spine.
A pinched nerve in its corresponding dermatome may cause numbness, tingling, or pain. Based on where the symptoms present, a doctor can determine which nerve is impacted.
After that, the physician determines the pinched nerve’s underlying cause, cures it, and offers suggestions for symptom relief.
Which of the following are some of the most prevalent signs of dermatome disorders?
Deviations from normalcy in the nerves or spinal cord result in disorders affecting the dermatomes. Such disruptions can result in a variety of symptoms. Three categories apply to the symptoms:
- motor (about movement).
- sensory (connected to touch).
- autonomic (about automatic bodily processes).
Motor signs and symptoms:
- weakened or paralyzed muscles.
- Uncontrollably active or ineffective muscles can move uncontrollably.
Sensory signs and symptoms:
- Pain
- tingling
- numbness
Autonomic symptoms:
Body processes known as autonomic processes operate continuously whether or not you are aware of them. These processes aid in your body’s upkeep and regulation, making them crucial. If dermatome damage compromises autonomic functioning, you may have symptoms suggesting that your body cannot naturally control processes in that region. As an example, consider:
- excessive perspiration (hyperhidrosis) or little perspiration (anhidrosis).
- bladder or bowel muscle dysfunction that impairs your ability to control when you urinate (urinary incontinence).
- Sexual dysfunction.
Which common tests are available to screen for dermatome issues?
The most popular types of testing are those that use imaging and nerve signal detection, such as:
- CT scans, or computed tomography.
- Magnetic resonance imaging (MRI) scans.
- Cisternogram scan.
- Electromyogram (EMG) tests.
The purpose
Dermatome testing is part of the neurological evaluation. They are frequently used to establish the neurologic “level” of a spinal cord injury and whether sensory loss on a limb is due to a single spinal segment.
Method:
A metal pin and cotton fabric wool are the best instruments for Dermatome testing. When the patient shuts their eyes, have them rate the various stimuli for the therapist.
- Light Touch Test – Apply a piece of cotton wool to a small patch of skin to detect a light touch feeling.
- A pinprick Examination: Pain Sensation: Ask the patient if they feel sharp or dull when gently pressing a pin against their skin.
Enquiring carefully about the pattern or distribution of sensory symptoms (such as tingling, numbness, diminished, or absent sensation) from the patient during the review of systems gives the therapist some initial information to help direct the examination and help identify the dermatome(s) and nerve(s) involved.
Compared to pain dermatomes, light-touch dermatomes are larger. In circumstances when just one or two subsections are impacted, pain sensitivity testing is a more sensitive evaluation method than light touch tests.
What therapies are available for problems associated with dermatomes?
Alternative therapies for spinal nerve disorders and associated dermatomes vary based on the underlying cause and context. A healthcare practitioner is the best person to advise you on the numerous therapies and what they propose because therapeutic options vary substantially.
What measures can I take to avoid problems and issues with my dermatomes?
Beginning with your spine is the initial step in taking care of your dermatomes because they are markers of the condition of your spinal cord and spinal nerves. Keep the options that follow details regarding your spine and spinal nerves in mind:
Wear safety equipment, such as seat belts and other restraints, as directed. Spinal injuries are frequently caused by motor vehicle incidents. Seat belts and other safety precautions can help avoid major injuries.
Lift safely. One way to prevent damage to your spinal cord and spinal nerves (like a herniated disc) is to lift using your legs rather than your back. You might need to wear a back support brace if you have a history of back issues, particularly if your profession involves a lot of lifting or if you lift weights regularly for physical activity.
Use caution when handling weapons. gunshot wounds are the main cause. No matter what, you should ALWAYS handle firearms with the finest caution. Even when you’re positive they’re not loaded, act like they are.
To prevent falls, take safety measures. When operating at an elevation, safety gear—especially safety harnesses is crucial. Additionally, you should take precautions against falls at home, particularly on staircases and in restrooms. This may entail installing handrails, using non-slip footwear and flooring, and removing potential trip hazards from the staircase.
Give your bones top consideration. Vertebral fractures can result from conditions like osteoporosis and osteopenia, which are linked to bone loss.
It matters how you position yourself. Your back is not designed to withstand the kind of strain that poor posture while standing or sitting can cause. As an illustration, consider a pinched nerve.
Summary
One spinal neuron connects each dermatome, or skin region. These regions come together to form a surface map of the body.
Damage or malfunction of the spinal nerve may be the source of symptoms in the appropriate dermatome. Nerve injury or dysfunction can be brought on by trauma, infection, or compression.
The degree and location of nerve injury can occasionally be ascertained by doctors using the intensity of symptoms in a dermatome. After that, they try to identify and address the damage’s root cause.
FAQs
What is the purpose of a dermatome?
For skin grafting, tiny skin sheets are sliced with a surgical instrument known as a dermatome. Dermatomes come in a variety of varieties. Cutting dermatomes are portable instruments that need a high degree of technical expertise and may not consistently produce accurate results.
Why do we only have thirty dermatomes?
Thirty dermatomes make up your body—one more than spinal nerves. This is due to the infrequent presence of a sensory root in the C1 spinal nerve. Dermatomes thus start with spinal nerve C2. Your body’s dermatomes are distributed in different segments.
How do dermatomes work?
Dermatomes are skin areas that are associated with certain spinal nerve roots. On the way to and from your brain, nerve traffic to these regions passes through the designated spinal nerve (as well as occasionally its neighbors).
Dermatomal pain: what is it?
For a pain pattern to be categorized as dermatomal, it must originate from the associated nerve root at the location specified in the reference sources.
Why is it vital to monitor dermatomes?
Dermatomes are valuable tools for diagnosing and evaluating a wide range of illnesses. Dermatomes can be neurologically screened to identify patterns of sensory loss that may indicate a particular spinal nerve’s involvement.
What dermatome symptoms are present?
In its corresponding dermatome, a pinched nerve may cause numbness, tingling, or pain. So, a doctor can determine which nerve is impacted by the symptoms based on where they are presenting.
References
- Professional, C. C. M. (2024a, May 1). Dermatomes. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24379-dermatomes
- Nichols, H. (2024, August 5). Shingles (Herpes Zoster). https://www.medicalnewstoday.com/articles/154912#symptoms




One Comment