Atelectasis
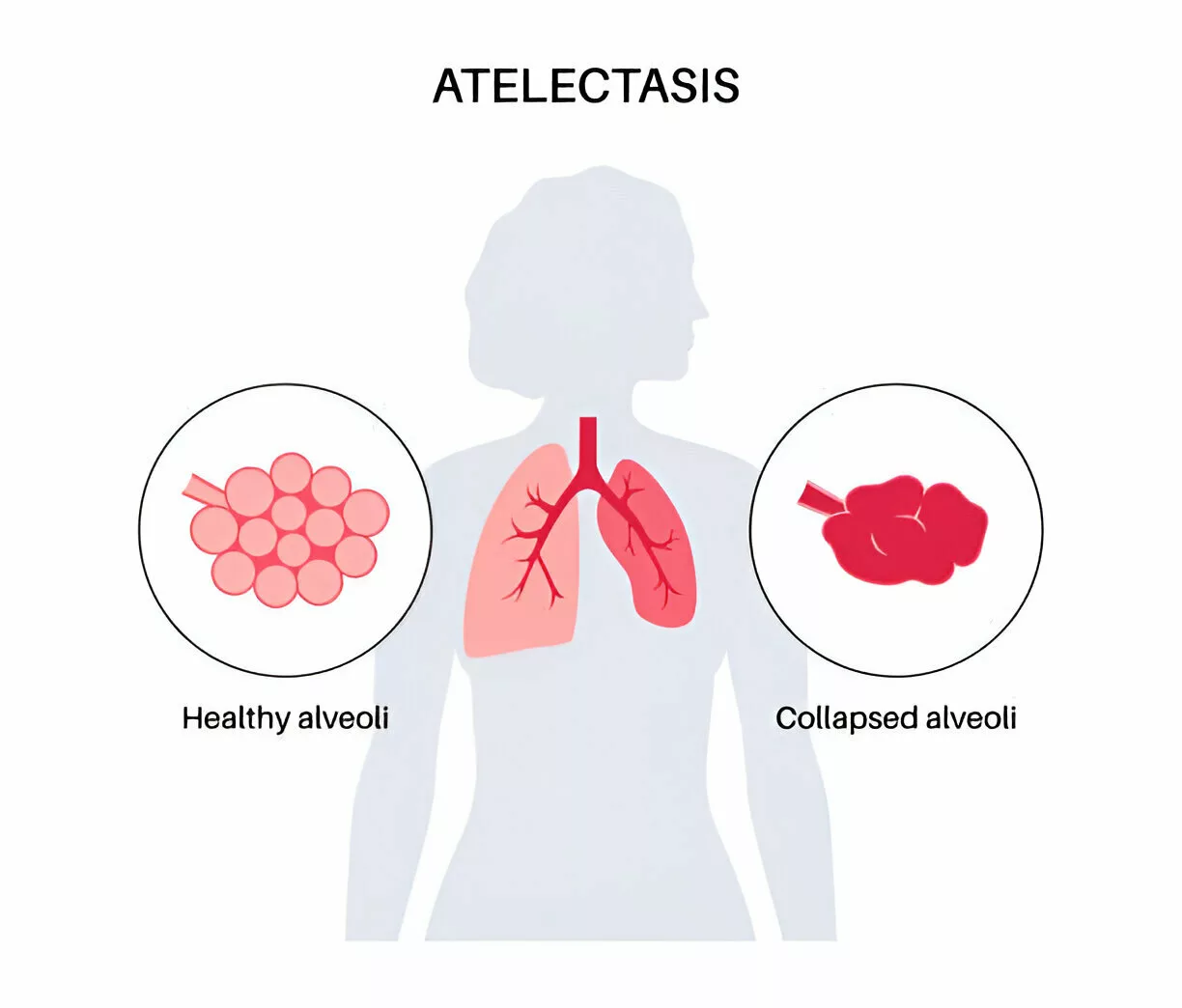
What is an Atelectasis?
Atelectasis is a condition in which a portion of the lung collapses or fails to inflate properly, leading to reduced gas exchange. It commonly occurs due to airway obstruction, pressure on the lung, or shallow breathing, often after surgery or in individuals with underlying lung conditions.
Although it normally only involves a partial collapse, it is frequently referred to informally as a collapsed lung. This inaccurate word is also used informally to refer to a fully collapsed lung caused by a pneumothorax.
It can be caused by a variety of medical disorders or by a normal exhale and is a very common finding in chest X-rays and other radiological investigations. Pneumothorax is a more specific condition that can produce atelectasis, but it is not the same as atelectasis, which is often defined as a collapse of lung tissue.
Acute atelectasis can be caused by a lack of surfactants or as a consequence of surgery. This causes infant respiratory distress syndrome in preterm infants.
Your lungs fill with air when you breathe in. The oxygen enters your blood stream through the alveoli, which are sacs in your lungs. Your body’s organs and tissues receive oxygen from the blood.
If your alveoli aren’t getting enough air to fill them or if outside forces are compressing them, they may collapse (atelectasis). Atelectasis may develop in the entire lung or just a small area of it. If enough of your lung is damaged, your blood may not receive enough oxygen, which could result in health issues.
Symptoms may include shortness of breath, chest pain, or coughing. Treatment focuses on addressing the underlying cause and may involve breathing exercises, physiotherapy, or medical intervention.
Who is at risk for atelectasis?
Your chance of developing atelectasis is increased if you have:
- Abdominal or chest surgery that prevented you from taking deep breaths because you needed medicine to keep you calm or drowsy (anesthesia).
- A disorder that stops your lungs’ tiny airways, called branches, from expanding normally.
- A rib fracture or chest injury hurts a lot. You might not be able to breathe deeply because of this.
- Been exposed to smoke.
Epidemiology
Neither species is disproportionately affected by atelectasis.
Patients with COPD, asthma, or advanced age do not have an elevated incidence.
Up to 20–25% of normal lung tissue is observed to be either weakly ventilated or atelectatic on CT during anesthesia, and the prevalence of atelectasis in individuals who have just undergone general anesthesia can reach 90%.
It is frequently seen as a side effect in individuals recovering from surgery whose breathing system is affected by the operation, discomfort, and extended periods of inactivity.
Patients with cystic fibrosis, bronchiectasis, and COPD are less likely to get atelectasis.
Atelectasis is more prone to occur in people who are obese or pregnant due to cephalad displacement of the diaphragm. Both normal and overweight patients showed an increase in atelectasis as their BMI increased.
Pathophysiology
Compression of Lung Tissue: The alveoli collapse when the net forces acting on the alveolar wall are not balanced. The lung tissue compresses as a result of this atelectasis mechanism.
Air Absorption in the Alveoli: Gas resorption is a second important factor. This can occur in one of two ways.
- A total blockage of the airway might result in atelectasis since the alveolar gas can only leave the body through the circulation and not the alveolar unit.
- The ventilation/perfusion mismatch in specific lung regions may be the cause of the second, and possibly more significant, process of gas resorption. Reduced lung capacity and less alveolar splinting will result from high absorption if the alveolar oxygen rises due to the higher inspired oxygen concentration while the nitrogen does not.
Deterioration of Surfactant Activity: Surfactant capacity may be limited due to acquired malfunction (e.g. in premature infants). By lowering alveolar surface tension, surfactant stabilizes and keeps alveoli from collapsing.
- Increased local surface tension can result in less alveolar expansion when inactivated, which lowers the resting lung volume worldwide.
Types of Atelectasis
There are mainly three forms:
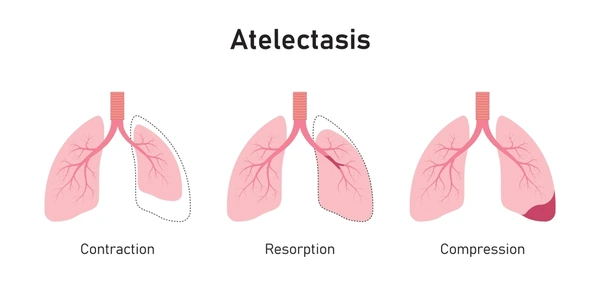
- Resorptive (obstructive),
- contraction, and
- compressive atelectasis
Compressive atelectasis
When something presses against your lung, such as fluid, air, blood, or a tumor, it can cause compression atelectasis, which results in the lung collapsing.
Obstructive/resorptive atelectasis
When the carbon dioxide and oxygen in your alveoli enter your bloodstream without any fresh air entering, you have resorptive atelectasis. Your alveoli collapse as a result. Resorptive atelectasis is frequently caused by anesthesia-requiring surgery.
Resorptive atelectasis can also be caused by something obstructing the inside of your lung, preventing air from entering the alveoli. The obstruction, which is also known as obstructive atelectasis, may be mucus, a tumor, or something you inhaled by accident.
Contraction atelectasis
Contraction atelectasis is caused by lung scarring or fibrosis. Leaving scars prevents the alveoli from opening correctly.
Additional forms of atelectasis
Patchy atelectasis is a rare form of atelectasis that can occur in neonates, especially premature newborns, or in patients suffering from acute respiratory distress syndrome (ARDS). When your lungs don’t contain enough surfactant, a protein that keeps them from collapsing, you get patchy atelectasis.
The location, appearance, or severity of the collapse are described by several forms of atelectasis, such as sub segmental atelectasis, rounded atelectasis, gravity-dependent atelectasis, and bibasilar atelectasis.
Rounded atelectasis: The pleura, the membrane layers that protect the lungs, shrinks and scars in rounded atelectasis (also known as folded lung or Blesovsky syndrome), causing visceral pleural thickening and lung tissue trapping.
This causes the outer part of the lung to gradually collapse. On X-rays, this creates a rounded appearance that medical professionals can mistake for a tumor.
Rounded atelectasis is typically a consequence of asbestos-induced pleural illness, but it can also be caused by other chronic pleural thickening and scarring conditions.
Patterns of Collapse
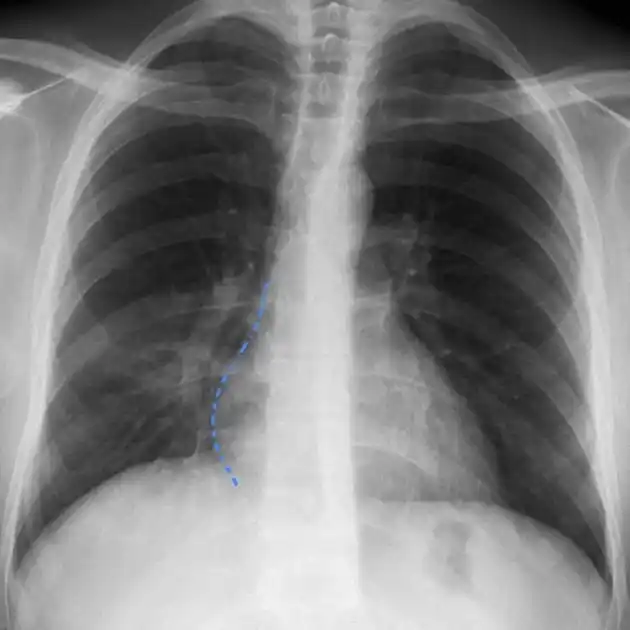
Atelectasis can be grouped based on radiological patterns of collapse.
Complete Collapse
Complete lung collapse is characterized by the whiteout or total opacification of a hemithorax. The mediastinal shift toward a collapsed lung helps differentiate this appearance from a massive pleural effusion, even though the pathology’s motion is in the opposite direction.
Lobar Collapse
Individual lobar collapse is associated with the following characteristics:
Right upper lobe (RUL) collapse

- Elevation of the right hilum
- The small fissure is elevated.
- The lateral view may show both minor and significant fissures.
- The minor fissure is typically convex superiorly. This is why the golden S sign is present.
Right middle lobe (RML) collapse
- Produces little opacity and is frequently overlooked.
- The loss of the right heart border’s outline is visible in a posterior-anterior view.
- On the lateral view, the oblique and right horizontal fissures are moving in the direction of one another, creating a wedge-shaped opacity.
Right lower lobe (RLL) collapse

- The right heart border is visible along with triangular opacity.
- The obliteration may cause the right hemidiaphragm to appear raised.
- The border of the right heart is visible.
- The lateral view shows denser lower thoracic vertebrae and a loss of the right hemidiaphragm form posteriorly.
Left upper lobe (LUL) collapse
- It extends from the hilum and disappears inferiorly, giving the appearance of a veil-like opacity due to the lack of a small fissure.
- On the lateral view, the lower lobe seems hyper-expanded, and the major fissure is moved anteriorly.
- There is a hyper-expanded superior segment of the left lower lobe, known as the Luftsichel sign.
Left Lower Lobe (LLL) collapse
- The left hemidiaphragm is shadowed by increased retrocardiac opacity.
- The lateral view shows denser lower thoracic vertebrae and a loss of the left hemidiaphragm outline posteriorly.
Signs and symptoms
What signs of atelectasis are present?
Although atelectasis itself often has no symptoms, some underlying conditions that cause it, like COPD, may cause symptoms.
If you have atelectasis that affects a lot of lung tissue, your blood oxygen level may drop (hypoxemia).
This may leads to:
- Dyspnea,
- Coughing;
- Chest discomfort,
- Rapid breathing (tachypnea),
- Lips and skin become blue.
Causes
What causes atelectasis most frequently?
The most frequent cause of atelectasis is surgery. You don’t cough to remove mucus from your lungs or breathe deeply enough to fill them completely when anesthesia is used to keep you sleeping during surgery. Resorptive atelectasis may result from airflow obstructions or shortages in the alveoli.
Other causes for atelectasis include:
- Mucus plug: Mucus accumulation is prevalent in children, people with cystic fibrosis, following surgery, and during severe asthma episodes.
- Item inhaled: Children are especially susceptible to lung blockages caused by unintentionally inhaling small food or toy items.
- Pleural effusion is fluid surrounding the lungs. Pleural effusion is typically the result of an underlying sickness, such as heart disease.
- Pneumothorax,
- Benign growths,
- Malignant growths,
- Lung scarring.
- Underlying disease: Atelectasis can result from respiratory infections such as COVID-19 or pneumonia, as well as illnesses like acute respiratory distress syndrome (ARDS) or chronic obstructive pulmonary disease (COPD).
Prevention
How can I lower my atelectasis risk?
Here are a few strategies to lower your chance of developing atelectasis:
- Following surgery, follow your doctor’s instructions to get up and move around, practice breathing techniques, and use an incentive spirometer.
- If you have any underlying medical disorders that can lead to atelectasis, treat those conditions according to your doctor’s advice.
- Avoid smoking or give it up.
- Children are less likely to inhale little things if they are kept away from them.
Testing and Diagnosis
How can atelectasis be diagnosed?
The first step in diagnosing atelectasis is a chest X-ray, which is a picture of your lungs. If required, your doctor may do a computed tomography (CT) scan to obtain more precise images.
In certain instances, your healthcare provider may do a bronchoscopy, which involves examining the inside of your lungs with a tiny camera connected to a tube that passes down your neck.
Bronchoscopy: A flexible, illuminated tube is inserted down your throat for this procedure. It enables your physician to determine the possible cause of a blockage. Tumors, foreign bodies, or mucus plugs are among the potential causes. Blockages may also be removed with this test.
Oximetry: This test measures your blood oxygen level by placing a tiny device on one of your fingertips. It helps in determining the severity of atelectasis
Chest ultrasound: Sound waves are used in this examination to provide detailed pictures of the structures inside your chest. To take the pictures, a tiny, handheld device is placed on your chest and moved as necessary. Two of the causes of atelectasis that it can detect are pleural effusion, where fluid develops in and around the lungs, and pneumothorax, where air flows into the space between the lungs and the chest wall.
Treatment
Treatment are as follows:
Surgery
Airway obstructions can be removed by bronchoscopy or suctioning mucus. During a bronchoscopy, the doctor carefully inserts a flexible tube down your neck to clear your airways.
If a tumor is producing atelectasis, surgery may be necessary to remove or reduce the tumor during the bronchoscopy. There may or may not be a need for additional cancer therapies like radiation or chemotherapy.
Physical therapy Treatment
Various physical therapy interventions have been shown to be helpful in the resolution of atelectasis; physical therapy treatment can also be used as a preventative measure before surgery.
The management of atelectasis depends on the duration and severity of the condition; non-invasive intervention (chest physical therapy and pharmaceutical agents) and invasive treatment (bronchoscopy) can be chosen according to the individual’s state of health.
Airway clearance techniques
- Suctioning.
- Percussion and vibration therapy.
- Positive expiratory pressure.
- Active cycle of breathing technique.
- Postural drainage.
- Chest high-frequency oscillations (CHFO) using the Metaneb System.
- Manual lung hyperinflation.
Breathing exercises
- Incentive spirometry
- Sustained maximal inspiration
- Intermittent positive pressure breathing
Positioning
- Kinetic Therapy: It is described as the continual rotation of a patient slowly along the longitudinal axis to ≥ 40° onto each side, utilizing a specific bed.
- Turning side to side
- Prone positioning
Early mobilization
- Sitting out of bed
- Standing on the first postoperative day,
- Walking a little distance on the second postoperative day within the room or corridor.
FAQs
Why does atelectasis occur?
A obstruction of the airways (bronchus or bronchioles) or pressure on the lung’s exterior can result in atelectasis.
Which drug works best for atelectasis?
Albuterol (Ventolin, Proventil)
The majority of patients benefit from treatment, even if there is no discernible increase in expiratory flow. Initially, inhaled beta-agonists are prescribed “as needed” only.
Is atelectasis self-healing?
The lung may naturally re-inflate after a minor pneumothorax or mild atelectasis has healed. If not, there are numerous methods for expelling air from the lungs, eliminating blockages, and promoting lung healing. Your doctor could advise chest percussion to break up mucus plugs in the airway if you have atelectasis.
What is the duration of atelectasis?
With the right care, atelectasis usually goes away in a day for most patients. On the other hand, atelectasis might cause fatal consequences if treatment is not received.
What kind of gas is utilized to stop atelectasis?
The early development of atelectasis may be avoided by using a gas combination that contains a gas that is poorly absorbed, like nitrogen, during the induction of anesthesia.
Can atelectasis be treated with antibiotics?
If a blockage has caused the lung to collapse, bronchoscopy, suctioning the airways, or coughing can all be used to clear the obstruction. An infection can be treated using antibiotics. If severe bleeding happens or persistent infections become fatal, surgery to remove a portion of the lung may be required.
How dangerous is atelectasis?
Collapsed airways can become infected with mucus. respiratory malfunction. Respiratory failure, which is potentially fatal, can result from severe occurrences of atelectasis, such as the collapse of a whole lung.
Does atelectasis improve with walking?
Exercise, such as walking, is a preferred method of encouraging deep breathing in ambulatory individuals. Continuous positive airway pressure may be beneficial for patients without significant secretions and without intubation.
Reference
- Atelectasis. (2024, December 19). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17699-atelectasis
- Atelectasis – Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/atelectasis/symptoms-causes/syc-20369684#:~