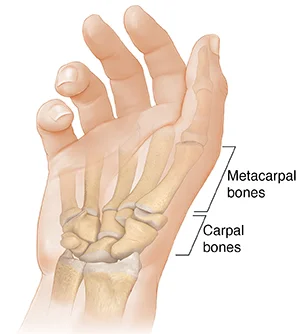
Carpometacarpal Joint
The carpometacarpal (CMC) joints are the articulations that connect the hand’s carpal (carpals) and metacarpal (metacarpals) bones. Five carpometacarpal joints are known to exist, with the thumb’s carpometacarpal joint—also referred to as the trapeziometacarpal joint—being the most specialized and flexible.
Introduction
The proximal bases of the five metacarpal bones and the distal row of carpal bones are joined by the carpometacarpal (CMC) joints, which are five wrist joints. Another name for the thumb’s CMC joint is the trapeziometacarpal (TMC) joint.
The carpal (carpo-) and metacarpal (-metacarpal) bones of the hand are joined by the carpometacarpal (CMC) joints. The thumb’s carpometacarpal joint, also known as the trapeziometacarpal joint, is the most specialized and adaptable of the five CMC joints.
Metacarpals 2, 3, 4, and 5 on the medial side and the distal row of carpal bones (trapezium, trapezoid, capitate, and hamate) on the distal side are connected by the four functional plane synovial joints that make up the remaining CMC joints. The three most medial CMC joints combine to form the common carpometacarpal joint.
The ranges of motion of the four CMC joints increase with medial movement; metacarpals 2 and 3 are nearly stationary, metacarpal 4 glides to a limited degree, and metacarpal 5 glides to the point where it produces flexion and rotation. The medial four CMC joints are exceptionally robust due to these properties, which enable a firm hold between the wrist and hand while also allowing for flexibility to support opposing movements such as palm cupping and thumb object grasping.
The CMC joints’ mobility increases from the radial to the ulnar sides of the hand as their articular surfaces grow increasingly curved.CMC joints total five in number. From the trapezium to the first metacarpal base is the first CMC joint. The second metacarpal base and the trapezoid are separated by the second CMC joint.
First Carpometacarpal Joint
The thumb (pollex) carpometacarpal joint, also referred to as the trapeziometacarpal joint (TMC), is the first carpometacarpal joint. It is necessary for the thumb’s proper function and serves as a link between the trapezium and the first metacarpal bone.
The prevalence of TMC osteoarthritis, a severely incapacitating condition, is up to 20 times higher in older women than in the overall population. The TMC is the most essential joint connecting the wrist to the metacarpus.
The pronation-supination of the first metacarpal is particularly crucial for opposition action. The capsulo-ligamentous complex surrounding the joint, the form of the joint, and the balance of the participating muscles limit the first CMC’s range of motion. First CMC joint subluxation (slight displacement) towards the radius is common if the first metacarpal does not sit correctly “on the saddle,” as in the case of hypoplasia.
Although the capsule reinforces ligaments and tendons to give joint stability, it is sufficiently slack to permit a wide range of motion and a 3 mm distraction. On the dorsal side compared to the ventral side, it is marginally thicker. Most postmenopausal women have osteoarthritis of the first carpometacarpal joint.
Type
Concavoconvex articular surfaces give rise to saddle type of synovial joints.
Articular Surfaces
- The trapezium’s distal surfaces
- first metacarpal bone’s proximal portion.
Concave in the sagittal plane and convex in the frontal plane are the articulating surfaces of trapeziums.
The articular surfaces’ concavoconvexity permits a broad range of motion.
Ligaments
There are significant differences in the anatomical literature on the number and nomenclature of the first CMC’s ligaments. The thumb is stabilized primarily by three intracapsular and two extracapsular ligaments.
Anterior oblique ligament (AOL)
A robust, thick intracapsular ligament that begins on the palmar tubercle of the trapezium and terminates on the palmar tubercle of the first metacarpal. According to certain reports, it has a significant retention function and is either absent or extended in CMC joint arthritis. Abduction, extension, and pronation all exhibit rigidity.
Ulnar collateral ligament (UCL)
An extracapsular ligament that extends nearly to the AOL is called the UCL. It is placed on the ulnopalmar tubercle of the first metacarpal after starting on the flexor retinaculum. It is often extended when CMC joint arthritis is present and is taut in abduction, extension, and pronation. Researchers differ widely about the UCL’s significance.
First intermetacarpal ligament(IML)
This ligament attaches to the ulnopalmar tubercle of the first metacarpal, where its fibers converge with those of the UCL, and joins the bases of the second and first metacarpals. It is taut during opposition, abduction, and supination.
It was the primary restraining structure of the original CMC joint, according to several researchers. Although some people think it isn’t strong enough to maintain the joint by itself, when paired with the UCL, it serves as a crucial restraining component.
Posterior oblique ligament (POL)
An intracapsular ligament called the posterior oblique ligament (POL) connects the dorsal side of the trapezium to the ulnar-palmar tubercle of the first metacarpal. Although it tightens during forceful adduction and radial abduction, it is not a crucial ligament for the first CMC joint.
Dorsoradial ligament (DRL)
Similar to the previous ligament, the DRL has no bearing on the initial CMC. The trapezium’s dorsal and first metacarpal sides have a connection it.
Relations
- Anteriorly: The joint is protected by the thenar eminence muscles.
- Posterior: The long and short extensors of the thumb are situated
- Medially: the radial artery and the first dorsal interosseous muscles
- Laterally: The abductor pollicis longus tendon
Movements
Flexion
- Opponents policies
- Flexor pollicis brevis
- Flexor pollicis longus
Extension
- Abductor pollicis longus
- Extensor pollicis longus
- Extensor pollicis brevis
Abduction
- Abductor pollicis longus
- Abductor pollicis brevis
Adduction
- Adductor pollicis
- Extensor pollicis longus
Opposition
The thumb pulp moves over the palm to get closer to the digit pulps.
When the thumb is simultaneously abducted, flexed, and pronated, opposition is created.
Retroposition
In both ulnar adduction and extension, the thumb pulp is raised.
extensor pollicis longus
Circumduction
Circumduction is the result of extension, abduction, flexion, and abduction occurring one after the other (or the opposite).
Circumduction, opposition, abduction, and adduction in a plane perpendicular to the palm, and flexion and extension in the palm’s plane are all allowed. The movement of opposition causes the thumb’s tip to make contact with the volar surfaces of the slightly bent fingers. A modest sloping facet on the anterior lip of the saddle-shaped articular surface of the greater multangular allows for this mobility. The Adductor muscles carry out the opposite movement, while the Flexor muscles pull the matching portion of the metacarpal bone’s articular surface onto this facet.
With help from the Opponens pollicis and Adductor pollicis, the Flexores pollicis longus and brevis bring this joint into flexion. The extension is mostly accomplished by the abductor pollicis longus, with support from the extensor pollicis longus and brevis. The Adductor is responsible for adduction, while the Abductores pollicis longus and brevis, with the help of the Extensors, are principally responsible for abduction.
Joint Capsule
There is a distinct synovial membrane surrounding the fibrous joint capsule.
Arterial supply
The anterior interosseous artery and the posterior carpal branches of the radial and ulnar arteries supply blood to the carpal joints.
The radial artery’s dorsal metacarpal branch.
Innervation
Lateral antebrachial cutaneous nerve
Palmar cutaneous branch of the median nerve.
Superficial radial nerve
Second to fifth carpometacarpal joints
Articular surfaces
The CMC joints connect the surfaces of the metacarpal bases of the medial four metacarpal bones to the distal surfaces of the four distal carpal bones.
The second metacarpal bone, trapezium, trapezoid, and capitate appoint to form the second CMC joint. A flat, quadrilateral bony protrusion (facet) that links to another quadrilateral facet on the base of the second metacarpal is directed medially by the distal part of the trapezium. The trapezoid’s distal surface is triangular and concave coronally, ‘cupping’ a concave groove on the base of the second metacarpal. It is convex in the transverse plane. The concave, anterolateral corner of the capitate bone is articulated with a deep ridge situated medially to this groove. The second CMC joint is unique in these features since it is the only one in which the articulation is formed by three carpal bones.
The third metacarpal bone and the capitate make up the third CMC joint. The triangular and primarily concave distal aspect of the capitate articulates with a convex facet on the metacarpal base.
Together with the hamate and fourth metacarpal bones, the capitate bone contributes to the formation of the fourth CMC joint. This capitate’s anteromedial corner develops an articulating facet in the direction of a sizable, oval dorsal facet on the base of the fourth metacarpal. On the distal aspect of the hamate bone, a tiny, anterolateral facet meets the somewhat convex and concave quadrangular proximal surface of the metacarpal base.
The fifth CMC joint is formed in part by the fifth metacarpal bone and the adjacent bigger, anteromedial facet on the same distal surface of the hamate. This metacarpal base gets attached to the hamate by a laterobasal surface that is coronally convex and transversely concave. This transition from concave to convex is not sharp; rather, it slopes almost smoothly downward. The articular surface of the hamate bone has a beveled edge that allows the fifth CMC joint to move more freely than the other CMC joints.
The four CMC joints are flat (non-planar) based on the specifications given above. Certain surfaces can be concave, convex, or both, but some are nearly flat. Certain surfaces can be concave, convex, or both, but some are nearly flat. They therefore resemble sophisticated saddle synovial joints or ellipsoid joints physically. The CMC joints are functionally classified as plane synovial joints because of their tiny curvatures, which are typically ignored.
Ligaments
The dorsal carpometacarpal ligaments, palmar carpometacarpal ligaments, and interosseous ligaments are the three types of ligaments that connect the CMC joints. The fibrous joint capsule that envelops the CMC joints thickens to form these soft tissue formations.
Dorsal carpometacarpal ligaments
The CMC joints are largely supported by the strongest ligaments, the dorsal carpometacarpal ligaments, which are situated on the dorsal side of the hand. They consist of four medial metacarpal bases and seven ligamentous bands that extend obliquely between the dorsal surfaces of the distal row of carpal bones.
Both metacarpals 2, 3, and 4 are given two bands: the capitate and hamate for metacarpal 4, the trapezium and trapezoid for metacarpal 2, and the trapezoid and capitate for metacarpal 3.The fifth metacarpal is unique in that the hamate bone only gives it one ligamentous band. The equivalent palmar carpometacarpal ligament is connected to this band to produce an incomplete capsule.
Palmar carpometacarpal ligaments
Palmar carpometacarpal ligaments are found on the palmar portion of the hand and resemble their dorsal counterparts in many ways. With three ligamentous bands—one medial from the hamate, one intermediate from the capitate, and one lateral from the trapezium/trapezoid—the third metacarpal base is the only exception.
Interosseous ligaments
The CMC joints’ smallest stabilizers are the interosseous ligaments. These structures separate the third and fourth metacarpal bases and the inferior portion of the capitate and hamate bones’ distal edges by two thick, fibrous bands.
These bands may be joined proximally or entirely. The capitate and the third metacarpal base are connected by the lateral band and the fourth metacarpal base by the medial band, respectively, if they are separated. The CMC joint space can also occasionally be separated into medial and lateral compartments by the medial interosseous ligament, which forms a distinct synovial cavity between the hamate and the fourth and fifth metacarpal bones.
Movement
The four CMC joints are all synovial based on their structural composition. Their functional classification, degrees of freedom, ranges of motion (ROM), and articular surfaces, however, separate them into two groups. The latter gradually rises as one moves medially over the four CMC joints.
The range of motion of the second to fifth carpometacarpal joints increases from the radial to the ulnar side. Small gliding motions are produced at these joints by the contraction of the long flexor and extensor digitorum muscles. The opponens digiti minimi can contract to induce flexion and lateral rotation at the fifth carpometacarpal joint, which makes it possible to do palm “cupping.”
Muscles acting
There is no direct muscle activity required to move the four medial CMC joints. The muscles that affect joint translational movements, however, are the flexor digitorum profundus and extensor digitorum. The fourth and fifth CMC joints experience flexion and extension, respectively, as a result of the indirect gliding action of these antagonistic muscles on the phalanges.
The isolated exception is the opponent’s digit minimise direct participation in the fifth CMC joint’s rotating movement. The muscle brings the fifth finger to the palm when it is in an agonistic position, externally rotating it and hollowing the palm. Adductor pollicis, opponens pollicis, flexor pollicis brevis, and abductor pollicis brevis are the muscles that oppose and smoothly govern the opponens digiti minimi. Together, the flexor digiti minimi, abductor digiti minimi, and palmaris brevis support the joint when moving.
Several soft tissue structures are connected to the four medial CMC joints. The flexor digitorum superficialis, flexor digitorum profundus, flexor carpi radialis (lateral), and flexor carpi ulnaris (medially) are among the muscles whose tendons cover the CMC joints on the palmar aspect of the hand. Additionally, the hypothenar muscles cover the medial CMC joints superficially.
On the dorsal side of the hand, near the tendons of the extensor forearm muscles, are the CMC joints. Extensor carpi ulnaris, extensor pollicis longus, extensor digitorum, extensor digiti minimi, extensor carpi radialis longus, and extensor carpi radialis brevis are a few examples.
Joint capsule
A shared fibrous capsule envelops and stabilizes the four CMC joints. A synovial membrane that lines this fibrous capsule secretes viscous synovial fluid, which serves as a lubricant. The synovial membrane is normally continuous with the lining of the intercarpal joints.
The midcarpal and intermetacarpal joint spaces are connected to the proximal and distal extensions of the joint cavity of the CMC joints, respectively. CMC joints are lined with hyaline cartilage on their articular surfaces.
Arterial supply
- Posterior carpal branch of the radial artery
- Posterior carpal branch of the ulnar artery
- Anterior interosseous artery
Innervation
- Dorsal ulnar nerve
- Anterior interosseous nerve
- Superficial radial nerve
Blood supply of carpometacarpal joints
The palmar and dorsal carpal anastomotic arches give blood to the CMC joints. These are created when the radial artery’s palmar and dorsal carpal branches unite.
Synovial membranes of carpometacarpal joints
The intercarpal joints’ membrane continues onto the synovial membrane. There are instances where the hamate and the fourth and fifth metacarpal bones form a joint with a distinct synovial membrane.
There are five synovial membranes in the wrist and carpus, as may be seen:
- The lower end of the ulnar muscle connects to the ulnar notch of the radius muscle, and it runs along the upper surface of the articular disk.
- The second connects the first row of bones below to the articular disk and the lower end of the radius above.
- The third, and longest, connects the contiguous margins of the two rows of carpal bones. If an interosseous ligament is missing, it can also connect the second row’s bones to the carpal extremities of the second, third, fourth, and fifth metacarpal bones.
- Starting from the edge of the larger multangular, the fourth one reaches the thumb’s metacarpal bone.
- The fifth connects the pisiform and triangle bones’ neighboring edges.
Occasionally, there is a distinct synovial membrane at the fourth and fifth carpometacarpal joints.
For the wrist and carpal joints to operate smoothly and to be lubricated, these synovial membranes are essential.
Clinical significance
The degeneration of both the joint cartilage and the underlying bone is a defining feature of osteoarthritis of the carpometacarpal joints. In particular, it is called trapeziometacarpal osteoarthritis when it involves the thumb.
The development of a tiny, fixed projection over the joint is known as carpometacarpal bossing. The formation of an immovable prominence in the carpometacarpal area is referred to by this word.
The affected joints may experience pain, stiffness, and decreased mobility as a result of these diseases, which frequently influence daily activities and hand function.
Summary
The distal row of carpal bones and the proximal bases of five metacarpal bones are joined by the carpometacarpal (CMC) joints, which are five wrist joints. The trapeziometacarpal (TMC) joint, the first CMC joint, is more common in older women and is necessary for appropriate thumb function.
The first dorsal interosseous muscles, the radial artery, the long and short extensors of the thumb, the thenar eminence, and two extracapsular ligaments are all covered by the first CMC joint. Three types of carpometacarpal ligaments—dorsal, palmar, and interosseous—maintain the stability of the CMC joints.
Despite having synovial motion, the CMC joints are classified into two categories based on their articular surfaces, degrees of freedom, and ranges of motion. The flexor digitorum profundus and extensor digitorum muscles have an indirect effect on the four medial CMC joints. On the dorsal part of the hand, near the tendons of the extensor forearm muscles, are the CMC joints.
FAQs
The most movable carpometacarpal joint is which one?
The thumb’s carpometacarpal joint (pollex), also known as the first carpometacarpal joint or the trapeziometacarpal joint (TMC), is an essential component of the thumb’s normal function because it connects the trapezium to the first metacarpal bone.
At what types of movements does the carpometacarpal joint move?
The CMC joint can move in all directions, including flexion, extension, adduction, and abduction. When combined, these motions enable intricate thumb actions like adduction, palmar and radial abduction, opposition, and retropulsion.
Where is joint discomfort associated with CMC?
The base of the thumb hurts as a result of the wear and tear on that CMC joint in particular.
What is the CMC’s weakness?
A frequent degenerative illness that significantly impairs function and causes morbidity is osteoarthritis of the thumb carpometacarpal (CMC) joint. Hand weakness is common in patients with early-stage CMC OA when they pinch, grab, or twist objects.
How big is the carpometacarpal joint?
Due to its small stature, the carpometacarpal joint is suitable for code 20600, Arthrocentesis, aspiration, and/or injection, small joint or bursa (e.g., fingers, toes); without ultrasound guidance.
Is the carpometacarpal a saddle joint?
A wide range of motion (ROM) is made possible by the thumb’s carpometacarpal (CMC), a saddle joint that is primarily responsible for the typical agility of human comprehension. Throughout life, this joint, which is found at the very base of the thumb, is consistently under a lot of physical strain.
References:
- Vaghela, D. (2023, December 13). Carpometacarpal Joint – Anatomy, Structure, Function. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/carpometacarpal-joint/
- January 21, 2024: Goswami, K. Carpometacarpal joints (CMC joints): All the Information You Need. Physiotherapy Clinic of Samarpan. CMC joints: https://samarpanphysioclinic.com/carpometacarpal-joints/
- Carpometacarpal (CMC) joints. (2023, July 5). Kenhub. https://www.kenhub.com/en/library/anatomy/carpometacarpal-cmc-joints
- Wikipedia contributors. (2024a, May 22). Carpometacarpal joint. Wikipedia. https://en.wikipedia.org/wiki/Carpometacarpal_joint



One Comment