Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis: What is It?
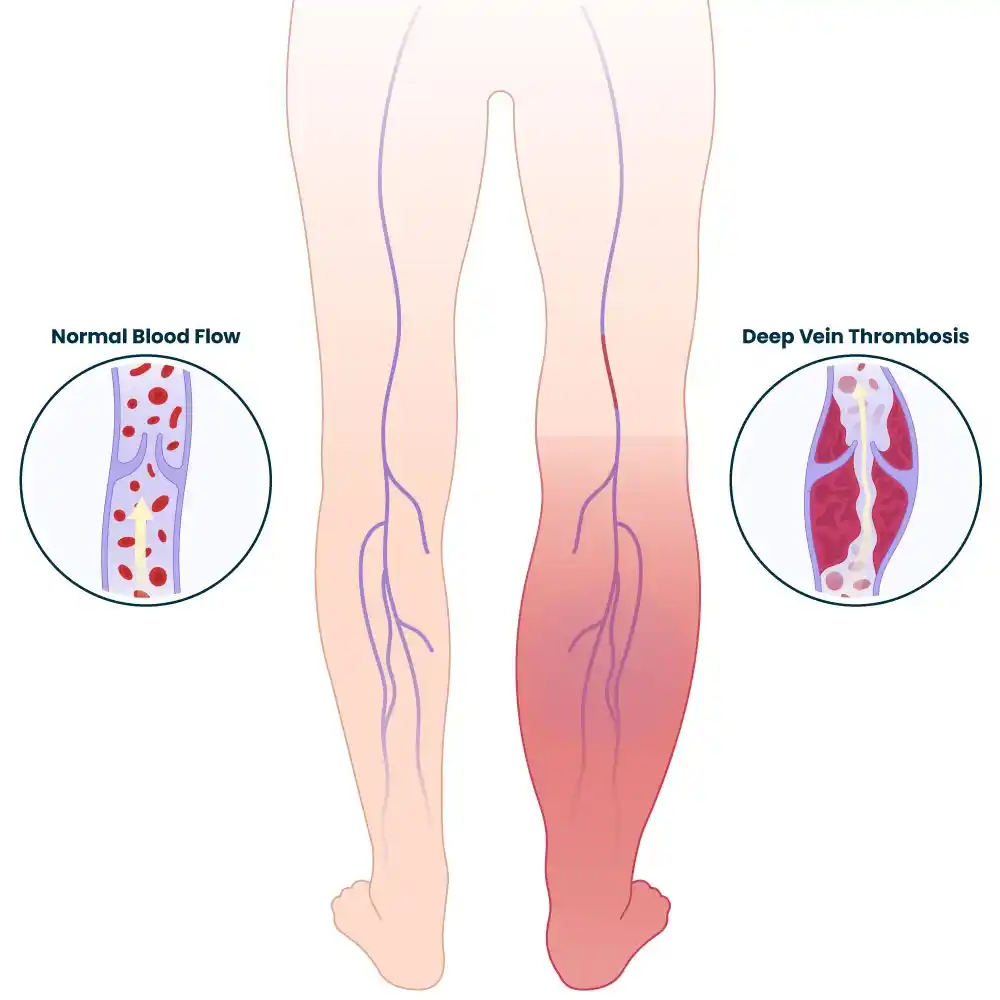
Deep Vein Thrombosis (DVT) is a condition where a blood clot forms in a deep vein, mainly in the legs. It can cause pain, swelling, and redness, though some cases are asymptomatic. If a clot breaks loose, it can travel to the lungs, causing a life-threatening pulmonary embolism (PE).
Long-term immobilization, surgery, specific medical problems, and lifestyle choices are risk factors. Prevention involves movement, hydration, and, in some cases, medication.
Your vein’s ability to carry blood may be entirely or partially blocked by the blood clots. The majority of DVTs occur in the lower leg, thigh, or pelvis, although they can also develop in the arm, brain, intestines, liver, or kidney.
How dangerous is DVT?
The blood clots may break free and move through your bloodstream, even though DVT is not a life-threatening condition in and of itself. When moving blood clots, or emboli, become stuck in your lung’s blood veins, it can cause a pulmonary embolism (PE). You need a prompt diagnosis and treatment because this ailment might be fatal.
Up to 50% of people who suffer a DVT in the legs experience sporadic limb pain and swelling, which can linger for months or even years. These symptoms, known as post-thrombotic syndrome, can occur when your veins’ inner lining and valves are damaged, causing blood to “pool” more than it should. In addition to causing discomfort and swelling, this raises the amount of pressure inside your veins.
This condition’s features include:
- A collection of blood.
- Persistent edema in the legs.
- Elevated blood vessel pressure.
- Increased skin discolouration or pigmentation.
- Venous stasis ulcers are leg ulcers.
What is the prevalence of deep vein thrombosis?
In the US, between 1 and 3 out of every 1,000 adults get a deep vein or pulmonary embolism annually, and up to 300,000 individuals lose their lives to DVT/PE. After heart attacks and strokes, it is the third most prevalent vascular disease. Although acute DVT/PE can happen at any age, it is more common in people over 60 and less frequent in children and adolescents. More than half of all DVTs occur after surgery or when a patient is in the hospital due to a medical condition. After a hospital stay, DVTs are more likely since you spend most of your time in bed rather than going around like you normally would.
Blood clots that form in a vein near the skin’s surface are known as superficial venous thrombosis, phlebitis, or superficial thrombophlebitis. Unless they first pass from the peripheral system into the deeper venous system, these blood clots hardly ever make it to your lungs. A doctor can use a physical examination to identify superficial vein clots, but only an ultrasound can identify DVT.
Deep vein thrombosis (DVT) types
- Chronic DVT
- Acute DVT
Acute DVT:
A blood clot that develops in a deep vein, typically in the thigh or lower leg, is known as acute deep vein thrombosis (DVT). It may happen unexpectedly and necessitate prompt medical care.
Signs and symptoms
- Leg pain and swelling,
- Typically in the thigh or calf
- When the foot is bent upward, the pain is worse.
Acute DVT treatment
Restoring blood flow is the aim of treatment for acute DVT. Pain and swelling usually go away after the clot is eliminated or disintegrated.
To eliminate the blood clot, Stanford offers a range of methods, medications, and equipment. A catheter, which resembles an IV, is inserted into the occluded vein during the surgery. The type of device we utilize is determined by the size and age of the thrombi.
Chronic DVT:
Any clot that is more than a month or two old is referred to as “chronic.” The vein is scarred and the clot gets harder. This process causes the vein to shrink significantly, making it difficult for blood to pass through.
Signs of persistent DVT
- Leg swelling, discomfort, and frequently skin darkening below the knee are symptoms of persistent DVT.
- In order to alleviate these symptoms, compression stockings are usually administered to these patients.
- These symptoms are caused by a blocked vein that prevents blood from leaving the leg.
Causes and Symptoms
What signs of deep vein thrombosis are present?
Usually, a DVT develops in the veins in your arms or legs. Up to 30% of DVT patients have no symptoms, though occasionally there are extremely minor ones that are not cause for alarm. Acute DVT symptoms include the following:
- Swelling in your arm or leg, which can occasionally occur all at once.
- You could only experience pain or discomfort in your arm or leg as you stand or walk..
- It’s possible that the swollen or painful part of your arm or leg is warmer than normal.
- Skin that is stained or red.
- It’s possible that the veins close to the surface of your skin are bigger than usual.
- When blood clots damage the veins deep within your belly, you may have flank or abdominal pain.
- Severe headaches, which typically appear suddenly, and/or seizures, which occur when blood clots damage the brain’s veins.
Deep vein thrombosis: what causes it?
Your chance of developing deep vein thrombosis may be elevated by certain conditions:
- The chance of blood clots is increased if you have a genetic or hereditary disorder.
- Undergoing chemotherapy and other cancer therapies.
- Having a family or individual history of deep vein thrombosis.
- Having restricted deep vein blood flow as a result of an injury, surgery, or immobilization.
- Long-term immobility following surgery or a catastrophic injury, such as sitting for extended Periods of time while traveling by car, truck, bus, rail, or airplane.
- Having recently given birth or being pregnant.
- Being over 40, even though DVTs can strike anyone at any age.
- Being obese or overweight.
- Suffering from an autoimmune condition such as inflammatory bowel disease, vasculitis, or lupus.
- Consuming tobacco products.
- Having veins that are varicose.
- Using hormone therapy or birth control tablets.
- Having a pacemaker or central venous catheter.
- Having COVID-19.
Diagnosis
How is a diagnosis of DVT made?
In addition to reviewing your medical history, your healthcare professional will perform a physical examination. Imaging tests are also required.
Diagnostic tests for DVT
The Homan’s Sign Test
A physical examination technique called the Homan’s sign test is performed to check for DVT. When combined with other clinical indicators, a positive Homan’s sign could be a rapid indicator of DVT.
John Homan established Homan’s sign test, frequently referred to as the dorsiflexion sign test, in 1941. A physical examination technique called the Homan’s sign test is used to check detect Deep Vein Thrombosis (DVT). For patient treatment, the clinical examination by itself is not sufficient. However, when done correctly, it can still be helpful in identifying whether more tests are required (such as pulmonary angiography, multidetector helical computerized axial tomography (CT), ultrasonography, and the D-dimer test).

Method
- The patient must voluntarily extend his knee in order to complete this exam.
- The examiner lifts the patient’s straight leg to ten degrees after the knee is extended, then suddenly and passively dorsiflexes the foot then squeezes the calf using the other hand.
- Tenderness and deep calf pain could be signs of DVT.
- The technique’s mechanism has been described as follows: knee flexion combined with passive and sudden ankle dorsiflexion results in mechanical pressure on the anterior tibial vein, which in turn activates lower limb pain-sensitive tissues.
Take Precaution
This examination may be risky because surgeons utilize forceful dorsiflexion on the foot to remove clots from the veins.
Typical Mistakes
The examiner frequently makes the mistake of not dorsiflexing the patient’s foot sufficiently to obtain an accurate evaluation. Additionally, the patient’s knee needs to be fully extended.
Venous duplex ultrasound: Because it is readily accessible and non-invasive, this test is the most frequently used to diagnose DVT. This test shows blood flow and clots that occur in your veins using ultrasonic waves. As they scan your arm or leg, a vascular ultrasonography technologist applies pressure. A blood clot may be present if the force of blood does not cause your vein to collapse. Your healthcare professional may employ an additional imaging test if the duplex ultrasound results are unclear.
Venography: In order to determine whether any blood clots are totally or partially obstructing blood flow within your veins, your doctor will numb the area around your neck or groin and then use a tube called a catheter to inject a particular dye (opposed material) into your veins. Nowadays, venography is rarely utilized, although occasionally it is required.
MRI stands for magnetic resonance imaging, or magnetic resonance venography: An MRI shows pictures of the inside organs and structures of your body. Images of the veins in specific body sections are displayed by MRV. More information can frequently be obtained via MRI and MRV than from a CT scan or duplex ultrasonography.
An X-ray called a computed tomography (CT) scan can reveal internal body structures: A CT scan may be used by your doctor to detect a blood clot in your lungs (pulmonary embolism) and a DVT in your brain, pelvis, or abdomen.
You could require certain blood tests if your doctor believes you might have an acquired or genetic clotting issue. This could be significant if:
Your doctor is unable to identify another reason for your history of blood clots.
You had a clot of blood in an uncommon place, like a vein in your brain, liver, kidney, or intestines.
Your family has an extensive record of blood clots.
There is a particular genetic clotting disease in your family.
Treatment
- You may initially find it more difficult to move around due to limb pain and swelling if you have a DVT. However, you will be able to gradually resume your regular activities.
- Place your heels 5 to 6 inches higher in bed if your limbs feel heavy or bloated.
- This reduces edema and enhances circulation.
Furthermore:
If you spend a lot of time sitting still, work out your calf muscles.
Every hour while awake, and particularly during a lengthy flight or road journey, get up and take a little walk.
Medical Treatment
As directed by your healthcare professional, take the drugs exactly as prescribed.
Get the blood tests your doctor prescribes, and attend all of your lab appointments on time.
Ask your doctor before beginning or stopping any medicine, including over-the-counter medications and vitamins.
Discuss your diet with your healthcare physician. According to the medication you take, you might need to adjust.
Anticoagulants, which thin the blood. This kind of drug makes blood clotting more difficult. Anticoagulants also inhibit blood clots from migrating and from growing larger. Blood clots are not destroyed or “melted” by anticoagulants. Sometimes a clot doesn’t entirely go away, but your body may dissolve it on its own. If not, they typically contract and turn into tiny “scars” inside your veins. These “old” clots frequently don’t cause any symptoms, but occasionally they might cause swelling in the legs.
Oral Xa inhibitors, heparin, and warfarin are among the various kinds of anticoagulants. The optimum kind of medicine for you will be discussed with you by your doctor.
You may be required to take an anticoagulant for a limited period of time (often three to six months) or for an indefinite period of time. Your treatment duration may vary based on each person’s unique circumstances, such as if:
Clots are nothing new to you.
You’re undergoing treatment for another disease, such as cancer or an autoimmune condition (anytime your risk of a clot is elevated, you might require the use of an anticoagulant).
The most frequent adverse effect of anticoagulants is bleeding. If you discover that you break or bleed readily while taking this drug, you should contact your doctor immediately.
- Put on compression stockings that reach your knees. If used on a daily basis, these reduce leg discomfort and edema by at least 50%.
- Avoid behaviors that could seriously hurt you.
- Always drink plenty of water, but especially when traveling.
- Deep vein thrombosis (DVT) physical therapy aims to increase blood flow and circulation.
- Additionally, it can lessen pain and swelling and stop additional clots.
Physical Therapy Treatment
Compression treatment: One way to lessen swelling and avoid blood clots is to use intermittent pneumatic compression devices or wear compression stockings.
Massage therapy can lessen muscle tension and increase circulation.
Aerobic exercises can help alleviate symptoms, such as jogging, swimming, dancing, walking, and trekking.
Exercises for range of motion: Leg stretches, ankle circles, and foot pumps can all improve blood flow and muscular strength.
Patients receive education regarding the prevention, risk factors, symptoms, and repercussions of DVT.
Additional DVT control
- Earlier mobilization
- Easy workouts
- Medicines with mechanical compression
- Changes in lifestyle, include eating a healthy weight, drinking plenty of water, and avoiding prolonged bouts of inactivity
Complication
- A pulmonary embolism (PE) occurs when a fragment of the clot separates and moves to the lungs, obstructing blood flow and possibly leading to death. Chest pain, breathing difficulties, and blood in the cough are among the symptoms.
- Chronic venous insufficiency
- A chronic illness that causes blood to collect in the veins, resulting in leg pain and swelling
- post-thrombotic syndrome
- A chronic illness that causes leg pain, edema, redness, ulcers, and sores
Prevention
How do I lower my risk?
You must lower your risk of developing another DVT or PE clot after having one by:
- following your doctor’s instructions to the letter when taking your meds.
- Maintaining your subsequent appointments with the lab and your physician. These inform your doctor about the effectiveness of your treatment.
- modifying one’s lifestyle to include things like quitting smoking, eating better, and exercising more.
If you are at a higher risk of getting a DVT but have never had one, make sure to:
- Exercise your calf muscles if you have to sit still for extended periods of time.. If you’re on a long flight, get up and take a stroll at least every 30 minutes. Alternatively, if you’re on a lengthy road trip, get out of your car every hour.
- After being ill or having surgery, get out of the bed and walk about as soon as you can. You have a lower likelihood of getting a DVT the earlier you move around.
- To lower your chance of a clot following surgery, take medicine or, if recommended by your doctor, wear compression stockings.
- To lower your chance of a clot, follow the instructions of your provider as instructed and heed their advice.
Prognosis and Outlook
If I have a deep vein thrombosis, what can I anticipate?
- Because a DVT can take weeks to a year to heal, you will need to continue taking blood thinners as prescribed and wearing stockings with compression until your doctor instructs you to stop. To ensure you’re taking blood thinners at the proper dosage, you might require blood testing. To determine whether your blood clot continues to be there, getting better, or getting bigger, your doctor might want to perform additional ultrasounds in the future.
FAQs
What is the primary cause of thrombosis in the deep vein?
One or more of the following risk factors increases your chance of developing DVT: becoming sedentary as a result of bed rest or prolonged periods of sitting still, like when traveling. A family history of thrombosis. containing a tube on a blood vessel, such as an indwelling catheter.
How can a DVT test be performed at home?
This test, called Homan’s Test, involves extending the knee of the suspicious leg while lying flat on your back. Ask a friend or relative to pinch the calf after raising the extended leg to a 10-degree angle. The presence of significant calf pain could be a sign of DVT.
Is it possible to fully heal DVT?
After beginning blood thinner medication, the majority of persons with DVT and PE will experience improvement somewhat rapidly (within days to weeks), and by three months, their symptoms will be completely resolved. As shown below, longer-term symptoms can occur in certain circumstances.
What is DVT’s last stage?
If DVT is not treated, the blood clot may rupture and travel to the lungs through the bloodstream, obstructing circulation. We refer to this as a pulmonary embolism (PE). Venous thromboembolism (VTE) is a potentially lethal and life-threatening illness that includes both PE and DVT.
For DVT, what is the first line of treatment?
Direct oral anticoagulants (DOACs) are advised as the initial line of treatment for acute PE or DVT. For the majority of patients without moderate-to-severe liver disease, antiphospholipid antibody syndrome, or severe renal insufficiency (creatinine clearance <30 ml/min), DOAC therapy is recommended over vitamin K antagonists (VKAs).
Does DVT benefit from exercise?
Exercise can also help with DVT symptoms like redness, pain, and edema. Engaging in exercise can also boost your energy levels. Being moving is especially crucial for your legs if you have DVT. Blood clots typically form there.
References
- Deep Vein Thrombosis (DVT). (2024, May 1). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16911-deep-vein-thrombosis-dvt
- Acute DVT. (2019, September 26). Stanford Health Care. https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/deep-vein-thrombosis/types/acute-dvt.html#about





One Comment