Charcot Neuropathic Osteoarthropathy(CN)
Introduction
Charcot Neuropathic Osteoarthropathy (CN) is a progressive condition affecting the bones, joints, and soft tissues of the foot and ankle, often seen in individuals with peripheral neuropathy, like diabetes. It leads to weakening of the bones, fractures, joint dislocation, and deformities if untreated. Early diagnosis and management are crucial to prevent severe complications.
The increased stresses across the joints. Patients may not be aware of it, but abnormal sensation can lead to repetitive micro-trauma to the foot and ankle. The increased stresses across the joints can lead to joint collapse or even fracture. This is linked to a rise in blood circulation to the affected region, which can lead to additional damage to bones and joints.
Charcot neuropathic osteoarthropathy is a joint disorder characterized by destruction and triggered by trauma to a neuropathic extremity. This may lead to fractures and dislocations in the foot. It is essential to accurately diagnose and treat acute Charcot to reduce the risk of lasting foot deformity and to ensure the development of a stable, plantigrade foot that can support walking. This task emphasizes the importance of the interprofessional team in managing patients with Charcot neuropathic osteoarthropathy.
Goals:
- Describe the histopathological features of Charcot arthropathy.
- Examine the history and physical examination of a patient suffering from Charcot arthropathy.
- Summarize the available treatment and management options for Charcot arthropathy.
- Summarize why enhancing care coordination among interprofessional team members is crucial for better outcomes in patients with Charcot arthropathy.
Without timely treatment, Charcot foot can lead to joint collapse in your foot and have lasting consequences for its functionality. It can also increase the chances of a foot infection worsening or expanding through your body. This can result in the necessity of a foot amputation or lead to complications that endanger life, particularly in severe cases.
To prevent Charcot foot, it is crucial to have regular checkups with a healthcare provider and to inspect your feet for any loss or alteration in your ability to perceive touch, pain, or pressure.
Some alternative names that healthcare providers use instead of Charcot foot include:
- Diabetes-related foot.
- Charcot arthropathy.
- Charcot neuropathy.
What does Charcot arthropathy refer to?
Charcot arthropathy, referred to as Charcot neuroarthropathy or Charcot foot and ankle, is a syndrome affecting individuals with peripheral neuropathy or loss of sensation in the foot and ankle. Patients can suffer from bone and joint fractures and dislocations even with minimal or no identifiable trauma.
Epidemiology
Reports indicate that Charcot affects 0.1% to 0.9% of individuals with diabetes. Approximately 63% of individuals suffering from Charcot neuropathic osteoarthropathy will go on to develop a foot ulceration. High body mass index was found to be significantly associated with Charcot arthropathy.
Pathogenesis
Any condition that leads to a reduction in peripheral sensation, proprioception, and fine motor control:
- Diabetes mellitus neuropathy, which is currently the most common in the U.S. and leads to the destruction of foot and ankle joints, affects Charcot joints in 1 out of 600–700 diabetics, connected to chronic hyperglycemia.
- Alcoholic neuropathy
- Cerebral palsy
- Leprosy
- Syphilis (Tabes dorsalis), which is caused by the Treponema pallidum organism
- Spinal cord injury
- Myelomeningocele
- Syringomyelia
- Intra-articular steroid injections
- Congenital insensitivity to pain
- Peroneal muscular atrophy
Stages of Charcot neuropathic
Stage One: Fragmentation and destruction
- During this acute stage, the foot and ankle will exhibit redness, swelling, and heat.
- Internally, there are emerging signs of minor bone fractures and soft tissue swelling. The joints and adjacent bone are thereby destroyed. This causes instability in the joints, potentially leading to dislocation. The bones can completely soften and become gel-like.
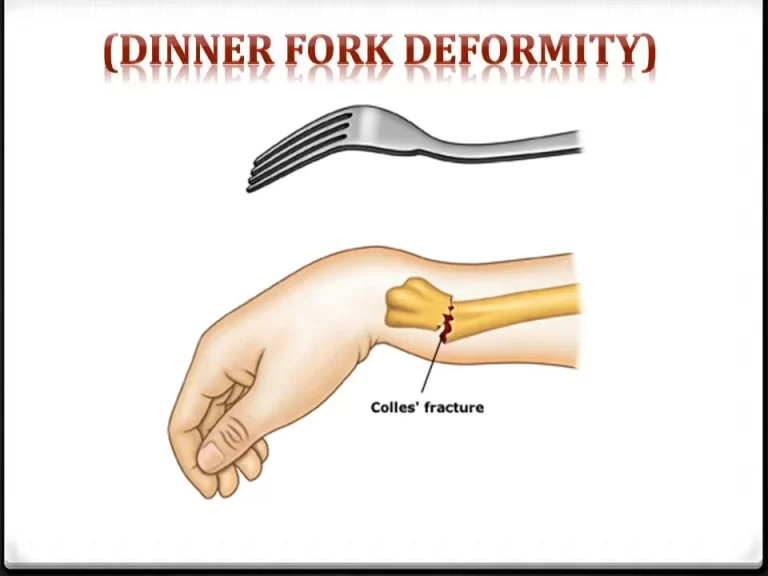
- Rocker bottom foot deformity
- Bony protrusions
- This stage can persist for up to a year if no treatment is administered.
Stage Two: Coalescence
In the first phase, the body tries to mend the damage caused. As the degradation of the bones and joints decelerates, there is a reduction in edema, redness, and warmth.
Stage Three: Reconstruction
This marks the concluding phase of the healing process for the foot’s joints and bones. Regrettably, they are unable to independently return to their original form or status. Even without additional injuries, the foot is frequently left in a distorted and unstable state.
Furthermore, the foot might be more prone to ulcers and sores, which can result in additional deformities or may necessitate amputation in some instances.
Causes of Charcot neuropathic osteoarthropathy
Patients with peripheral neuropathy from various conditions such as diabetes mellitus, leprosy, syphilis, poliomyelitis, chronic alcoholism, or syringomyelia may develop Charcot foot. When microtrauma occurs repeatedly and at a rate that surpasses the healing process, it can lead to fractures and dislocations. Alterations in circulation may lead to bone resorption, weakening of the bone, and increased susceptibility to fractures and dislocations.
- Individuals with diabetes who struggle to control their blood sugar (blood glucose) levels are at a higher risk of experiencing frequent occurrences of high blood sugar (hyperglycemia).
- Chronic hyperglycemia can lead to neuropathy (nerve damage), particularly affecting the lower legs and feet.
- This nerve damage results in diminished sensation and feeling in your affected foot.
- When you can’t perceive pain or other indicators that something is amiss with your foot or ankle, the likelihood of overlooking signs that require medical attention increases. Before you recognize that something is causing you pain, an easily treatable problem can grow into more serious conditions.
As an image, persons who have Charcot foot may lack the ability to sense pain that indicates damage to their bones, tendons, or ligaments, and as a result, they continue to walk on an injured foot. Ankle injuries that are usually minor, as well as bone fractures, can worsen significantly if you continue to walk on your foot without experiencing pain or being aware of the injury. That additional stress can lead to lasting changes in the shape of your foot and ankle over time.
In the same way, if you suffer from Charcot foot and are unable to perceive symptoms such as pain or warmth, it’s possible that you could overlook signs of an infection until it has resulted in serious complications.
Symptoms
At first, your foot and ankle may swell, redden, and feel warmer than usual. Later on, when fractures and dislocations happen, serious deformities may arise, such as the collapse of the midfoot arch (commonly known as rocker bottom foot) or instability in the ankle and hindfoot.
Early symptoms of Charcot foot include:

- Foot pain.
- Discoloration or redness.
- Swelling.
- A feeling of warmth or heat, especially when one foot is noticeably warmer than the other.
As a consequence of fractures and misalignment of the foot’s bones, the foot or ankle eventually develops a malformation.
- A rocker-bottom foot is a characteristic Charcot sign. This occurs when the bones located in the middle of the foot collapse. This leads to the collapse of the foot’s arch and a downward bend.
- Downward curling of the toes may occur.
- Protruding bones at odd inclinations can lead to foot ulcers and pressure sores.
- Because the feet lack sensation, these ulcers and sores can deepen or widen before they are noticed.
Additionally, high blood glucose levels hide the body’s ability to fight diseases. As a result, these foot sores could become infected. At the first sign of change in your feet, you should seek the advice of a doctor. If your doctor identifies Charcot foot early on, the chances of serious problems arising decrease.
In this section are instances of Charcot foot deformities that are more serious and have the potential to change the shape of your foot:
A rocker-bottom foot deformity
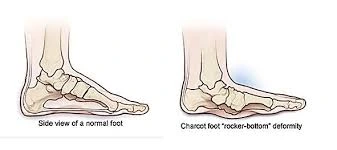
A rocker-bottom foot can occur as a result of the bones in the center of your foot collapsing and disintegrating. This results in the collapse of your foot’s arch. Instead of being naturally curved upward, a rocker’s foot is smoothed out. In the area where the arch used to be, you might notice a bulge in the middle of your foot.
- Changes in the shape of the toes: You may find your toes curling or curving under. If the bones and other tissues in your foot break or collapse, your toes will form a claw-like grip to help keep you stable.
- Alterations in the shape of the ankle: It is possible that one side of your ankle flexes or curls, causing it to look considerably less stable and straight in comparison to the other side.
- Foot ulcers: If Charcot foot causes changes in the shape of your ankle or foot, you may put undue pressure on specific areas of your foot. This can lead to open sores or ulcers, thereby increasing your risk of infection.
Diagnosis
Assessment
Clinical findings consist of erythema, edema, and high temperature in the affected joint. Neuropathic foot joints may demonstrate plantar ulcers. Since osteomyelitis and a Charcot joint can exhibit similar tagged WBC scan and MRI characteristics (such as joint destruction, dislocation, and edema), it is frequently hard to tell the two apart. A conclusive diagnosis might necessitate a biopsy of either the bone or synovial tissue.
A healthcare provider uses a physical examination and several imaging tests to diagnose Charcot foot. Inform your healthcare provider if you experience any symptoms, including pain, swelling, warmth, or loss of sensation in your feet, ankles, or toes.
Your doctor will check your feet and ankles. They will look at both of your feet and compare them to identify any differences. Your healthcare practitioner will evaluate your foot sensation level by touching your ankles, feet, and toes.
Your healthcare provider may use various tests to diagnose Charcot foot, including:
Foot X-Ray
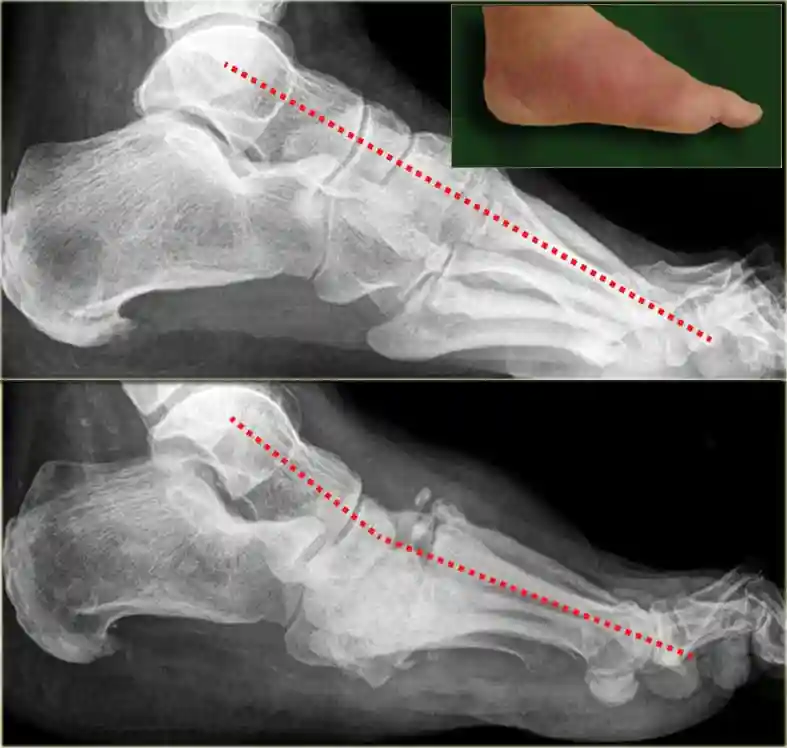
The primary initial imaging method for evaluating the foot in diabetes patients is radiography. They provide information regarding alignment, mineralization, and structure of bones; they are easy to obtain and not too expensive. A standard X-ray can display minor fractures and dislocations, or it may later show more evident fractures and subluxations.
In the future, the angle of the first metatarsal bone to the talus is fractured and the calcaneal inclination angle is reduced. Medial calcification of the arteries is included in most cases of Charcot foot, and this is a frequent secondary finding on radiographs. Nonetheless, the sensitivity of radiographic alterations of CN is generally low and they are delayed.
CT scan (computed tomography).
Because it can be likened to a 3D X-ray, a CT scan can provide an exceptionally detailed depiction of the bones. If your doctor believes you need surgery for Charcot foot, they will likely request a CT scan. The comprehensive CT scan could greatly facilitate the planning of the exact type of operation you need.
MRI (Magnetic resonance imaging).
X-rays can appear normal during the initial phases of active CN, but magnetic resonance imaging (MRI) allows for the identification of subtle changes. MRI mainly images protons in fat and water to provide a detailed view of anatomy and pathology in both soft tissue and bone. Due to its unique ability to differentiate tissues with high precision, MRI displays a high sensitivity and specificity for osteomyelitis. Consequently, it has become the favored method for assessing the complex feet of patients with diabetes. Although X-rays can provide a diagnosis, MRI is especially useful for identifying early Charcot bone and joint changes that are not yet visible on plain films.
Bone scan
A bone scan is one nuclear medicine test that can help determine whether a bone infection is present. There are various types of bone scans, and it is the physician’s responsibility to determine which one or ones are best suited for a particular problem. While these tests can still yield equivocal results, they are somewhat more effective than MRI at making a difference between a bone infection and Charcot. As part of a specialized test known as an indium scan, a marker is applied to white blood cells. Subsequently, these cells are monitored to see if they are moving toward the bone to fight an infection.
An indium scan will show noticeably high activity only in the case of an infection. However, both Charcot foot and bone infection lead to a positive result on a bone scan.
- Blood tests to look for indications of infection.
- Electromyography
- Nerve conduction velocity tests
- Nerve biopsy
Differential Diagnosis
- There have been reports of frequent misdiagnosis involving conditions like cellulitis, gout, deep-vein thrombosis (DVT), osteomyelitis, and even osteoarthritis. Clinicians should maintain a high level of suspicion for neuropathic patients who present in Charcot stage 0.
- Including Charcot foot in their differential diagnosis for patients with the classic red, hot, swollen foot may reduce the number of cases that go unnoticed. It is essential to highlight that patients often exhibit different levels of swelling, warmth, and redness. Even minor trauma should be taken seriously. In 22% of cases, Charcot Foot may also follow foot surgery events and injuries like ankle sprains.
Treatment
The most important part of Charcot foot treatment is to prevent severe complications. To prevent any problem or injuries from deteriorating (progressing), you need to cease walking on your foot. Your doctor will offer treatments to relieve your symptoms and reduce the long-term effects of Charcot foot on your foot’s functionality.
Medical Treatment
Diabetic Wound Care Management.
- Infected wounds necessitate antibiotic treatment in addition to wound maintenance until the inflammation is resolved.
- In the case of uncontrollable infections, it is advisable to use hospitalization, immobilization, and intravenous antibiotics.
In cases where the infection is linked with a deep abscess, widespread involvement of bones or joints, crepitus, considerable necrosis or gangrene, or necrotizing fasciitis, urgent surgery is warranted. They recommend that surgery for moderate to severe infections is likely to reduce the risk of serious amputation.
The main aim of Charcot foot treatment is to create a plantigrade foot that is ulcer-free, allowing the patient to walk comfortably in a commercially available diabetic shoe. To achieve this, treatment ensures that the foot is:
- Stable: The patient’s ankle and foot exhibit strength and shape suitable for bearing weight and walking without the risk of new deformities.
- Plantigrade: The feet can lie flat on the surface as understood. To understand this concept, envision the foot as a three-legged stool consisting of the big toe, little toe, and heel. A foot is classified as plantigrade if, while normally standing, all three of the following points touch the ground.
- Braceable: Utilizing shoe inserts and braces to stabilize the foot and maintain a plantigrade position can likely prevent deformities and ulcers, even if the foot itself is not in a normal position.
- Ulcers free: The primary aim of Charcot treatment is to prevent ulcers from occurring. By preventing ulcers, you might be able to avoid infections and probable amputations. To prevent ulcers, it is essential to avoid or address bony prominences that lie beneath the skin. Along with helping the patient to walk normally, the therapy goals mentioned earlier can be viewed as methods for lowering the risk of ulcer development.
Nonsurgical Treatment
Immobilization
Your healthcare practitioner will require you to wear a complete contact cast. This will result in limited movement of your foot and ankle. To avoid putting any weight on your foot, you will likely need to use a wheelchair, crutches, or a knee-walker. Once the swelling goes down, your foot will be fitted with new casts. The healing process can take several months or even longer.
Casting
In the initial stages of Charcot, a cast or specialized boot is commonly employed to safeguard the foot and ankle. Castings serve to stabilize the bones during healing and prevent the emergence of additional abnormalities. A cast does an excellent job of protecting bones and reducing edema.
The most commonly used cast for Charcot foot is known as a “total contact cast.” This encases the whole foot and has many similarities to conventional casts. While wearing a cast, the patient must avoid putting weight on the foot until the bones have had sufficient time to heal. Usually, a wheelchair, knee scooter, or crutches are needed. At times, the healing process can take three months or even longer.
To ensure that the cast remains on the leg while the swelling decreases and to prevent ulcer formation, it is often replaced every one or two weeks.
Once the edema has subsided, patients are occasionally transitioned to an expert heavy-duty boot that covers the entire foot and can be detached. By replacing the cast with a boot, one can walk and remove it for foot inspection and cleaning—this is the characteristic that makes the switch advantageous. The final aim is to go back to wearing normal shoes.
Taking weight off your foot
To minimize swelling and prevent further injuries such as bone fractures, it is important to lessen pressure and weight on your injured foot. You may require:
- A cast or brace.
- Crutches.
- A walker.
- A wheelchair.
Orthotics and footwear changes

Shoe inserts called orthotics help keep your toes in the correct position and provide support for your feet. An ankle brace or custom-made insoles may be essential for you. Your healthcare provider may recommend orthotics or custom-made shoes with greater depth to alleviate extra strain on your feet and provide support while walking.
Changes in activity: The possibility always exists that Charcot foot may recur or affect your other foot. To protect your feet, your provider may recommend modifying your activities, like reducing the amount of time you spend standing or walking. You may need to cut down on activities involving your feet by using a wheelchair.
Surgical Treatment
When casting and custom footwear are insufficient to achieve the previously mentioned Charcot therapy objectives, surgery may be the most effective option.
Surgery may be suggested if the abnormalities hide your ability to walk normally or raise your risk of developing ulcers. Healing unstable fractures and dislocations also requires surgery.
Several surgical options for the various problems that Charcot can cause are outlined below. These procedures are often performed together to meet the individual needs of each patient.
Debridement of ulcers.
Surgery may be necessary to help ulcers heal. Debridement consists only of cleaning the ulcer and removing any non-healing dead skin. Once debridement has been performed, a cast can be put on to ease pressure on the ulcer as it heals.
Lengthening the calf muscle or Achilles tendon.
The Achilles tendon or calf muscle may be tight, but this is not always due to an injury. This constriction can lead to ulcers due to the formation of pressure points on the sole, especially at the ball or front part of the foot. Strengthening the calf or Achilles muscles can help reduce this pressure.
Removal of bony prominences (Exostectomy).
Deformities can lead to prominent bones appearing beneath the skin, and these bones can exert pressure on the skin, causing ulcers to form. The easiest way to prevent an ulcer from forming due to a bony prominence is to remove the bone fragment. Ulcers are especially likely to develop on the inside and bottom of the foot because of prominences.
Charcot deformity correction.

When fractures and dislocations are unstable or the bones are clearly misaligned, plates, screws, and/or rods might be necessary to rectify abnormalities and ensure the bones heal correctly. Due to the low quality of bone, fractures in diabetics are typically more complex.
Consequently, the procedures needed to rectify them usually necessitate more hardware (plates and screws) than those for individuals without diabetes. Should any of these procedures be performed, bone graft material may be utilized to assist in the healing of bone.
An arthrodesis, or joint fusion, is a procedure that can help dislocated bones heal into a single, solid piece of bone. Joint fusions are an effective method for reversing deformity and improving stability, making them a key part of Charcot treatment.
- In cases of acute fractures without significant joint dislocations, it may be sufficient to heal the shattered bones through open reduction and internal fixation.
- A substantial rod may need to be inserted into the ankle to maintain stability in cases of severe abnormalities, particularly those involving the heel or ankle.
Amputation. In severe cases of Charcot arthropathy, particularly those complicated by significant deformity, deep bone infection, or lack of blood circulation to the foot, it may not be possible to save all or part of the foot. To assist the patient in maintaining mobility given these conditions, the physician may recommend an amputation above the level of the disease, followed by fitting for a prosthetic device.
Surgical Outcomes
- In comparison to conventional treatment for foot and ankle fractures, surgical intervention for a Charcot foot involves a greater risk of wound complications, infections, and amputation, due to the effects of underlying diabetes and the significant deformities that are often present. The strategies that most effectively reduce risks are:
- Control blood sugar levels, as the patient’s hemoglobin A1C level is directly related to the risk of complications.
- Post-surgery, do not put weight on your foot until the doctor has cleared you to do so.
Though there is a considerable risk involved with surgery of complications, the likelihood of adverse outcomes is often greater for Charcot foot that goes untreated. As an example, in cases where surgery is necessary to correct abnormalities and avert ulcers, the procedure usually justifies the risk, given that Charcot patients with ulcers face a 50% chance of limb amputation.
If surgery is done before an ulcer develops, the chances of success are quite high (generally exceeding 80%). However, surgery becomes significantly more challenging with the presence of an ulcer, primarily because of the increased risk of infection. After the operation, it is generally necessary to keep the foot immobile for at least three months.
Complications arising from prematurely placing weight on the foot and ignoring the physician’s recommendations include:
- Difficulty healing the incisions
- New injuries
- Return or even worsening of the deformity
Prevention
The best way to protect yourself from Charcot foot is to manage your diabetes and overall health effectively. Maintaining your blood sugar at a proper level can help you reduce your chances of developing neuropathy and avoid hyperglycemia. Ask your doctor how often you should have your feet checked. Inquire whether you should see a podiatrist, a foot and ankle orthopedist, or another foot care specialist.
Furthermore, you can reduce the likelihood of developing Charcot foot and other diabetes-related foot problems by:
- Examining your feet daily for any alterations. Don’t forget to watch your toes. If needed, utilize a mirror or request help.
- Getting your feet checked whenever you consult a medical professional.
- Maintaining the filing and trimming of your toenails. To prevent ingrown toenails, trim them straight across.
- Keep your feet’s blood flowing. While sitting, keep your feet and wiggle your toes often.
- Wearing shoes (or slippers) and socks throughout the day. Check that your shoes fit properly and that your socks aren’t overly tight.
- Washing feet daily. Ensure they are entirely dry, even between your toes. Lotion ought to be applied to the tops and bottoms of the feet, avoiding application between the toes.
Risk factors
Charcot foot nearly always affects individuals with diabetes. For individuals with diabetes for over seven years, the likelihood of developing neuropathy increases with frequent smoking and alcohol consumption.
Moreover, the presence of diabetes and other health conditions raises your likelihood of developing neuropathy. These illnesses include:
- High blood pressure (hypertension).
- Obesity (overweight).
- High cholesterol.
- Kidney disease.
Prognosis
If a healthcare professional identifies Charcot foot at an early stage, they should be able to avert the important effects. Regular follow-up sessions with your provider will be necessary. They will take further X-rays of your feet to look for any changes or new symptoms.
If Charcot foot causes considerable symptoms or problem, you might have to use mobility aids or discover new methods of walking and moving. You can find out more about what to expect from your doctor. They will assist you along the journey and be on hand to respond to any queries you might have.
Complications
- Foot deformities including flatfoot, rocker-bottom foot, hammertoes, and ankle equines contracture.
- Bony prominences that may result in ulceration, infection, and in certain instances, amputation or death.
- Charcot joint recurrence
- Upon the initial diagnosis of acute Charcot, the 5-year mortality rate is 13%, comparable to that of diabetics who do not have Charcot.
Conclusion
The best method for treating diabetic foot problems is prevention. Important preventative factors include:
- Control of blood glucose levels
- Inspect your feet daily to ensure that no cuts or ulcers are developing.
- To prevent cuts and injuries, it is also essential to wear shoes that provide full coverage, are robust, and offer support.
For further recommendations regarding foot care for diabetics, refer to: Taking Care of Diabetic Foot. If you notice any alterations in the appearance of the foot, like swelling, redness, warmth, or a sore, consult your doctor immediately. Charcot arthropathy should be recognized and treated as soon as possible to improve the prognosis.
Once Charcot is diagnosed, it is essential to allow the bones to heal in a stable posture that minimizes the risk of ulcers as part of the treatment. While surgery is often the most effective way to prevent serious deformities and ulcers, it can sometimes be avoided while still achieving the same result.
To ensure the best possible treatment outcome:
- Concerning the timing of when it is safe to put weight on the injured foot, the patient should follow the doctor’s instructions.
- Patients must dedicate themselves to daily monitoring of their blood sugar levels and foot examinations throughout their lives.
- Both of these behaviors are essential for the early identification of Charcot foot and the prevention of long-term problems.
FAQs
What is the reason that a delay between the appearance of symptoms and the diagnosis of Charcot foot is common?
Charcot foot manifests initially with non-specific signs that are often observed in other, more prevalent conditions like infections and rheumatologic disorders. A lot of patients either do not experience pain or have pain that is due to pre-existing neuropathy. Doctors who do not specialize in orthopedic foot and ankle problems may encounter a Charcot foot only a handful of times throughout their careers, which is less often than they encounter other conditions such as septic arthritis, gout, rheumatoid arthritis, and other inflammatory arthropathies.
Does the prognosis worsen if there is a delay between the appearance of signs and diagnosis?
Not a requirement. In some instances of Charcot arthropathy, instability develops in the initial stages, and the condition has already become destabilized before the patient’s consultation with a physician. Even with early protection of the foot and ankle, other cases may still destabilize. For some patients, early protection may aid in reducing the risk of further instability; however, instability can still arise even with early protection. Instability due to massive bony fragmentation may manifest quite differently than in a fracture caused by trauma in a non-neuropathic patient.
Which complications are associated with Charcot arthropathy?
Complications Deformities of the foot, including flatfoot, rocker-bottom foot, hammertoes, and equines contracture of the ankle.
Bony prominences that may result in ulceration, infection, and in certain instances, amputation or death.
Which treatment for neuropathy has the greatest success?
Neuropathy symptoms may be treated with tricyclic antidepressants, anti-seizure medications, or electrical stimulation. Physical therapy can assist in managing neuropathy and enhancing mobility.
What are the four stages of Charcot’s disease?
Charcot foot consists of four distinct disease stages, akin to active and inactive phases: inflammation, fragmentation, coalescence, and consolidation. Typically, the illness is confined to one run through these various stages of disease.
Is it possible to cure Charcot?
Early evaluation and treatment can avert lasting harm. It is possible to recover completely from Charcot foot and prevent its recurrence by managing other aspects of your health, such as controlling blood sugar levels and maintaining a healthy weight.
What is the latest therapy for neuropathy?
Transcutaneous electrical nerve stimulation (TENS) is a non-invasive therapy that employs a device to provide low-intensity electrical currents to the surface of the skin. The goal of TENS is to disrupt pain signals, enhance endorphin release, and boost blood circulation to ease neuropathic pain.
Does Charcot cause pain?
Charcot foot, known as Charcot arthropathy, is a condition that affects the bones, joints, and soft tissues in your feet. At the outset, you might not notice that something is amiss. However, in the long run, it can lead to painful sores or alter the shape of your foot.
Does Charcot count as a disability?
A Charcot foot can result in serious disability and, in certain instances, amputation as the foot becomes progressively more deformed. Individuals exhibiting signs of Charcot foot should pursue medical care immediately. Patients with early diagnosis and treatment can achieve more successful outcomes than those with advanced deformity.
Reference
- Petrova, N., & Edmonds, M. (2015). Acute Charcot neuro‐osteoarthropathy. Diabetes/Metabolism Research and Reviews, 32(S1), 281–286. https://doi.org/10.1002/dmrr.2734
- Marks, R. M. & Medical College of Wisconsin. (n.d.). Charcot neuroarthropathy (Neuropathic arthropathy). https://www.mcw.edu/-/media/MCW/Departments/Orthopaedic-Surgery/Foot-and-Ankle-Patient-Education-Charcot-Neuroarthropathy.pdf
- Charcot arthropathy (Neuroarthropathy) symptoms & causes. (n.d.-b). FootCareMD. https://www.footcaremd.org/conditions-treatments/the-diabetic-foot/charcot-arthropathy
- Harris, A., & Violand, M. (2023, May 8). Charcot neuropathic osteoarthropathy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470164/
- Holmes, C., Schmidt, B., Munson, M., & Wrobel, J. S. (2015). Charcot stage 0: A review and considerations for making the correct diagnosis early. Clinical Diabetes and Endocrinology, 1(1). https://doi.org/10.1186/s40842-015-0018-0
- Wikipedia contributors. (2025a, January 10). Neuropathic arthropathy. Wikipedia. https://en.wikipedia.org/wiki/Neuropathic_arthropathy