Pusher Syndrome
What is a Pusher Syndrome?
Pusher Syndrome, also known as controversial pushing, is a neurological condition often observed in patients who have experienced a stroke or brain injury, particularly those affecting the right hemisphere.
Patricia Davies originally discussed this in 1985. It is typically seen after a stroke and is frequently accompanied by severe inattention and chemosensory impairments. The literature reports varying incidence rates of this disease following stroke, ranging from around 5–10% to 63%.
Pathology
The origins and symptoms of Pusher Syndrome are being studied more thoroughly, although the presentation is still unclear. According to some theories, pusher behavior might arise from a high-order interruption of somatosensory information processing from the paretic hemi-body, or it could be the result of a conflict.
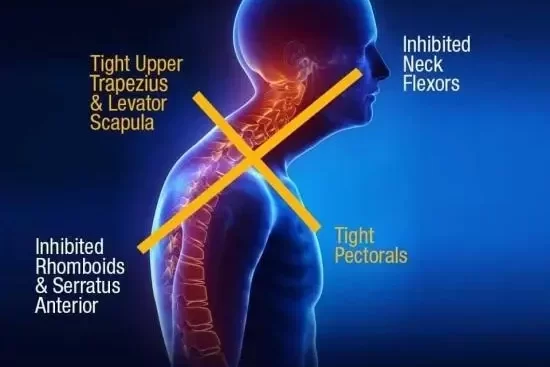
Pusher syndrome patients may also experience motor impairments, poor proprioception, primary visual abnormalities, or visual perception issues. These conditions make it more difficult for them to regain balance and posture.
According to a number of earlier research, individuals with right brain injury were more likely than those with left brain damage to exhibit pusher behavior. Additionally, Abe et al. Three key factors should be considered when diagnosing pusher behavior.
Signs and Symptoms
Patients who behave like pushers may require lengthier rehabilitation.
Additionally, when it comes to subjective visual verticals, individuals don’t appear to exhibit any abnormal vestibular or visual processing. When the patient is upright and unable to support their body weight on the weaker lower extremity, the push manifests as a powerful lateral lean toward the affected side, making the patient extremely unstable.
Some earlier hypotheses argue that pusher syndrome develops as a result of neglect, and the terms “pusher syndrome” and “hemispatial neglect” are occasionally used interchangeably. Contrary to popular belief, hemispatial neglect is mostly associated with right hemisphere injuries; nevertheless, different research found that pusher syndrome can also develop in individuals with left hemisphere lesions, resulting in aphasia.
Karnath combines these two opposing viewpoints and concludes that there is a strong correlation between pusher syndrome and both aphasia and neglect. This correlation may be caused by the closeness of important brain areas linked to the two diseases. The essay continues, nevertheless, by emphasizing how important it is to understand that pusher syndrome is not primarily caused by aphasia or neglect.
Clinical Presentation
- affected side limbs in a flexed posture
- Position of the unaffected side limbs extended
- opposition to any efforts at correction
- Left brain damage combined with spatial aphasia.
Differential Diagnosis
Because it stresses moving the non-hemiparetic extremities towards the contralateral side of the brain lesion, the phrase “controversies pushing” is unique in this respect. Furthermore, the hemiparetic patient without pushing syndrome exhibits tugging rather than pushing when he or she recognizes they have lost their balance and seeks to grip onto anything with their non-paretic hand.
Diagnostic Procedures
Three diagnostic variables for Pusher Syndrome are identified by Karnath and Broetz and are displayed below:
- Spontaneous Body Posture (severe, moderate, and mild)
- It is necessary to check the patient for contralateral tilting based on their initial posture, which should preferably be supine to sit or sit to stand, right after a positional shift. This may be observed falling to the side opposite the brain lesion or not.
- Capture and Expansion of the Nonparetic Limbs
- Reluctance to Accept Passive Adjustment of Slanted Posture
- When a therapist uses physical interventions to modify their body posture, patients usually aggressively resist.
Pusher Syndrome may be quickly and easily identified by doctors using the SCP, which can be applied in both acute and rehabilitative settings.
Treatment of Pusher Syndrome
Giving the patient visual input on their changed body position is the first aim of beginning therapy, according to Karnath and Broetz. Patients can sense whether they are in an erect posture when they perceive that they are inclined because they are given visual information about their surroundings.
Patients should be questioned about their ability to see if they are upright when in various postural configurations. They should also be provided visual cues and references to assist them orient themselves upright as well as feedback regarding their body alignment.
It is envisaged that with consistent therapy, individuals with Pusher Syndrome would be able to use training techniques independently and make use of their surroundings to obtain visual input from vertical structures, even if they may initially require urging when using visual feedback.
Based on their clinical experience, Karnath and Broetz proposed that the following therapy sequence might be useful in treating Pusher Syndrome:
- Give the patient the opportunity to visually investigate their surroundings, the body’s connection to those surroundings, and whether or not they are orientated upright. The therapist’s arm or a variety of vertical objects.
- keeping an upright body posture while carrying out functional tasks.
More modern therapies advise:
- Acquire the skills required to place your body vertically.
Additional treatment techniques that have been discovered to be effective recently include standing frames, robot-assisted gait training, lateral stepping with body weight-supported treadmill training, interactive visual feedback training, and mirror visual feedback training.
When treating these individuals, physical therapists concentrate on motor learning techniques. Weight shifting, verbal signals, regular feedback, and practicing proper orientation are all useful techniques for lessening the consequences of this illness. One potential treatment for pusher behavior is to have the patient sit with their stronger side against a wall and tell them to lean that way.
Treatment is arranged so that patients may become aware of their changed perception of the vertical, learn the motions required to achieve optimal vertical position, use visual aids for feedback regarding body orientation, and maintain vertical body position while engaging in other activities.
Prognosis
According to some writers, Pusher Syndrome is infrequently observed six months after a stroke and has been proven to have no detrimental effects on the patient’s final functional result, however, it can cause a three-week delay in rehabilitation. However, according to a case study by Santos-Pontelli et al., three patients had Pusher Syndrome that persisted for up to two years after a stroke, severely impairing their functional capacities.
To see if it affected the degree of recovery. Based on their research, they hypothesized that 90.5% of patients with just a motor presentation might “recover” from Pusher Syndrome in 27 days, scoring 0 or 1 on the Burke Lateropulsion Scale. In around 59% of cases, the patients who had two deficiencies met the aim.
FAQs
How may pusher syndrome be resolved?
These experts will assist in assessing the severity of symptoms and offer practical recommendations for supporting survivors in keeping an upright posture while sitting, standing, and moving around.
What pusher syndrome mechanism exists?
A clinical condition known as “pusher syndrome” that develops after left or right brain injury causes patients to deliberately push away from their nonhemiparetic side, impairing their postural balance. It is only lately that the mechanism behind this condition and the anatomy associated with it have been discovered.
What differentiates Wallenberg syndrome from pusher syndrome?
Usually, individuals with medulla-related infarctions have Wallenberg’s syndrome. They have an SVV (subjective visual vertical) tilt.
How often does pusher syndrome occur?
Lateropulsion, often known as pusher syndrome (PS), is a frequent disability following a stroke. Patients with it typically push forcefully toward their hemiparetic side and show resistance to the body’s passive adjustment to a vertical upright position. According to a recent survey, 41% of stroke victims had PS.
What is the pusher’s purpose?
With them, you may handle extra activities once events are sent and change, filter, and adjust them without having to maintain your own infrastructure.
References
- Wikipedia contributors. (2024, January 19). Pusher syndrome. Wikipedia. https://en.wikipedia.org/wiki/Pusher_syndrome
- Pontelli, T. E. G. D. S., Pontes-Neto, O. M., Colafêmina, J. F., De Araújo, D. B., Santos, A. C., & Leite, J. P. (2005). Posture control in Pusher syndrome: influence of lateral semicircular canals. Brazilian Journal of Otorhinolaryngology, 71(4), 448–452. https://doi.org/10.1016/s1808-8694(15)31197-6